Lower-income populations are hit harder by the diabetes epidemic as regards both prevalence and the risk of complications. Food Insecurity is one of the mechanisms through which poverty may predispose people with low socio-economic status to poorer control and higher complication rates. The United Nations Food and Agriculture Organization defined food security as “the right to have access to sufficient nutritional and culturally acceptable food choices.” Adults suffering from diabetes with limited income have a 40% greater chance of having food insecurity and an inadequate blood glucose control. Such patients have a two-fold greater risk of developing severe hypoglycemia. In addition, several studies have shown that social vulnerability resulting from food insecurity, low socioeconomic status, low educational levels, and poor health education is an independent risk factor for hypoglycemia, even after conventional predictors are controlled. This review analyzes the literature available on social vulnerability as a non-conventional risk factor for development of hypoglycemia in diabetic subjects.
La epidemia de diabetes afecta de manera especial a las poblaciones de menores ingresos, aumentando no solo su prevalencia sino también el riesgo de complicaciones. Entre los mecanismos por los cuales la pobreza podría predisponer a las personas de bajo nivel socioeconómico a un mal control de su enfermedad, se encuentra la inseguridad alimentaria. La seguridad alimentaria es definida por la Organización de Naciones Unidas para la Alimentación y la Agricultura como “el derecho de todas las personas a tener una alimentación cultural y nutricionalmente adecuada y suficiente”. Los adultos con diabetes que no cuentan con suficientes ingresos para llevar una dieta saludable tienen una probabilidad un 40% mayor de presentar un control glucémico inadecuado. Estos pacientes tienen además un riesgo al menos dos veces mayor de presentar hipoglucemias severas. Según los estudios publicados hasta la fecha, la vulnerabilidad social que representa la inseguridad alimentaria, el bajo nivel socioeconómico, el bajo nivel de instrucción y la pobre educación sanitaria, ha demostrado ser un factor de riesgo independiente para hipoglucemia, aun después de controlar los predictores convencionales. El objetivo de este artículo es analizar la literatura existente sobre vulnerabilidad social como factor de riesgo no convencional de hipoglucemia.
It is estimated that approximately 415 million people worldwide suffer from diabetes, 77% of them, live in low-medium income countries.1 The prevalence of diabetes in Argentina is 9.8%, being greater in lower-income than in higher-income groups (10.3% vs 7.3%).2 Lower-income populations are hit harder by the diabetes epidemic, not only in prevalence but also on the risk of complications.3–5 Food Insecurity is one of the mechanisms by which poverty may predispose people with low socio-economic status to worse control and higher rates of complications. In 1974 the United Nations Food and Agriculture Organization (FAO) defined food security as “the right to have access to sufficient nutritional and culturally acceptable food choices.”6 According to the latest data from the Social Debt Observatory of the Argentine Catholic University (Observatorio de la Deuda Social Argentina (ODSA), Universidad Católica Argentina, UCA), which analyzed over a period of five years (2010–2014) reported that more than 1 out of 10 households are at risk of suffering from nutritional problems due to economic reasons. In 2014 the prevalence of food insecurity among households located in the country's main urban centers was 13.8%.7 Since the 2000s, the association between food insecurity and chronic diseases such as type 2 diabetes in households is well described, and is 50% higher compared to households with food security.8 Adults suffering from diabetes with limited income have 40% greater chance of having food insecurity and an inadequate glycemic control. In such patients, the risk of developing severe hypoglycemia is twice greater.9 In addition, several studies have shown that social vulnerability resulting from food insecurity, low socioeconomic status, low schooling and poor sanitary education is an independent risk factor for hypoglycemia, even after conventional predictors are controlled.10 In fact, low socioeconomic status confers a risk of hypoglycemia similar to that attributed to insulin use.11
The global frequency of hypoglycemia varies considerably among studies, being greater in patients with type 1 diabetes (T1D) than in patients with type 2 diabetes (T2D).12–14 In the Diabetes Control and Complications Trial (DCCT), patients in the intensive arm had a 65% incidence of severe hypoglycemia, compared with 35% in the conventional group. In the UK Diabetes Prospective Study, the rates of major hypoglycemic episodes were 0.7% in the conventional group, 1.4% in the glibenclamide group, and 1.8% in the group treated with insulin.12 Conventional risk factors for hypoglycemia are related to absolute or relative insulin excess due to excessive doses of antidiabetic medication, skipping meals, physical exercise, alcohol intake, and kidney failure, among others.15 These factors, however, account for a minority of cases of severe hypoglycemia, of which, asymptomatic hypoglycemia is a result of defective counterregulation and strict glycemic control.15–17 Little is known about non-conventional risk factors such as the role of social vulnerability as a cause of hypoglycemia in patients with diabetes. Therefore, this review analyzes the existing literature on social vulnerability as a non-conventional risk factor for the development of hypoglycemia in diabetic individuals.
Material and methodsA systematic search was carried out from 1991 to 2015 on peer review manuscripts listed in PubMed, MedLine, Cochrane Library and LILACS using the following search terms: hypoglycemia risk factors, hypoglycemia and food insecurity, hypoglycemia, socioeconomic level, level of income, unemployment, work, hunger and food insecurity. The search was limited to articles published in English literature in human adults. The exclusion criteria included studies of patients under the age of 15 years and gestational diabetes, case reports, letters, and book chapters.
A total of 81 titles and abstracts from the electronic search were reviewed. After applying exclusion and inclusion criteria, 17 articles were selected (1 systematic review, 3 prospective, 4 retrospective, 5 cross-sectional, 1 cohort, 1 case-control, and 2 post hoc studies).
Hypoglycemia and social vulnerabilitySocial vulnerability is defined as the reduced ability or inability of a person or groups of people to respond to (in the sense of cope with, recover from, or adapt to) any external stresses or pressures placed on their livelihoods and well-being.18 The degree of vulnerability of individuals, groups of people or communities depends on a number of factors, ranging from individual demographic (age, gender, level of education) and household characteristics (household composition, lifecycle, socio-economic and occupational status, poverty situation) to macro-indicators (development level, economic and social contexts).18 The concurrence of social vulnerability factors and health problems puts people in a particular situation that deserves special attention.
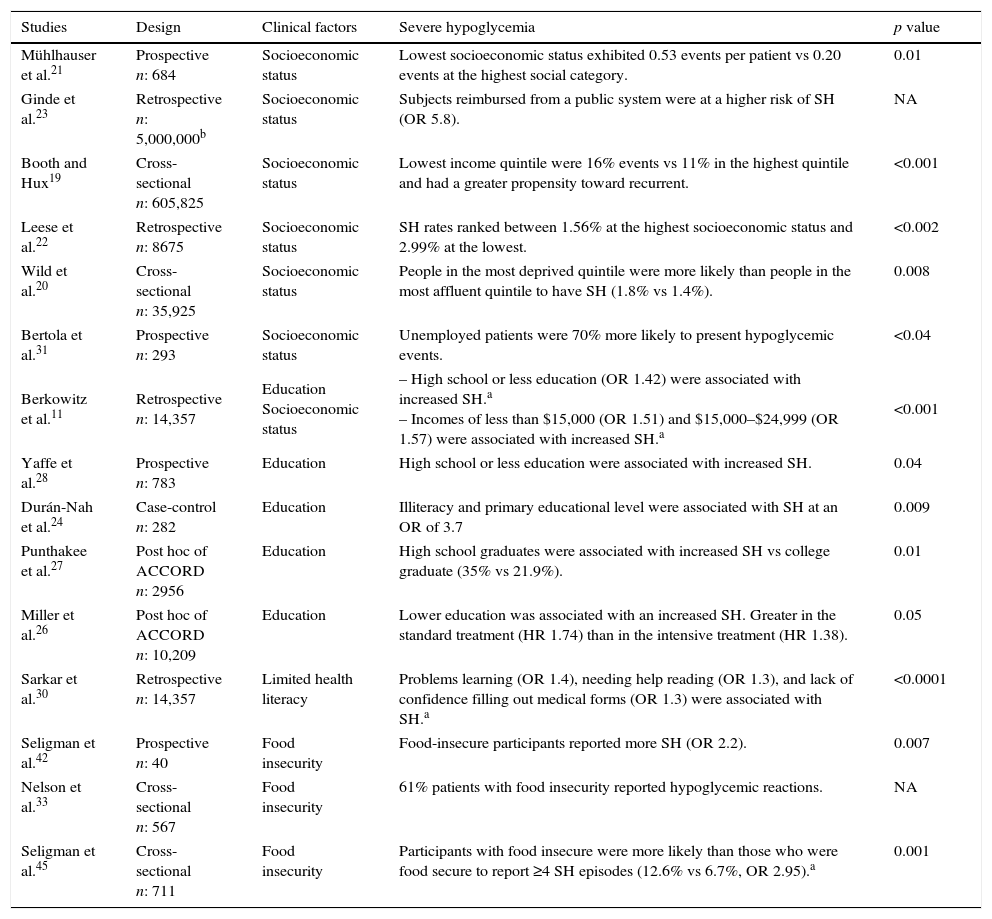
In this context, there are few studies evaluating the influence of social vulnerability factors on the incidence of hypoglycemia in diabetic patients (Table 1), and most of these studies are of limited methodological quality. These studies demonstrate that social vulnerability factors, such as low socio-economic status, poor sanitary education, and food insecurity, behave as independent risk factors for hypoglycemia, even after adjusting for demographic and clinical factors, which are known to cause hypoglycemia.10
Studies evaluating hypoglycemia and social vulnerabilities.
| Studies | Design | Clinical factors | Severe hypoglycemia | p value |
|---|---|---|---|---|
| Mühlhauser et al.21 | Prospective n: 684 | Socioeconomic status | Lowest socioeconomic status exhibited 0.53 events per patient vs 0.20 events at the highest social category. | 0.01 |
| Ginde et al.23 | Retrospective n: 5,000,000b | Socioeconomic status | Subjects reimbursed from a public system were at a higher risk of SH (OR 5.8). | NA |
| Booth and Hux19 | Cross-sectional n: 605,825 | Socioeconomic status | Lowest income quintile were 16% events vs 11% in the highest quintile and had a greater propensity toward recurrent. | <0.001 |
| Leese et al.22 | Retrospective n: 8675 | Socioeconomic status | SH rates ranked between 1.56% at the highest socioeconomic status and 2.99% at the lowest. | <0.002 |
| Wild et al.20 | Cross-sectional n: 35,925 | Socioeconomic status | People in the most deprived quintile were more likely than people in the most affluent quintile to have SH (1.8% vs 1.4%). | 0.008 |
| Bertola et al.31 | Prospective n: 293 | Socioeconomic status | Unemployed patients were 70% more likely to present hypoglycemic events. | <0.04 |
| Berkowitz et al.11 | Retrospective n: 14,357 | Education Socioeconomic status | – High school or less education (OR 1.42) were associated with increased SH.a – Incomes of less than $15,000 (OR 1.51) and $15,000–$24,999 (OR 1.57) were associated with increased SH.a | <0.001 |
| Yaffe et al.28 | Prospective n: 783 | Education | High school or less education were associated with increased SH. | 0.04 |
| Durán-Nah et al.24 | Case-control n: 282 | Education | Illiteracy and primary educational level were associated with SH at an OR of 3.7 | 0.009 |
| Punthakee et al.27 | Post hoc of ACCORD n: 2956 | Education | High school graduates were associated with increased SH vs college graduate (35% vs 21.9%). | 0.01 |
| Miller et al.26 | Post hoc of ACCORD n: 10,209 | Education | Lower education was associated with an increased SH. Greater in the standard treatment (HR 1.74) than in the intensive treatment (HR 1.38). | 0.05 |
| Sarkar et al.30 | Retrospective n: 14,357 | Limited health literacy | Problems learning (OR 1.4), needing help reading (OR 1.3), and lack of confidence filling out medical forms (OR 1.3) were associated with SH.a | <0.0001 |
| Seligman et al.42 | Prospective n: 40 | Food insecurity | Food-insecure participants reported more SH (OR 2.2). | 0.007 |
| Nelson et al.33 | Cross-sectional n: 567 | Food insecurity | 61% patients with food insecurity reported hypoglycemic reactions. | NA |
| Seligman et al.45 | Cross-sectional n: 711 | Food insecurity | Participants with food insecure were more likely than those who were food secure to report ≥4 SH episodes (12.6% vs 6.7%, OR 2.95).a | 0.001 |
NA: data not available; SH: severe hypoglycemia.
Among the studies evaluating the relationship between low socio-economic status and hypoglycemia risk, one of most important was the DISTANCE study conducted in T2D patients from different ethnicities.11 This cross-sectional analysis of a 14,357-patient database revealed that low-income patients have a greater prevalence of episodes of hypoglycemia compared to high-income patients (16% vs 8.8%; p<0.001). In a multivariate analysis, patients with yearly income less than $15,000 had an odds ratio (OR) of 1.42 (CI 1.19–1.91), and those with income between $15,000 and $24,999 had an OR of 1.51 (CI 1.27–1.94). These results indicate that low socioeconomic status confers a higher risk of hypoglycemia comparable to that associated with the use of insulin (OR 1.44; CI 1.19–1.74).11 This study, however failed to assess the role of vulnerability, which is food insecurity and its possible association with hypoglycemia.
Several well-controlled studies have also demonstrated the association between social vulnerability and hypoglycemia.19–24 Mühlhauser et al., reported in a prospective study in patients with T1D, that a lower social status (determined by the level of education attained, employment status, and yearly economic income) had an increased risk for severe hypoglycemia. The authors suggested that patients of a higher socio-economic status have a better chance of preventing, recognizing and treating hypoglycemic events, since they have a greater knowledge of the outpatient management of insulin therapy and self-monitoring. In the study published by Leese et al.22 that included patients with T1D and T2D, a retrospective evaluation was carried out of the prevalence of assistance to diabetic patients for severe hypoglycemia in the emergency room and an association between low socioeconomic status and severe hypoglycemia was found. In another study,23 five million emergency department visits for hypo and hyperglycemic complications over 12 years were retrospectively evaluated and it was found that the consultation rates (per 1000 patients) for patients with public health insurance were more than double for patients with private health insurance or patients who paid out of their own pocket. The main predictor factor for emergency room consultation was the absence of consultation with a physician during the previous year (OR 2.01).
Socially vulnerable populations often have limited access to most up-to-date therapeutic options and generally get their medications through state programs that include drugs as sulfonylureas, glinides and human insulin. This, in turn, renders them even more vulnerable to hypoglycemia.25 This suggests that a low socioeconomic status is an important factor that limits the ability of people with diabetes to have access to resources and safer management of their disease.
Hypoglycemia and education levelLimited data is available on the association between education level and the risk of hypoglycemia in patients with diabetes. Two post-hoc analyses from the ACCORD study showed that less than high school education was associated with a higher risk of severe hypoglycemia compared with higher level and graduate education, irrespective of the branch of treatment assigned (standard or intensive).26,27 Berkowitz et al.11 also reported that the education level is an important risk factor for hypoglycemia. In this study, patients with a lower level of education were found to have a higher prevalence of severe hypoglycemic events compared with those who have a higher level (11.9% vs 8.9%; p<0.001). The multivariate analysis showed that patients with less than high school education had an OR of 1.57 for hypoglycemia compared to individuals with higher education. Similarly, a 12-year prospective study that evaluated hypoglycemia risk in patients with cognitive dysfunction and dementia reported that less than high school education was significantly related to a greater risk of severe hypoglycemia.28 This association also holds true in patients with very low education level.29 A case-control study reported that a group of patients with illiteracy or primary educational level had a risk of severe hypoglycemia nearly four times greater than that of patients with a higher educational level.24
Hypoglycemia and limited health literacyThe relationship between health literacy and hypoglycemia risk has not been determined. In the DISTANCE study,30 factors that entailed greater risk of hypoglycemia were insulin use, presence of learning problems, and inability to read or fill out a health form unassisted. After multivariate adjustment, the latter three factors were independently associated with a 30–40% greater risk of severe hypoglycemia. The authors indicated that limited health literacy poses an obstacle to self-managing treatment regimens due to a poor understanding of instructions concerning both medication doses and precautions to bear in mind, which may lead to an increased risk of severe hypoglycemia.
Unemployment and mild hypoglycemia riskLittle evidence is available between socioeconomic status and the risk of hypoglycemia in individuals with diabetes. A prospective study conducted at a public hospital in the city of Córdoba, Argentina reported a prevalence of 38.9% of hypoglycemia in patients with T1D and T2D.31 Of them, 46% of patients were unemployed and such patients had a 70% greater risk of hypoglycemia compared to employed patients. The most frequent risk factor was food intake omission (57%), which suggests that a limitation of food budgets may play a role in the incidence of hypoglycemic episodes.31
Hypoglycemia and food insecurityAt present, many countries are facing economic crises and a large number of people are losing their jobs or have insufficient incomes to maintain an adequate treatment for diabetes, especially as far as nutrition is concerned.9 Thus, addressing this group of patients poses a real challenge as they are in a special situation of vulnerability to develop hypoglycemia.32,33
In 2014, the reported prevalence of undernourishment worldwide was 10.9%.34 In Argentina, according to the data published by the Social Debt Observatory of the Argentine Catholic University (Observatorio de la Deuda Social Argentina (ODSA), Universidad Católica Argentina, UCA), food insecurity affects 13.8% of the population.7 A special module of questions is used to qualitatively and directly measure the problematic issue of food insecurity, which is expressed as the involuntarily cutting back on food portions and/or the perception of hunger experiences because of economic problems over the past 12 months. Food insecurity does not affect all people in the same way, being unequal within the social structure according to type of employment, socioeconomic status, housing conditions, educational level, the presence of children and head of household's gender.
Additionally, food insecurity among households located in slums and precarious settlements reached levels more than ten times higher than that in households located in upper-middle socioeconomic status neighborhoods. Similarly, the risk is also greater for households with a head who have an incomplete high school education. Analogously, in 2014 households with children are more likely to experience food insecurity than those comprised only of men. Furthermore, food insecurity is higher in households with a female head than in those with a male head of household.7 These data show that food insecurity has greater impact in low socio-economic groups, which may worsen the already existing social inequalities.
The association between food insecurity and the increased prevalence of chronic diseases, including diabetes, is well established.8,10,35–39 According to data from the NHANES40 survey conducted between 1999 and 2002, the likelihood of developing diabetes was twice as high for people with food insecurity, and this association was not attenuated after adjusting for body mass index (BMI), which suggests that this association cannot be totally attributed to the coexistence of obesity. The hypothesis accounting for the increased risk of diabetes is the substitution of healthy choice (fruits and vegetables) in the diet for low-cost high carbohydrate and fat meals, which increases the glycemic load and may lead to carbohydrate intolerance in predisposed individuals.8,41–43 In the other hand, diabetes can predispose to the development of food insecurity, due to the high cost of health care expenditures, which competes with healthy food choices.41–43
Food insecurity is associated with a greater risk of hypoglycemia.9,32,44,45 Similarly, glycemic control has been reported to be worse adult patients with diabetes who live in households with food insecurity.8,9,38,42,45–49 It is well accepted that food insecurity is a multidimensional concept that not only involves a reduction in the quantity and quality of food, but also involves additional mechanisms that may influence the glycemic control. According to Seligman et al., food insecurity can reduce self-efficacy, defined as the belief in one's own capacity to successfully deal with all that is necessary for the care of our own health, or can increase the emotional stress related to diabetes management.44 In a cross-sectional study involving low-income T2D patients, it was found that those with food insecurity were more likely to have HbA1c >8.5%, conferring a risk 50% greater compared with those patients who followed a healthy diet.38 These results support the hypothesis that food insecurity and cost-related underuse of medication are independently associated with poor diabetes control and a greater use of sanitary resources.43–47
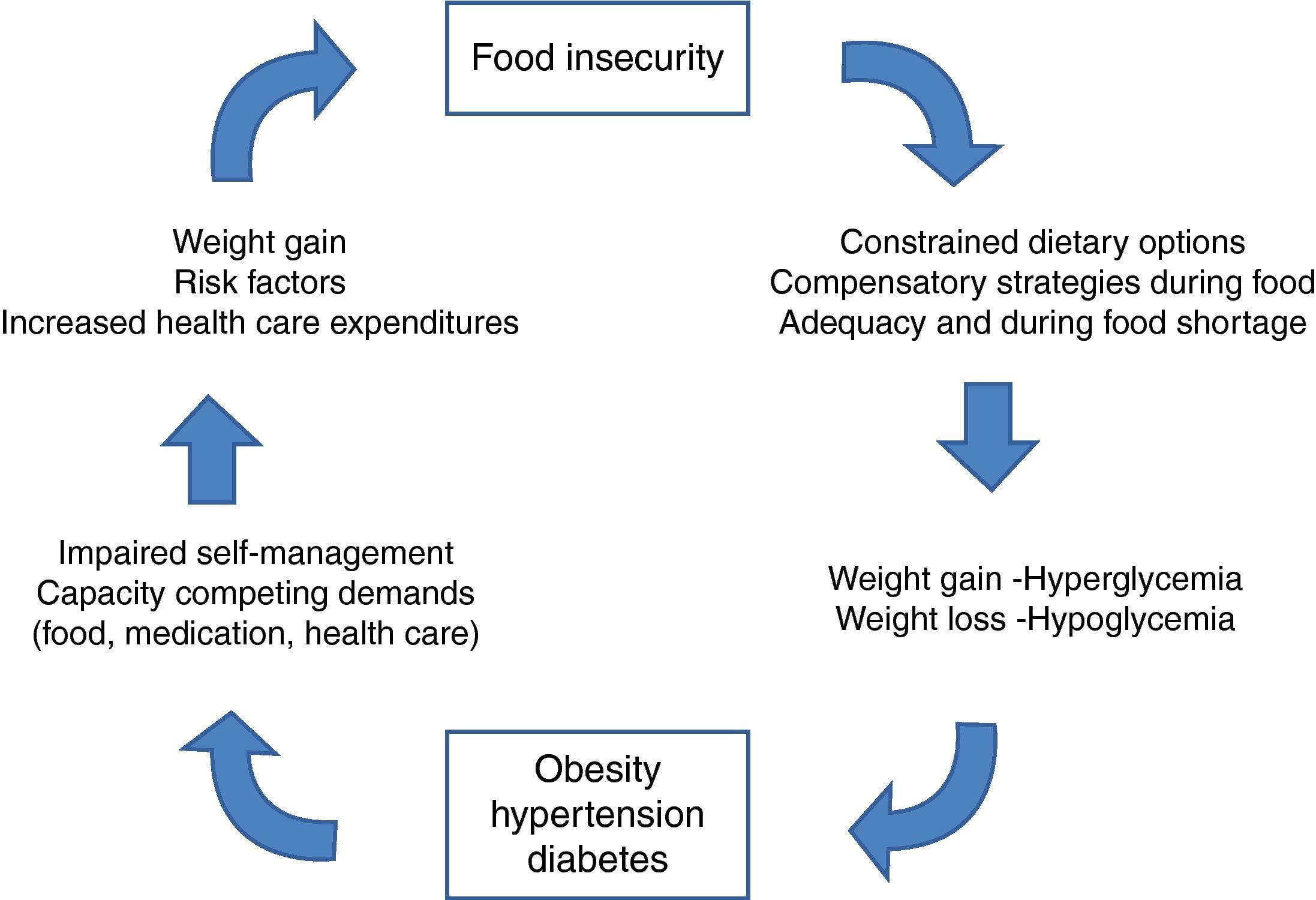
The “food insecurity cycle” shown in Fig. 1, explains how food insecurity may increase the risk of hyperglycemia and hypoglycemia in patients with diabetes. Hyperglycemia can occur as a result of inability to obtain adequate food or to excessive consumption during relatively sufficient food periods (i.e., first days of the month). On the other hand, hypoglycemia may occur when meals are skipped or when caloric intake is reduced due to inadequate food supply (last days of the month).9 Social vulnerability and food insecurity is a real phenomenon in many countries facing economic crises and in populations with insufficient incomes to obtain adequate diabetes treatment.
ConclusionThe epidemic of diabetes has taken root in the developing world, and it is known that 3 in 4 people with diabetes live in low-medium income countries, an epidemiological trend that will continue to rise in the future.50 In diabetes and in other chronic disorders, poverty and social exclusion add a negative effect establishing a vicious circle that worsens health outcomes and social welfare.
Hypoglycemic episodes are an unwanted effect in the treatment of diabetes and their frequency is increased in vulnerable populations with high rates of food insecurity. Few studies have evaluated this association but are mostly, observational retrospective design, which does not allow establishing a causality relationship. Despite these limitations, increasing evidence demonstrates that social vulnerability factors behave as independent risk predictors of severe hypoglycemia, even after adjusting for known demographic and clinical factors. In vulnerable populations, a socioeconomic vicious circle has been described, in which hypoglycemia is responsible for missed work (absenteeism) and a reduction in labor productivity leading to increased unemployment and food insecurity, which further increase the risk of hypoglycemia.
Increasing evidence indicates there is an association between severe hypoglycemia and dementia.51,52 Both conditions are increasing at an alarming rate and beginning to manifest at earlier ages. Cognitive impairment in socially vulnerable patients can generate an extra economic burden on the patient and his family. In addition, the decline in cognitive function may further increase the risk of severe hypoglycemia mainly in elderly patients.
Since hypoglycemia constitutes a major barrier to the successful management of diabetes, physicians and clinical guidelines must consider social vulnerability and food insecurity as important factors contributing to increased risk of hypoglycemia and poor metabolic control, which in turn may increase long-term complications of diabetes. Taking these factors into consideration will help provide a personalized medicine, adjusting glycemic goals and therapeutic approaches to the needs and social reality of each patient.
Conflict of interestDr. Waitman reports having received consulting fees or/and honoraria for membership in advisory boards from Novo Nordisk, Astra Zeneca and Sanofi.
Dr. Umpierrez is supported in part by research grants from the American Diabetes Association (1-14-LLY-36), PHS grant UL1 RR025008 from the Clinical Translational Science Award Program (M01 RR-00039), and grants from the National Institute of Health and the National Center for Research Resources. He has received unrestricted research support for inpatient studies (at Emory University) from Merck, Novo Nordisk, Astra Zeneca, Boehringer Ingelheim, and Sanofi, and has received consulting fees or/and honoraria for membership in advisory boards from Novo Nordisk, Sanofi, Merck, Johnson and Johnson and Boehringer Ingelheim.
Dr. Caeiro has nothing to disclose.
Dr. Gonzalez has nothing to disclose.
Dr. Romero has nothing to disclose.
Dr. Ré has nothing to disclose.
RD Daghero has nothing to disclose.