Diabetes mellitus (DM) is included in the disease group described as the pandemic of the century. Although disease management is possible, it can significantly reduce the quality of life when glycaemic control is poor. The objective of this systematic review was to examine the effectiveness of different educational programmes on the management of the disease among type 2 DM patients.
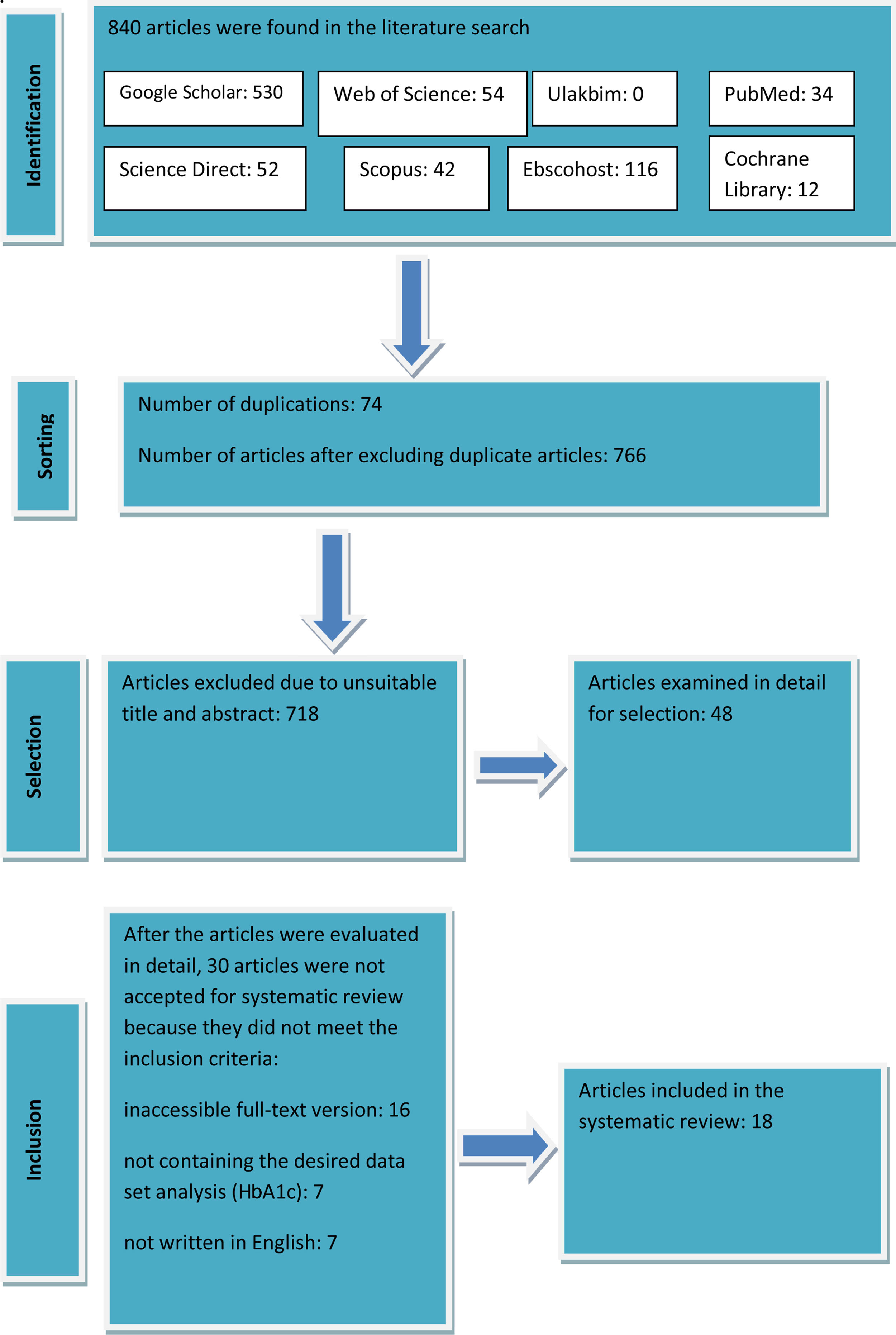
MethodsIn the literature review, the flow chart of PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols) was used. A literature search was conducted from 2010 to 2020 using the Ulakbim National Database, Google Scholar, Scopus, PubMed, Library, Science Direct, Web of Science, Medline, Ebscohost and Cochrane Library, and 18 English randomised controlled studies were included.
ResultsWithin the scope of these studies, it was found that individualised and face-to-face training and long-term follow-up after the training were effective on metabolic control. Peer support was also determined as an important factor in the efficacy of the training. In line with the training, the self-management and quality-of-life scores of the individuals with diabetes were positively affected.
ConclusionsIt can be suggested that planned and regular training has a positive effect on metabolic control variables, self-management behaviours and quality of life of individuals with diabetes. Regular training for individuals with diabetes and follow-up for more than 6 months are recommended since they have a positive effect on the disease. It is also recommended to integrate peer support into training programmes.
La diabetes mellitus (DM) es una de las enfermedades descritas como la pandemia del siglo. Si bien es posible controlar la enfermedad, esta puede reducir significativamente la calidad de vida cuando el control glucémico es deficiente. El objetivo de esta revisión sistemática fue evaluar la eficacia de diferentes programas educativos sobre la gestión de la enfermedad entre los pacientes con DM tipo 2.
MétodosEn la revisión bibliográfica se utilizó el diagrama de flujo de PRISMA-P (por sus siglas en inglés: elementos de informes preferidos para los protocolos de revisión sistemática y metaanálisis). Se realizó una búsqueda bibliográfica desde 2010 hasta 2020 utilizando la base de datos nacional Ulakbim, Google Scholar, Scopus, PubMed, Library, Science Direct, Web of Science, Medline, Ebscohost y Cochrane Library y se incluyeron 18 estudios ingleses controlados aleatorizados.
ResultadosEn el contexto de estos estudios se comprobó que la formación individualizada y presencial y el seguimiento a largo plazo tras la formación eran eficaces para lograr el control metabólico. También se determinó que el apoyo por los iguales era un factor importante para garantizar la eficacia de la formación. En consonancia con la formación, las puntuaciones de autogestión y calidad de vida de las personas con diabetes se vieron afectadas positivamente.
ConclusionesEs posible sugerir que la formación planificada y regular tiene un efecto positivo sobre las variables de control metabólico, las conductas de autogestión y la calidad de vida de las personas con diabetes. Se recomienda formar regularmente a las personas con diabetes y llevar a cabo un seguimiento durante un mínimo de 6 meses, ya que ambas intervenciones tienen un efecto positivo sobre la enfermedad. También se recomienda integrar el apoyo por los iguales en los programas de formación.
Diabetes mellitus (DM) has become an increasingly important public health problem all over the world. According to the International Diabetes Federation, the number of individuals with diabetes worldwide was 425 million in 2017 and will probably increase to 629 million by 2045.1
Patients may experience many complications due to the nature of DM, because of late diagnosis and poor management of the disease. Poor glycaemic control is related to the development of diabetes complications.2,3 Acute complications of the disease are hypoglycaemia, diabetic ketoacidosis and hyperglycaemic hyperosmolar state. Chronic complications are microvascular (diabetic retinopathy, diabetic nephropathy and diabetic neuropathy) and macrovascular (cardiovascular diseases, peripheral artery disease and cerebrovascular diseases) problems. While acute complications are more dynamic, chronic complications develop over a long time and can lead to more serious damage. Coronary artery disease, a chronic complication, develops 2–4 times more in diabetic individuals compared to healthy individuals.4,5 While 2% of individuals with diabetes lose their vision, 20–40% experience nephropathy and, as a result, become dialysis patients.6,7 In 15% of patients with neuropathy, another complication of DM, foot wounds can develop and this situation can negatively affect the quality of life. The prevention or reduction of the severity of these complications can be possible with good glycaemic control.8,9 Galli et al. reported that the development of nephropathy is directly related to poor glycaemic control.45 In the study of Tao et al., the diabetic patients who performed good self-monitoring during their stay at home during the coronavirus pandemic lockdown, had better outcomes while individuals with poor glycaemic control had significantly higher complication rate.10
Patients with DM need effective and continuous care and follow-up programmes, including training, to provide glycaemic control, to increase the quality of life, and to prevent the development of complications.11,12 Ranasinghe et al. examined the effectiveness of exercise on glycaemic and cardiometabolic control in the patients with type 2 diabetes, and reported that physical activity was significantly effective in providing glycaemic control.13 Comellas et al. determined that nutrition, exercise and regular medication use provided glycaemic control in diabetic individuals.14 The American Diabetes Association (ADA) has emphasised that nutrition, exercise and medication are important in the control of the disease. Both healthcare institutions and diabetic individuals should be actively involved in the treatment plan and self-management.8,15 Diabetic patients must have sufficient knowledge, skills and positive attitudes to successfully manage diabetes.16 Patients’ beliefs and attitudes towards diabetes are crucial in diabetes treatment and affect the outcomes of the disease. Attitude and behaviour change is possible with education.17 Training programmes should include all of the knowledge, attitudes and skills that ensure the continuity of care for patients with diabetes and their families.18 The training of diabetic individuals requires the teamwork of healthcare professionals, such as physicians, nutritionists, psychologists and nurses. Nurses play a key role in this teamwork by coordinating, planning, implementing and evaluating training programmes for individuals with DM.19
Although the basic information in DM training is standard, factors such as the frequency and duration of the training, and the training material itself, can create differences in the specified goals.20 There are studies in the literature for diabetic individuals, including different training methods, training durations and results evaluation. However, no recent systematic review of these studies was found in the relevant literature. Examining the studies evaluating the training for diabetic individuals can provide a guide to developing DM management strategies and establishing effective training programmes, by contributing to the improvement of the evidence-based knowledge level on the subject. This systematic review aims to assess the randomised controlled studies that examined the effectiveness of different training programmes on the management of DM.
Materials and methodsThe systematic review was written according to the recommendations in the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Since the existing studies were reviewed only, approval from the ethics committee was not required for this study.21
Search strategyFor this systematic study, the English keywords “type 2 diabetes, diabetes mellitus, diabetes education, diabetes management, nursing, randomised controlled” were searched between 2010 and 2020. The literature search was conducted between 16 November and December 2020 using the Ulakbim National Database, Google Scholar, Scopus, PubMed, Library, Science Direct, Web of Science, Medline, Ebscohost and Cochrane Library. The studies found as a result of the literature search were categorised according to the databases and shown in the PRISMA-P flow chart.
Inclusion criteriaThis systematic review included the full-text randomised controlled studies published in English between 2010 and 2020, in which individuals with type 2 DM were trained in disease management.
The studies which were included in the systematic review were chosen according to the study design (PICOS) model of the Joanna Briggs Institute. P: population (the type of participants), participant characteristics; I: types of interventions, the characteristics of the intervention; C: comparator (types of comparisons), the feature of group comparison; O: outcome (types of outcomes), results; Q: study designs (Ttpes of studies) (Fig. 1).21
- •
P: the studies which were conducted with individuals with type 2 DM and over the age of 18, regardless of gender, race or socio-economic status, were included in this study.
- •
I: the nursing studies including the training of patients for type 2 DM management were examined.
- •
C: the studies comparing the effectiveness of training and other applications in type 2 DM management were included in the study.
- •
O: health criteria (frequency of acute and chronic complications, frequency of hospitalisation, HbA1c values, weight, blood lipid level), knowledge (level of knowledge, exercise status), attitude (health promotion, self-efficacy and insulin) were evaluated as parameters affecting disease management in type 2 DM.
- •
S: the randomised controlled trials were included in the study.
The non-randomised studies with type 2 DM patients before 2010, that included no training results on disease management, were not included in this study.
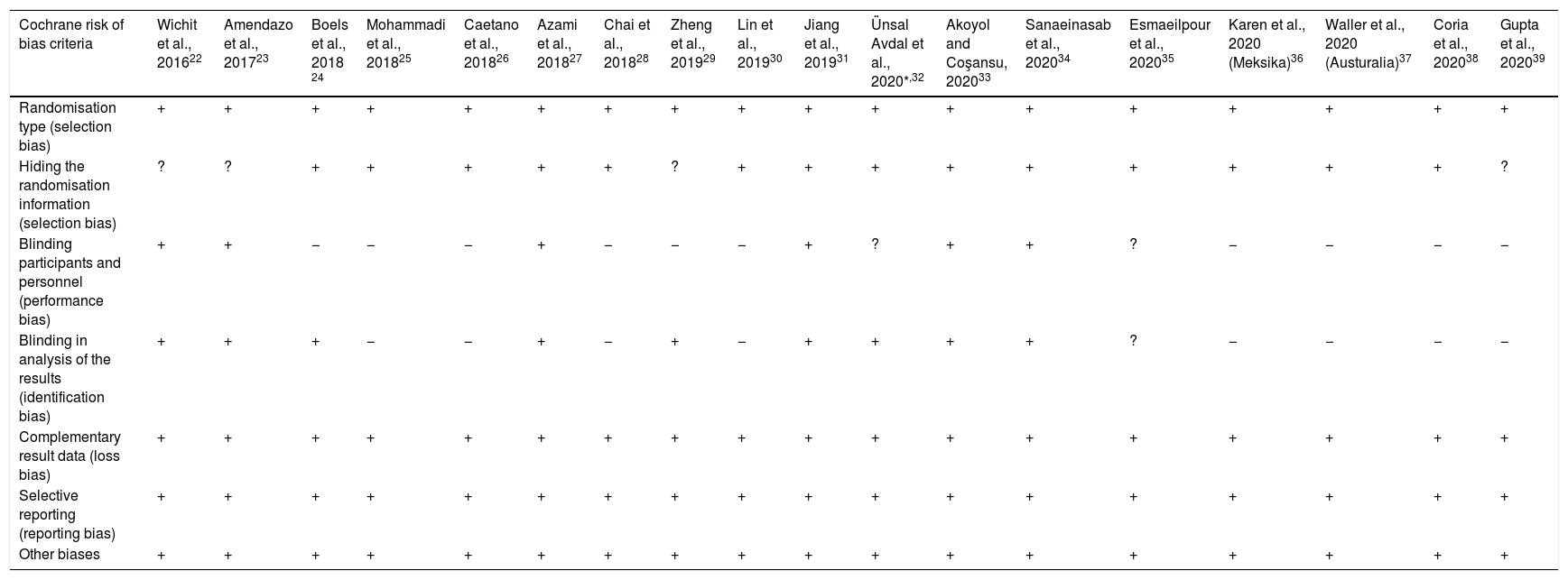
Risk of bias assessmentIn all studies included in the review, the risk of bias was assessed by the researchers using the Cochrane risk of bias tool. The assessment included mode of randomisation (selection bias), hiding randomisation information (selection bias), blinding participants and staff (performance bias), blinding (determination bias) in result evaluation, incomplete results data (loss bias), selective reporting (reporting bias) and other biases. A consensus was achieved by the authors regarding bias assessment. In the included studies, the risk of bias was evaluated in three levels: low, unclear and high (Table 1). While only four of the 18 studies included in our study were considered to be with low risk, six of them were considered to be with unclear risk, and eight of them were considered as with high risk. In the studies where the risk of bias is considered to be high, the determined issues are considered as research limitations.
Evaluation of the risk of bias: +=low risk; ?=unclear risk; −=high risk.
| Cochrane risk of bias criteria | Wichit et al., 201622 | Amendazo et al., 201723 | Boels et al., 2018 24 | Mohammadi et al., 201825 | Caetano et al., 201826 | Azami et al., 201827 | Chai et al., 201828 | Zheng et al., 201929 | Lin et al., 201930 | Jiang et al., 201931 | Ünsal Avdal et al., 2020*,32 | Akoyol and Coşansu, 202033 | Sanaeinasab et al., 202034 | Esmaeilpour et al., 202035 | Karen et al., 2020 (Meksika)36 | Waller et al., 2020 (Austuralia)37 | Coria et al., 202038 | Gupta et al., 202039 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Randomisation type (selection bias) | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Hiding the randomisation information (selection bias) | ? | ? | + | + | + | + | + | ? | + | + | + | + | + | + | + | + | + | ? |
| Blinding participants and personnel (performance bias) | + | + | − | − | − | + | − | − | − | + | ? | + | + | ? | − | − | − | − |
| Blinding in analysis of the results (identification bias) | + | + | + | − | − | + | − | + | − | + | + | + | + | ? | − | − | − | − |
| Complementary result data (loss bias) | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Selective reporting (reporting bias) | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Other biases | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
As a result of searching with the keywords and their synonyms in Google Scholar (530), EBSCOhost/CINAHL Complete (116), PubMed (34), Scopus (42), Science Direct (52), Web of Science (54) and Cochrane Library (12), a total of 840 studies were found. Repeated studies, studies with unsuitable titles and abstracts were excluded. The remaining 48 studies were re-evaluated for the inclusion and exclusion criteria. In line with these evaluations, 18 studies that met the inclusion criteria were included in the systematic review (Fig. 1).
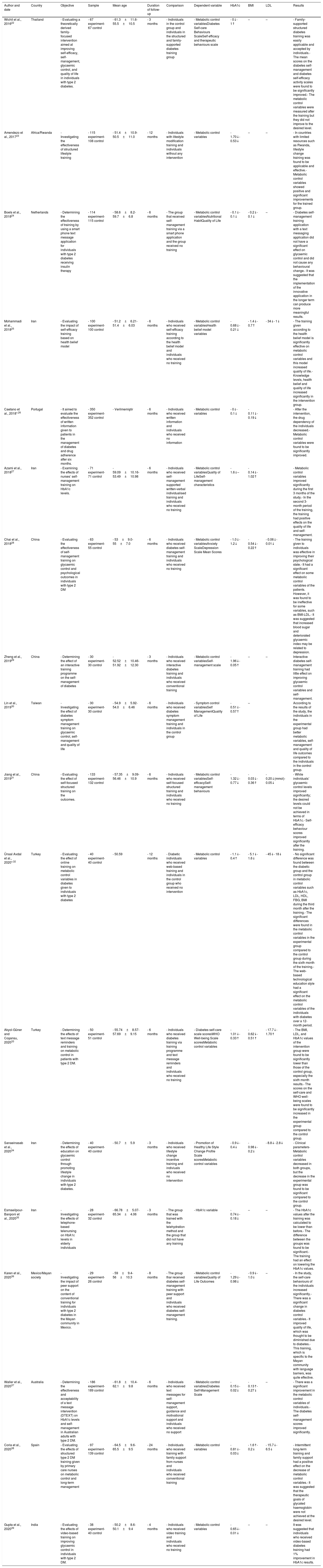
The findings obtained as a result of a detailed examination of 18 studies (Table 2) were evaluated according to five subjects: characteristics of the studies, style of training, duration of the training, outcomes of metabolic control, and outcomes of self-management of diabetes.
Studies on the effectiveness of disease management training for patients with type 2 diabetes mellitus.
| Author and date | Country | Objective | Sample | Mean age | Duration of follow-up | Comparison | Dependent variable | HbA1c | BMI | LDL | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wichit et al., 201622 | Thailand | - Evaluating a theoretically derived family-focused intervention aimed at improving self-efficacy, self-management, glycaemic control, and quality of life in individuals with type 2 diabetes. | - 67 experiment- 67 control | - 61.3±11.6- 55.5±10.5 | - 3 months | - Individuals in the control group and individuals in the structured and family-supported diabetes training group | - Metabolic control variablesDiabetes Self-care Behaviours ScaleSelf efficacy and therapeutic behaviours scale | - 0↓- 1↑ | – | – | - Family-supported structured diabetes training was easily applicable and accepted by individuals.- The mean scores on the diabetes self-management and diabetes self-efficacy activity scales were found to be significantly improved.- The metabolic control variables were measured after the training but they did not improve to the desired level. |
| Amendezo et al., 201723 | Africa/Rwanda | - Investigating the effectiveness of structured lifestyle training | - 115 experiment- 108 control | - 51.4±10.9- 50.5±11.0 | - 12 months | - Individuals with lifestyle modification training and individuals without any intervention | - Metabolic control variables | - 1.70↓- 0.53↓ | – | – | - In countries with limited resources such as Rwanda, lifestyle change training was found to be applicable and effective.- Metabolic control variables showed positive and significant improvements for the trained group. |
| Boels et al., 201824 | Netherlands | - Determining the effectiveness of training by using a smart phone text message application for individuals with type 2 diabetes receiving insulin therapy | - 114 experiment- 115 control | - 58.6±8.2- 59.7±6.8 | - 6 months | - The group that received self-management training via a smart phone application and the group received no training | - Metabolic control variablesNutritional HabitQuality of Life | - 0.1↓- 0.1↓ | - 0.2↓- 0.1↓ | – | - Diabetes self-management training application with a text messaging application did not have a significant effect on glycaemic control and did not cause any behavioural change.- It was suggested that the implementation of the innovative application in the longer term can produce more meaningful results. |
| Mohammadi et al., 201825 | Iran | - Evaluating the impact of self-efficacy training based on health belief model | - 100 experiment- 100 control | - 51.2±6.21- 51.4±6.03 | - 6 months | - Individuals who received self-efficacy training according to the health belief model and individuals who received no training | - Metabolic control variablesHealth belief model variables | - 0.68↓- 0.21↓ | - 1.4↓- 0.7↑ | - 34↓- 1↓ | - The training given according to the health belief model is significantly effective on metabolic control variables and this model increased quality of life.- Knowledge levels, health belief and quality of life increased significantly in the intervention group. |
| Caetano et al., 2018*,26 | Portugal | - It aimed to evaluate the effectiveness of written information given to patients in the management of diabetes and drug adherence after six months. | - 350 experiment- 352 control | - Verilmemiştir | - 6 months | - Individuals who received written information and individuals who received no information | - Metabolic control variables | - 0↓- 0.1↓ | - 0.11↓- 0.19↓ | - After the intervention, the drug dependency of the individuals decreased.- Metabolic control variables were found to be significantly improved. | |
| Azami et al., 201827 | Iran | - Examining the effects of nurses’ self-management training on HbA1c levels. | - 71 experiment- 71 control | - 59.09±10.16- 53.49±10.98 | - 6 months | - Individuals who received self-management supported written-verbal individualised training and individuals who received no training | - Metabolic control variablesQuality of LifeSelf-management characteristics | - 1.6↓– | - 0.14↓- 1.02↑ | - Metabolic control variables improved significantly during the first 3 months of the study.- In the second 3-month period of the training, the training had positive effects on the quality of life and self-management. | |
| Chai et al., 201828 | China | - Evaluating the effectiveness of self-management training on glycaemic control and psychological outcomes in individuals with type 2 DM | - 63 experiment- 55 control | - 53±9.0- 55±7.0 | - 6 months | - Individuals who received diabetes self-management training and individuals who received no training | - Metabolic control variablesAnxiety ScaleDepression Scale Mean Scores | - 1.0↓- 1.2↓ | - 0.54↓- 0.22↑ | - 0.06↓- 0.01↓ | - The training given to individuals was effective in improving their psychological state.- It had a significant effect on some metabolic control variables of the patients. However, it was found to be ineffective for some variables, such as BMI-LDL.- It was suggested that increased blood sugar and deteriorated glycaemic index may be related to depression. |
| Zheng et al., 201929 | China | - Determining the effect of an interactive training programme on the self-management of diabetes | - 30 experiment- 30 control | - 52.52±10.46- 51.92±12.30 | - 3 months | - Individuals who received interactive diabetes training and individuals who received conventional training | - Metabolic control variablesSelf-management scale | - 1.96↓- 0.05↑ | – | – | Interactive diabetes self-management training had little effect on improving glycaemic control variables and self-management. |
| Lin et al., 201930 | Taiwan | - Investigating the effect of diabetes symptom management training on glycaemic control, self-management and quality of life | - 30 experiment- 30 control | - 54.9±5.92- 54.0±6.46 | - 6 months | - Individuals who received diabetes symptom management training and individuals in the control group | - Symptom control variablesSelf ManagementQuality of Life | - 0.51↓- 0.57↑ | – | According to the results of the study, the individuals in the experimental group had better metabolic variables, self-management and quality of life outcomes compared to the individuals in the control group. | |
| Jiang et al., 201931 | China | - Evaluating the effect of self-focused structured training on the outcomes. | - 133 experiment- 132 control | - 57.35±9.09- 56.46±10.9 | - 6 months | - Individuals who received self-focused structured training and individuals who received no training | - Metabolic control variablesSelf-efficacySelf-management behaviours | - 1.32↓- 0.77↓ | - 0.03↓- 0.36↑ | - 0.20↓(mmol)- 0.05↓ | - While individuals’ glycaemic control levels improved significantly; the desired levels could not be achieved in terms of HbA1c.- Self-efficacy behaviour scores improved significantly after the training. |
| Ünsal Avdal et al., 2020*,32 | Turkey | - Evaluating the effect of online training on metabolic control variables in diabetes given to individuals with type 2 diabetes | - 40 experiment- 40 control | - 50.59 | - 12 months | - Diabetic individuals who received web-based training and individuals in the control group who received no intervention | - Metabolic control variables | - 1.1↓- 0.4↑ | - 5.1↓- 1.6↓ | - 45↓- 18↓ | - No significant difference was found between the diabetic group and the control group in metabolic control variables such as HbA1c, LDL, HDL, FBG, BMI during the third month after the training.- The significant differences were found in the metabolic control variables in the experimental group compared to the control group during the sixth month of the training.- The web-based technological education style had a significant effect on the metabolic control variables of the individuals with diabetes over a 12-month period. |
| Akyol-Güner and Coşansu, 202033 | Turkey | - Determining the effects of text message reminders and training on metabolic control in patients with type 2 DM. | - 50 experiment- 51 control | - 55.74±8.57- 57.69±9.15 | - 6 months | - Individuals who received diabetes training via training programme and text message reminders and individuals who received no training | - Diabetes self-care scale scoresWHO Well-being Scale scoresMetabolic control variables | - 1.01↓- 0.33↑ | - 0.62↓- 0.51↑ | - 17.7↓- 1.70↑ | - The BMI, LDL, and HbA1c values of the intervention group were found to be significantly lower than those of the control group, especially the sixth month results.- The scores on the self-care and WHO well-being scales were found to be significantly increased in the experimental group compared to the control group. |
| Sanaeinasab et al., 202034 | Iran | - Determining the effects of education on glycaemic control through promoting lifestyle change in individuals with type 2 diabetes. | - 40 experiment- 40 control | - 50.7±5.9 | - 3 months | - Individuals who received lifestyle change incentive training and indiviuals who received no intervention | - Promotion of Healthy Life Style Change Profile Scale scoresMetabolic control variables | - 0.9↓- 0.4↓ | - 0.98↓- 0.2↓ | - 8.8↓- 2.8↓ | - Clinical parameters- Metabolic control variables decreased in both groups, but the decrease in the experimental group was found to be significant compared to the control group. |
| Esmaeilpour-Banponi et al., 202035 | Iran | - Investigating the effects of telephone-based telenursing on HbA1c levels in elderly individuals | - 28 experiment- 32 control | - 66.78±5.07- 65.34±4.06 | - 3 months | - The group that was trained with the telehydration method and the group that did not have any training | - HbA1c variable | - 0.74↓- 0.18↓ | – | – | - The HbA1c values after the training was calculated to be lower than before.- The difference between the groups was found to be significant.- The training had an effect on lowering the HbA1c values. |
| Karen et al., 202036 | Mexico/Mayan society | - Investigating the impact of peer support on the content of conventional training for individuals with type 2 diabetes in the Mayan community in Mexico. | - 29 experiment- 26 control | - 59±9.4- 56±10.3 | - 8 months | - The group thar received diabetes self-management training with peer support and individuals who received diabetes self-management training. | - Metabolic control variablesQuality of Life Outcomes | - 1.29↓- 0.98↓ | - 0.9↓- 1.0↓ | – | - In the study, the self-care behaviours of the individuals increased significantly.- There was a significant change in diabetes control variables.- It improved quality of life, which was thought to be diminished due to diabetes.- This training, which is specific to the Mayan community with language barriers, was quite effective. |
| Waller et al., 202037 | Australia | - Determining the effectiveness and acceptability of a text message intervention (DTEXT) on HbA1c levels and self-management in Australian adults with type 2 DM. | - 186 experiment- 189 control | - 61.8±10.4- 62.1±9.8 | - 6 months | - Individuals who received text messages for self-management support, guidance and motivational support and individuals who received no support | - Metabolic control variablesDiabetes Self-Management Scale | - 0.15↓- 0.02↓ | - 0.13↑- 0.27↓ | – | - There was a significant improvement in the metabolic control variables of individuals.- The diabetes self-management scores improved significantly. |
| Coria et al., 202038 | Spain | - Evaluating the effects of structured type 2 DM training given by primary care nurses on metabolic control and long-term management | - 97 experiment- 139 control | - 64.5±9.6- 65.5±9.5 | - 24 months | - Individuals who received training with family support from nurses and individuals who received conventional training | - Metabolic control variables | - 0.81↓- 0.03↓ | - 1.6↑- 0.2↓ | - 15.7↓- 6.5↓ | - Intermittent long-term training and family support had a positive effect on the decrease of metabolic control variables.- It was suggested that the therapeutic goals of glycated haemoglobin were not achieved at the desired level. |
| Gupta et al., 202039 | India | - Evaluating the effects of video-based training on improving glycaemic control in individuals with type 2 DM. | - 38 experiment- 40 control | - 50.2±8.6- 50.1±9.4 | - 4 months | - Individuals who received video training and individuals who received no training | - Metabolic control variables | - 0.65↓- 0.01↓ | – | – | It was suggested that individuals who received video-based diabetes training had 1% improvement in HbA1c results. |
All of the randomised controlled trials that were included in this systematic review were designed as longitudinal studies with follow-up evaluations. Type 2 DM patients who were admitted to the outpatient clinics to improve the management of the disease comprised the samples of the studies. The studies investigated the effectiveness of the training programmes provided for diabetes management on improving self-management, changing lifestyle, improving quality of life and metabolic results. Only one study addressed the psychological aspects of the disease.28 Two studies investigated the importance and effect of peer and family support in education.22–36 In addition, ethical approval was obtained for all of the studies included in the review before the research was conducted.
Training methodIn the majority (55.5%) of the studies examined, the effectiveness of education in the management of type 2 DM, individualised face-to-face traditional training was applied.22,23,25,27–29,31,34,36,38 Caetano et al.26 conducted a study to reduce the drug addiction of diabetic patients and used self-management brochures in addition to traditional education. Within the scope of diabetes training, there are also technology-based training applications such as telenursing to reduce the HbA1c levels of elderly individuals.35 In one study, video training was carried out to improve glycaemic control.39 In three studies included in the review, training was provided with an SMS reminder application.24,33,37 In the study by Akyok-Güner and Coşansu, text messages were sent to patients to remind them after self-management training for diabetes and metabolic control.33 In the study by Waller et al., text messages were used to control diabetes self-management behaviours and HbA1c levels.37 Ünsal-Avdal applied a web-based training programme; the training content supporting self-management of diabetes was provided on the internet, and the data were also collected online.32
Duration of follow-up/trainingThe studies included in this systematic review were evaluated in terms of duration of the follow-up and training. There are studies (88.8%) involving a minimum of three months and a maximum of 24 months of follow-up for the assessment of metabolic control for diabetes management.22–29,31–38 The metabolic assessment was carried out in all of the studies. Follow-up durations were 3 months in 4 studies, 4 months in 1 study, 6 months in 9 studies, 8 months in 1 study, 12 months in 2 studies, and 24 months in 1 study. During these periods, metabolic examinations and scale applications were performed on the patients through outpatient clinic services for follow-up. The duration of the studies can be shortened or extended according to the parameters. In the studies in which only the metabolic effect of the training was evaluated, a 3-month follow-up was performed.22,29,34,35 In the studies with anticipated effects on quality of life, behavioural changes or psychological effects, the duration was up to 24 months.23,32,38
Outcomes of metabolic controlIn the studies included in this systematic review, measurable values such as HbA1c, BMI, and LDL were examined to evaluate the effectiveness of training on diabetes management. In the studies (50%) in which individualised conventional education was applied,22,23,25,27,28,31,34,36,38 the metabolic control variables (especially the HbA1c level) of the individuals in the experimental groups were found to be statistically significantly different from those in the control group. In the studies in which training was via smartphones, text messages or written brochures,24,26,33,35,37 there was no statistically significant difference between the experimental and control groups in metabolic control variables. In particular, a decrease in BMI and LDL levels occur in longer periods and therefore it is suggested that the duration of training programmes and follow-up periods should be longer to reduce these values.2
Outcomes of diabetes self-managementThe concept of self-management was included in six of the studies in which training programmes were applied for the management of diabetes.22,25,27–29,37 In all of these studies, a significant improvement was observed in diabetes self-management scores after training. Wichit et al.22 reported that involving family support in diabetes management training programmes had positive effects on self-management. Mohammadi et al.25 showed that training programmes based on the health belief model contributed significantly to self-management in diabetic patients. Karen et al.36 conducted a study with individuals living in the Mayan community in Mexico. They determined that desired results in self-efficacy were obtained by peer-supported diabetes management training and the removal of the language barrier. Boels et al.24 also found that training via text messages did not provide desired outcomes in self-management.
Quality of life resultsQuality of life was examined in five of the studies in which training was given for the management of diabetes.22,24,25,27,36 Karen et al.36 increased the quality of life of the diabetic individuals in the Mayan community in Mexico by providing training. The training programme provided by Mohammadi et al., according to the health belief model, significantly increased the quality of life of the diabetic patients in the experimental group.25Azami et al. emphasised that there was an improvement in the quality of life in the second trimester of post-training follow-up among the patients with type 2 DM.27
DiscussionManagement of the disease in individuals with type 2 DM is very important in achieving glycaemic control, improving quality of life and preventing complications. Patients can adapt to living with diabetes and learn diabetes management through education. The studies reviewed in this systematic review included randomised controlled studies that included training to improve disease management, metabolic control, self-management and quality of life in individuals with type 2 DM.
In the studies examining the effectiveness of the training for the management of type 2 diabetes, individualised face-to-face or technology-based training methods were used and the patients were followed up for 3–24 months after training. In most of the studies, individualised and face-to-face training given to the patients with type 2 DM positively affected their health outcomes, especially metabolic variables. Since diabetes is a life-long disease, it is suggested that giving face-to-face, conventional and individualised training to these individuals is more effective in determining their needs. Considering the financial and moral burden and mental effects of the disease, an individualised approach can be useful in directing the necessary support systems. However, in some studies comparing individualised and group-based education models, both types of education were effective.40–42 Rickheim et al.40 compared the effectiveness of individual and group training given to patients with diabetes, and reported that the patients participating in group sessions had a decline in HbA1c levels as effective as those in individual sessions. Norris et al.43 reported in their study comparing group and individual training in diabetic individuals, that group training was beneficial in issues such as lifestyle changes. In the study by Erskine et al.,44 it was concluded that, the level of satisfaction was higher in the patients who participated in the group sessions in the training on insulin therapy. As a result of the studies, it is recommended to decide the educational method according to the advantages of the individual or group education.40,44
In some studies, conducted for the training of individuals with diabetes, the use of technology, such as mobile phones, was found to be effective. However, researchers could not achieve their desired goals.46,47 In fact, according to the results of some studies, training programmes using mobile phones and smartphones were reported to be insufficient in metabolic control parameters and self-management outcomes. Mario et al. and Hooshmand et al. also reported similar results regarding phone-based education.48,49 It is argued that when the standardisation and access infrastructure is better and prepared according to certain standards, phone applications and web-based training programmes can be more effective.46,50
It is recommended that individuals be followed up for a minimum of three months after diabetes training. This is due to the fact that the evaluation of HbA1c level requires a minimum of three months to evaluate the efficiency of the training.51,59 The duration of training in the studies included in this systematic review varied between three months and 24 months. According to the results of these studies, HbA1c levels reduced in the first three months while LDL levels and BMI lowered in a longer period. Some studies did not use LDL level in the control chart. Some other studies similarly reported that while HbA1c levels decreased to the desired level in the first, third and sixth month follow-up results of individuals with type 2 DM after the training in lifestyle change, LDL and cholesterol levels could be decreased in 12 months.52–54 Improvement in patient outcomes suggests that diabetes training positively affects patients’ behaviours in regard to medication use, exercise and nutrition, and is effective in disease management. In this systematic review, examination of the effectiveness of diabetes education on metabolic control variables showed mostly a decrease in HbA1c level, with fewer improvements in values such as BMI, LDL and HDL. Studies in the literature showed that, the method, content and duration of diabetes education were highly effective in the level of glycaemic control variables.55–57
In the studies evaluating areas such as self-management and quality of life in DM, training generally affected self-management and quality of life positively. In particular, individualised, family and peer-supported approaches improved patient outcomes. Rosland et al. reported that practical and emotional support from both family and friends had a positive effect on disease management measures in patients with diabetes.64 Pereira et al. also highlighted the importance of incorporating family variables in psychological interventions in diabetes care.65 Self-management and quality of life are associated with metabolic control, as well as with reducing the frequency of complications and improving individual well-being. The development of self-management leads to a decrease in HbA1c levels and complications, and as a result, the quality of life is improved.58 To improve self-management in diabetes, three-month (or longer) training and follow-up studies are recommended.60 It was shown that the duration of training and follow-up were longer in the studies examining the concepts of self-management, lifestyle change and quality of life.53,61,62 Having a chronic disease is accepted as a stressor for individuals; living with this stress and adapting to the disease may take time.51,63 The thought of living with the disease, the ability to cope with the disease and the ability to manage the disease may be improved with training. Self-management and quality of life can also be improved with permanent learning.
Overall, the results of this systematic review highlight the importance of designing effective educational plans for positive outcomes in patients with type 2 DM. There are similar previous systematic reviews in the relevant literature including various date intervals, regions and aims. In a systematic review conducted by Loveman et al. with 13 studies (2008), the methodologies of the examined studies were variable and they suggested preparation of evidence-based, planned, evaluable and standardised training content.66 Qingqing et al. performed a systematic review in mainland China based on the 34 articles regarding diabetes education. They found that popular educational methods were classroom teaching, or one-on-one teaching, and knowledge and glycaemic control were mostly selected as the outcome measurements. The beneficial effects of diabetes education on knowledge and glycaemic control were demonstrated in studies.67 In a systematic review conducted by Vas et al. with 14 studies to assess the effectiveness of self-management programmes in diabetes management, a wide variety of interventions were used, including diabetes education as a major component in self-management programmes. It was showed that the results of HbA1c self-management improved in the long or short term and were similar to those in our study.68
ConclusionThis systematic review was conducted to evaluate the effectiveness of different training programmes for type 2 DM patients on how to manage the disease. We have examined 18 studies and determined that providing training for patients with type 2 diabetes on how to manage the disease significantly contributes to their metabolic control variables, diabetes self-management skills, lifestyle change and quality of life. In the reviewed studies, patients were followed up for 3–24 months after training. In most of the studies, individualised and face-to-face training given to the patients with type 2 DM positively affected their health outcomes, especially metabolic variables. In some studies, using technology such as mobile phones was found to be effective; however, researchers could not achieve their desired goals. Examination of the effectiveness of diabetes education on metabolic control variables showed mostly a decrease in HbA1c level and more moderate improvements BMI, LDL and HDL. In the studies evaluating areas such as self-management and quality of life in DM, training generally affected self-management and quality of life positively. In particular, individualised, family and peer-supported approaches improved patient outcomes. In the light of this information, we recommend that the technology-assisted individualised training of individuals with diabetes should be carried out with the presence of social support for longer than three months. The quality of life of patients can be improved by developing strategies for diabetes training, ensuring effective disease management and preventing complications.
FundingNo financial support was received from private companies.
Conflict of interestThe authors declare no conflict of interest.