The diagnosis of type 1 diabetes mellitus (DM1) has a major impact on young people and their families. Psychosocial factors, patient motivation, participation and acceptance of the disease are essential to achieve good blood glucose control. Our aims were to analyse personality traits and how they are related to blood glucose control in patients with DM1.
MethodsSixty-two patients with DM1 over 18 years of age, with at least one-year disease duration and absence of advanced chronic complications were studied. Clinical, biological and personality parameters were measured. The Millon Index of Personality Styles was administered for personality assessment.
ResultsSignificant correlations between different personality variables and glycated haemoglobin (HbA1c) values were found. Individuals with poor blood glucose control had significantly higher scores on the Feeling-guided (53.6±25.7 vs 36.2±26.8, p=0.021), Innovation-seeking (36.7±24.1 vs 21.9±21.4, p=0.025), Dissenting (41.1±24.4 vs 15.6±16.6, p=0.001), Submissive (41.5±25.1 vs 28.3±14.7, p=0.038) and Dissatisfied (37.5±27.5 vs 19.5±20.2, p=0.015) scales. This psychological profile is characterised by greater focus on emotions and personal values (feeling-guided), the tendency to reject conventional ideas (innovation-seeking), an aversion to complying with norms and a preference for autonomy (unconventional/dissenting), labile self-confidence (submissive/yielding) and expressed disagreement with others (dissatisfied/complaining). Factor analysis based on the main components of the variance yielded four factors. Factor characterised as related to rebelliousness or independent judgement and action was correlated with poor blood glucose control (r=0.402, p<0.05).
ConclusionThe rebellious or non-conformist personality type is closely associated with poor blood glucose control in patients with DM1.
El diagnóstico de diabetes mellitus tipo1 (DM1) tiene un gran impacto en los jóvenes y sus familias. Los factores psicosociales, la motivación del paciente, la participación y la aceptación de la enfermedad son fundamentales para lograr un buen control glucémico. Nuestros objetivos fueron analizar los rasgos de personalidad y cómo se asocian con el control glucémico en pacientes con DM1.
MétodosSe estudiaron 62 pacientes adultos con DM1, con al menos un año de duración de la enfermedad y ausencia de complicaciones crónicas avanzadas. Se midieron parámetros clínicos, biológicos y de personalidad (índice Millon de estilos de personalidad [MIPS]).
ResultadosHubo correlaciones significativas entre diferentes variables de personalidad y hemoglobina glucosilada (HbA1c). Se observó peor control glucémico en pacientes con mayores puntuaciones en las escalas de perfil psicológico caracterizadas por un mayor enfoque en las emociones y los valores personales (53,6±25,7 vs 36,2±26,8; p=0,021), la tendencia al rechazo de ideas convencionales (36,7±24,1 vs 21.9±21,4; p=0,025), la aversión al cumplimiento de las normas y una preferencia por la autonomía (41,1±24,4 vs 15,6±16,6; p=0,001), autoconfianza lábil (41,5±25,1 vs 28,3±14,7; p=0,038) y desacuerdo expresado con los demás (37,5±27,5 vs 19,5±20,2; p=0,015). El análisis factorial basado en los componentes principales de la varianza arrojó cuatro factores. El factor caracterizado como relacionado con la rebeldía o el juicio y la acción independiente se correlacionaron con un control glucémico deficiente (r=0,402; p<0,05).
ConclusiónEl tipo de personalidad rebelde o inconformista está estrechamente asociado con un mal control glucémico en pacientes con DM1.
Type 1 diabetes mellitus 1 (DM1) is a metabolic disease characterised by the autoimmune destruction of beta cells, causing a deficit in insulin secretion and chronic increase in blood glucose levels. Chronic exposure to hyperglycaemia has serious consequences. In contrast, tight blood glucose control avoids or delays chronic microvascular complications,1 especially in younger patients at early stages of the disease,2 minimising costs both to the patients and to the health system.
The diagnosis of DM1 has a major impact on young people and their families, and can trigger a myriad of emotional responses. Continuous care and treatment is needed to prevent acute symptoms and to reduce the risk of chronic complications. To achieve this, it is necessary to have the full and active participation of the patient in the management of their disease.
Despite notable pharmacological advances and technological progress in the treatment of diabetes, less than one third of patients with DM1 achieve optimal metabolic control.3 Nonetheless, patient motivation, participation and acceptance of the disease are essential to achieve good blood glucose control.
Psychosocial factors include complex environmental, social, behavioural and emotional factors that influence living with diabetes. All of them have an important impact on achieving satisfactory medical outcomes and psychological well-being.4 Psychological variables involved in blood glucose control include intelligence, motivation, perceptiveness, interpersonal and decision-making skills, cognitive maturity level and the degree of control over the disease. Some of these variables have been predictors of future ketoacidosis.5 Different authors have proposed that psychosocial factors could influence poor outcomes in educational and therapeutic programmes on blood glucose control.6 For example, series of psychological risk factors for poorer blood glucose control have been proposed. Stress levels also affect metabolic control in diabetes regardless of the degree of treatment adherence.7
Lifestyle changes and treatment adherence are needed to achieve good metabolic control in diabetes mellitus. Thus, it is an excellent model to examine the effect of psychological variables on medical treatment. Stable personality traits could play a role in the degree of metabolic control. In fact, the close relationship between the patient's own behaviour, blood glucose control and associated medical complications prompt some authors to suggest a causal role for personality factors in determining adherence and blood glucose control behaviour.
Different personality traits have been associated with metabolic control evaluated by glycated haemoglobin (HbA1c). Extraversion, agreeableness, conscientiousness and sociability traits have been associated with good metabolic control.8 However, traits of neuroticism or negative mood tendencies have been variously associated with both good and poor control. In contrast, other studies have found that the erratic or dramatic personality cluster shows worse levels of blood glucose control, particularly noticeable in borderline personality disorder.9 Some attachment styles have been linked to higher HbA1c values. Within these interpersonal traits, an attachment style characterised by high self-confidence and low trust in others has been related to worse diabetic control. Alexithymia, which manifests as poor awareness and management of emotions, may also influence metabolic control, although results have been inconsistent.10
Thus, individual variables seem to be a mediating factor between adherence to medical treatment and good blood glucose control. It stands to reason that awareness of the differences between patients with good and poor blood glucose control can improve the doctor-patient relationship and thus treatment adherence. This indicates the need for more research on personality variables. Indeed, the literature shows that personality influences adherence to treatment. However, most research on the relationship between personality and blood glucose control in diabetic patients includes heterogeneous samples in which other factors such as age, insulin resistance, duration of diabetes, pancreatic reserves and the different antidiabetic guidelines used can affect treatment efficacy, and there could therefore be confounding associations between personality and blood glucose control.
Given the evident importance of behavioural factors in blood glucose control and the need to understand patients in order to encourage good control, the objective of this study was to analyse personality traits and how they are related with blood glucose control in patients with DM1.
Material and methodsSubjectsPatients with DM1 were consecutively recruited from our centre's Endocrinology and Nutrition Department. Inclusion criteria were patients with DM1 over 18 years of age, with at least one-year disease duration and absence of advanced chronic complications (blindness, need for laser therapy, macroalbuminuria, end-stage kidney failure, haemodialysis, amputation, neurological disability score (NDS)>7 or cardiovascular disease). All patients received the same standardised protocol for diabetes education in DM1 at our centre. To control for the influence of affective or thought disorders, patients diagnosed with severe psychiatric disorders or borderline personality disorder were excluded from the study, as were insulin pump users.
The study was carried out from November 2012 to January 2013. Sixty-nine consecutive patients with inadequate blood glucose control who attended our centre's diabetes referral unit were included in the study.
All of the patients included in the study were treated by the same endocrinologist and received identical diabetes education taught by the same educator. All of them were treated with multiple doses of insulin.
ProceduresAll data were collected by the same researcher in a specialist referral unit for DM1 patients. The same researcher briefed the patients about the study and instructed them on completing the personality questionnaire and the importance of filling it in without help. A deadline for submission to the hospital was set to avoid losing cases. The completed questionnaire was submitted by 95% of patients and no differences in social or medical variables were found between patients who chose to participate or not.
Patients who failed to submit the questionnaire by the indicated date were called by phone to remind them about the due date. The study and research protocol was approved by the hospital ethics committee. All of the patients gave written informed consent to participate.
Measurement methodsClinical and biological parametersClinical parameters including age (years old), disease duration (years since diabetes diagnosed), chronic complications (microalbuminuria and non-proliferative retinopathy), insulin treatment with multiple dose injection (MDI), active smoking, weekly physical activity (hours per week), carbohydrate counting, anthropometric measurements and blood pressure were all collected during the appointment by the same researcher. After clinical data was collected the questionnaire was handed out and a biochemical analysis was requested.
The measurement of HbA1c (%, mmol/mol) was performed using standardised laboratory techniques. The sample was divided using an HbA1c cut-off point of 8.0% in National Glycohemoglobin Standardization Program (NGSP) units, 64 mmol/mol in International Federation of Clinical Chemistry (IFCC) units. Subjects with HbA1c<8% were classed as having moderate blood glucose control and those with ≥8% as having poor blood glucose control. This cut-off point was established to emphasise that some personality traits can be associated with significantly high levels of control and not only moderate levels, as could be considered at 7–8%.
Patient self-monitoring of capillary blood glucose was also registered (number of checks per day).
Personality parametersThe Millon Index of Personality Styles (MIPS)11,12 was administered for personality assessment. It consists of 180 items using a true/false format and includes 24 scales grouped into 12 pairs, and each pair contains two bipolar scales. The 12 pairs are also arranged into three areas: Motivating Styles, Thinking Styles and Behaving Styles. In addition, the MIPS includes three validity indices: Positive Impression, Negative Impression and Consistency. The MIPS was adapted to and standardised for the Spanish population and was published in Spain.13 The internal consistency obtained in the Spanish population is satisfactory (α=0.72). In the group participating in this study, the α value was 0.73 for all the scales, ranging from 0.61 (for the Realistic/Sensing scale) to 0.82 (for Anxious/Hesitating scale).
Data analysisAll the analyses were performed with SPSS 11 for MacOsx. Results are expressed as mean±standard deviation. The p-values were two-tailed and a p-value of less than 0.05 was considered significant.
HbA1c was used as a categorical variableDue to the sample size and the measurement of variables that did not fulfil the criteria of normality, non-parametric tests were used. The Mann–Whitney test was used to assess differences in measured parameters between groups. Spearman's correlation was used to assess the degree of association between two quantitative variables. Qualitative variable comparison between groups was performed with the χ2 test. Regression analysis was performed in successive steps to calculate the variability of HbA1c explained by the personality variables. Factor analysis was applied to assess degree of association of personality profile with blood glucose control (HbA1c).
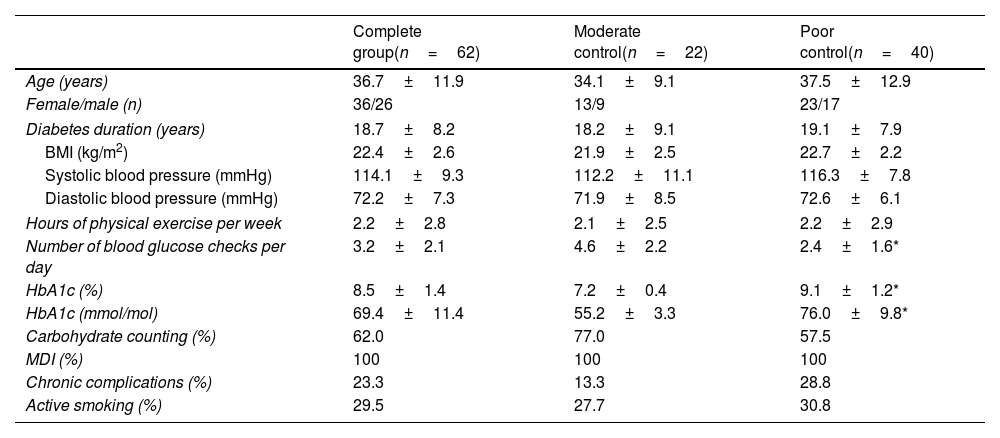
ResultsWe included 69 patients. Seven patients were excluded for non-compliance or non-submission of questionnaires. Finally, a total of 62 patients (58.1% female) were studied. Table 1 shows the clinical and biological characteristics of the patients included in the study. No statistically significant differences were found in the percentages in males and females (χ2=0.324, p=0.0569), age (t=−1.304, p=0.198), diabetes duration (t=−0.471, p=0.640), presence of chronic complications (χ2=9.832, p=0.631), smoking status (χ2=3.733, p=0.443) or carbohydrate counting (χ2=10.882, p=0.092) comparing moderate and poor blood glucose control groups. As expected, differences were found in the digital blood glucose testing variable between the moderate and poor blood glucose control groups (t=3.856, p<0.001) and HbA1c value.
Sociodemographic, clinical and biological characteristics of subjects with type 1 diabetes included in the study.
| Complete group(n=62) | Moderate control(n=22) | Poor control(n=40) | |
|---|---|---|---|
| Age (years) | 36.7±11.9 | 34.1±9.1 | 37.5±12.9 |
| Female/male (n) | 36/26 | 13/9 | 23/17 |
| Diabetes duration (years) | 18.7±8.2 | 18.2±9.1 | 19.1±7.9 |
| BMI (kg/m2) | 22.4±2.6 | 21.9±2.5 | 22.7±2.2 |
| Systolic blood pressure (mmHg) | 114.1±9.3 | 112.2±11.1 | 116.3±7.8 |
| Diastolic blood pressure (mmHg) | 72.2±7.3 | 71.9±8.5 | 72.6±6.1 |
| Hours of physical exercise per week | 2.2±2.8 | 2.1±2.5 | 2.2±2.9 |
| Number of blood glucose checks per day | 3.2±2.1 | 4.6±2.2 | 2.4±1.6* |
| HbA1c (%) | 8.5±1.4 | 7.2±0.4 | 9.1±1.2* |
| HbA1c (mmol/mol) | 69.4±11.4 | 55.2±3.3 | 76.0±9.8* |
| Carbohydrate counting (%) | 62.0 | 77.0 | 57.5 |
| MDI (%) | 100 | 100 | 100 |
| Chronic complications (%) | 23.3 | 13.3 | 28.8 |
| Active smoking (%) | 29.5 | 27.7 | 30.8 |
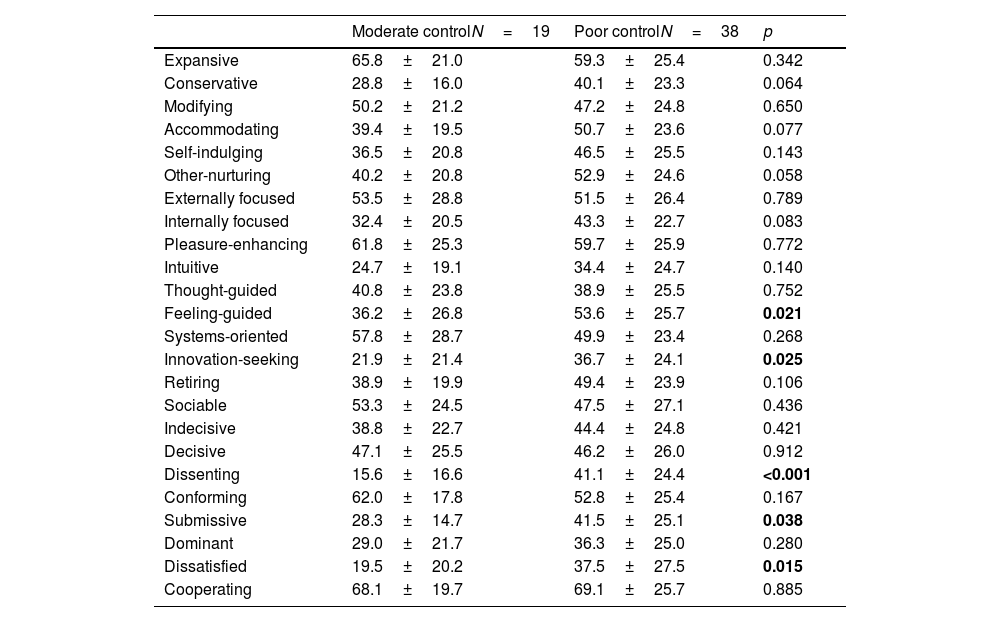
Significant correlations between different personality variables and HbA1c values were found (Table 2). Individuals with poor blood glucose control had significantly higher scores on the Feeling-guided, Innovation-seeking, Dissenting, Submissive and Dissatisfied scales (r=0.427; p 0.015). This psychological profile is characterised by greater focus on emotions and personal values (feeling-guided), the tendency to reject conventional ideas (innovation-seeking), an aversion to complying with norms and a preference for autonomy (unconventional/dissenting), labile self-confidence (submissive/yielding) and expressed disagreement with others (dissatisfied/complaining).
Differences between moderate (HbA1c <8%) and poor control.
| Moderate controlN=19 | Poor controlN=38 | p | |
|---|---|---|---|
| Expansive | 65.8±21.0 | 59.3±25.4 | 0.342 |
| Conservative | 28.8±16.0 | 40.1±23.3 | 0.064 |
| Modifying | 50.2±21.2 | 47.2±24.8 | 0.650 |
| Accommodating | 39.4±19.5 | 50.7±23.6 | 0.077 |
| Self-indulging | 36.5±20.8 | 46.5±25.5 | 0.143 |
| Other-nurturing | 40.2±20.8 | 52.9±24.6 | 0.058 |
| Externally focused | 53.5±28.8 | 51.5±26.4 | 0.789 |
| Internally focused | 32.4±20.5 | 43.3±22.7 | 0.083 |
| Pleasure-enhancing | 61.8±25.3 | 59.7±25.9 | 0.772 |
| Intuitive | 24.7±19.1 | 34.4±24.7 | 0.140 |
| Thought-guided | 40.8±23.8 | 38.9±25.5 | 0.752 |
| Feeling-guided | 36.2±26.8 | 53.6±25.7 | 0.021 |
| Systems-oriented | 57.8±28.7 | 49.9±23.4 | 0.268 |
| Innovation-seeking | 21.9±21.4 | 36.7±24.1 | 0.025 |
| Retiring | 38.9±19.9 | 49.4±23.9 | 0.106 |
| Sociable | 53.3±24.5 | 47.5±27.1 | 0.436 |
| Indecisive | 38.8±22.7 | 44.4±24.8 | 0.421 |
| Decisive | 47.1±25.5 | 46.2±26.0 | 0.912 |
| Dissenting | 15.6±16.6 | 41.1±24.4 | <0.001 |
| Conforming | 62.0±17.8 | 52.8±25.4 | 0.167 |
| Submissive | 28.3±14.7 | 41.5±25.1 | 0.038 |
| Dominant | 29.0±21.7 | 36.3±25.0 | 0.280 |
| Dissatisfied | 19.5±20.2 | 37.5±27.5 | 0.015 |
| Cooperating | 68.1±19.7 | 69.1±25.7 | 0.885 |
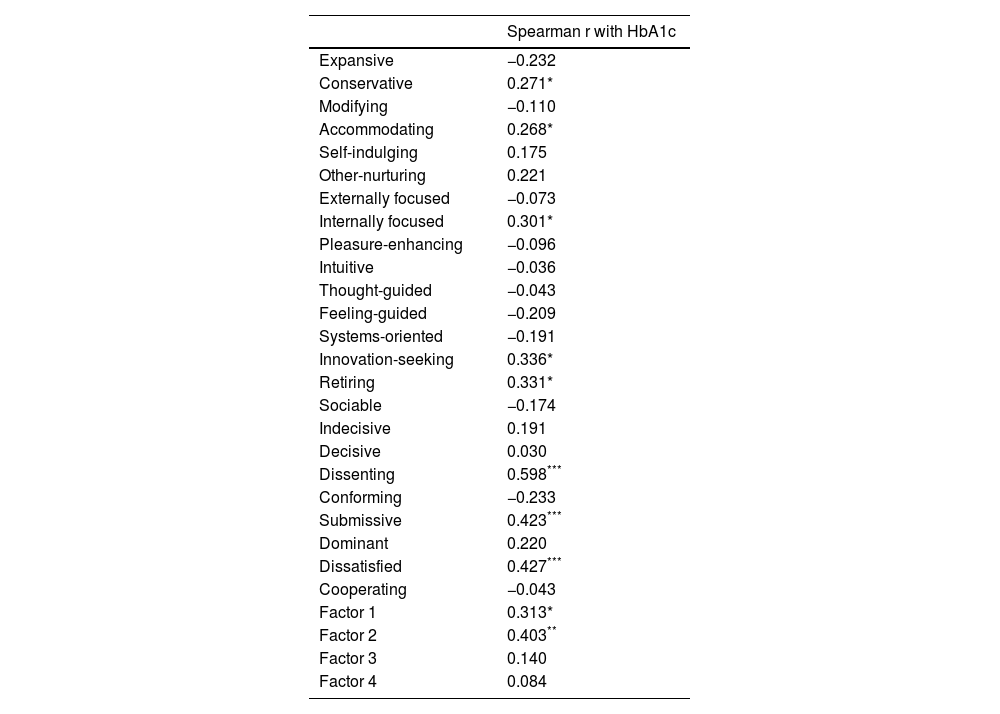
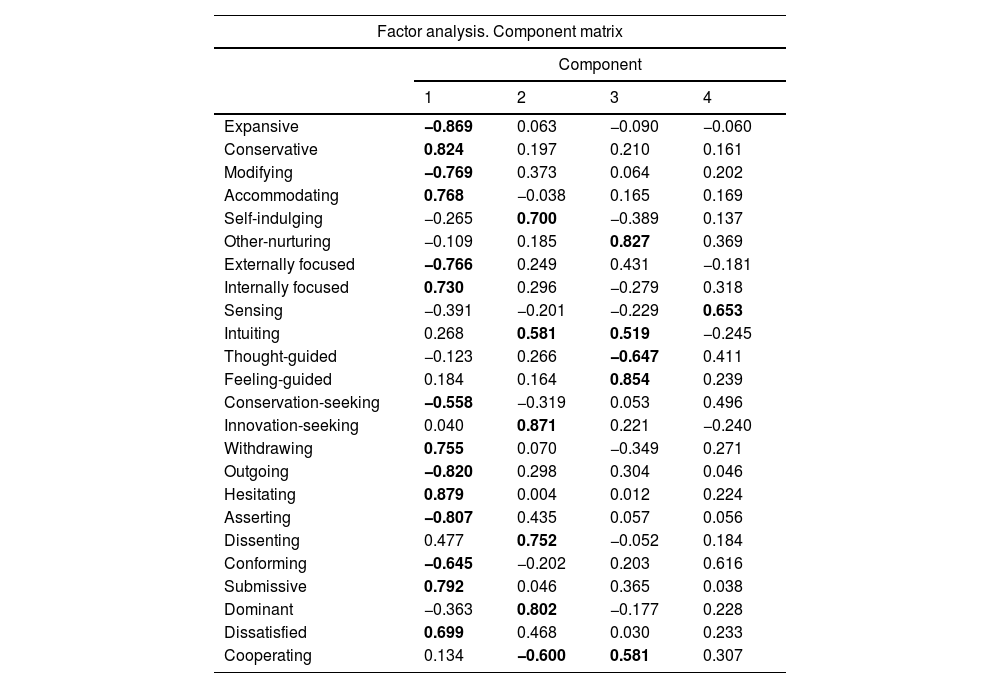
Factor analysis based on the main components of the variance (Tables 3 and 4) yielded four factors. Factor 1 shows correlations with Millon's adaptive variables that represent the index of psychological adjustment; this factor principally indicates degree of psychological maladjustment, as evidenced by a correlation close to 1 (r=−0.956, p<0.001) of the adjustment index with factor 1. It also correlated with Hb1Ac (r=0.313, p<0.05).
Factor analysis based on the main components of the variance.
| Spearman r with HbA1c | |
|---|---|
| Expansive | −0.232 |
| Conservative | 0.271* |
| Modifying | −0.110 |
| Accommodating | 0.268* |
| Self-indulging | 0.175 |
| Other-nurturing | 0.221 |
| Externally focused | −0.073 |
| Internally focused | 0.301* |
| Pleasure-enhancing | −0.096 |
| Intuitive | −0.036 |
| Thought-guided | −0.043 |
| Feeling-guided | −0.209 |
| Systems-oriented | −0.191 |
| Innovation-seeking | 0.336* |
| Retiring | 0.331* |
| Sociable | −0.174 |
| Indecisive | 0.191 |
| Decisive | 0.030 |
| Dissenting | 0.598*** |
| Conforming | −0.233 |
| Submissive | 0.423*** |
| Dominant | 0.220 |
| Dissatisfied | 0.427*** |
| Cooperating | −0.043 |
| Factor 1 | 0.313* |
| Factor 2 | 0.403** |
| Factor 3 | 0.140 |
| Factor 4 | 0.084 |
Factor analysis results.
| Factor analysis. Component matrix | ||||
|---|---|---|---|---|
| Component | ||||
| 1 | 2 | 3 | 4 | |
| Expansive | −0.869 | 0.063 | −0.090 | −0.060 |
| Conservative | 0.824 | 0.197 | 0.210 | 0.161 |
| Modifying | −0.769 | 0.373 | 0.064 | 0.202 |
| Accommodating | 0.768 | −0.038 | 0.165 | 0.169 |
| Self-indulging | −0.265 | 0.700 | −0.389 | 0.137 |
| Other-nurturing | −0.109 | 0.185 | 0.827 | 0.369 |
| Externally focused | −0.766 | 0.249 | 0.431 | −0.181 |
| Internally focused | 0.730 | 0.296 | −0.279 | 0.318 |
| Sensing | −0.391 | −0.201 | −0.229 | 0.653 |
| Intuiting | 0.268 | 0.581 | 0.519 | −0.245 |
| Thought-guided | −0.123 | 0.266 | −0.647 | 0.411 |
| Feeling-guided | 0.184 | 0.164 | 0.854 | 0.239 |
| Conservation-seeking | −0.558 | −0.319 | 0.053 | 0.496 |
| Innovation-seeking | 0.040 | 0.871 | 0.221 | −0.240 |
| Withdrawing | 0.755 | 0.070 | −0.349 | 0.271 |
| Outgoing | −0.820 | 0.298 | 0.304 | 0.046 |
| Hesitating | 0.879 | 0.004 | 0.012 | 0.224 |
| Asserting | −0.807 | 0.435 | 0.057 | 0.056 |
| Dissenting | 0.477 | 0.752 | −0.052 | 0.184 |
| Conforming | −0.645 | −0.202 | 0.203 | 0.616 |
| Submissive | 0.792 | 0.046 | 0.365 | 0.038 |
| Dominant | −0.363 | 0.802 | −0.177 | 0.228 |
| Dissatisfied | 0.699 | 0.468 | 0.030 | 0.233 |
| Cooperating | 0.134 | −0.600 | 0.581 | 0.307 |
Bold indicates statistically significant (p<0.05).
Factor 2 was saturated with the self-indulgence, intuition, innovation-seeking, dissenting, dominant and low cooperation variables. This establishes a profile of emotional independence, a feeling-guided thinking style, and rejection of traditional ways of thinking, a tendency towards innovation and novelty, and a behaving style that favours showing displeasure or expressing differences dominantly. They are guided by their own rules, with low preference for agreeing with others or being pleasant and cooperative. This profile could therefore be characterised as related to rebelliousness or independent judgement and action. This factor was correlated with poor blood glucose control (r=0.402, p<0.05).
DiscussionThe psychological profile is established during adolescence and emerging adulthood when cognitive, developmental and emotional changes occur. Ongoing assessment of psychosocial status and distress in the patient with DM1 and the caregiver during visits is essential.14–16
The psychological traits of individuals with poor blood glucose control could be defined as having a rebellious, irreverent adaptive style, which seeks intellectual independence and shuns conventions and externally imposed rules. This could be difficult to reconcile with following rules and maintaining strict blood glucose control, probably because patients of this type are not a good match with the traditional paternalistic doctor-patient relationship present in our clinical environment. This maladaptive style clashes with the need to conform and adapt to the viewpoints or indications of authority figures (doctors, educators, etc.) or follow the advice of others, despite a lack of evident complications in the short term. It also makes it more difficult to reach agreements with those around them regarding adherence to diet, physical activity, exercise, healthy lifestyle, self-control and the therapeutic requirements that facilitate blood glucose control. We propose that personality and blood glucose control can be both directly and indirectly related, in several ways.
One major way in which personality has previously been linked to good or poor blood glucose control is via certain psychological and emotional mechanisms that hamper ability to control. One of the principal personality variables studied in relation to blood glucose control is neuroticism. Previous studies in adolescents with type 1 diabetes showed that patients with negative affect, or a tendency to express negative emotions, had worse HbA1c values, as did children who experienced more intense reactions in relation to stress management.17
Another proposed pathway of influence relates indirectly to poor blood glucose control through maladaptive behaviour in the patient. Personality styles centred more on themselves or on others have been suggested as variables influencing blood glucose control. The tendency towards poorer self-care has been shown to worsen blood glucose control and increase the risk of complications. There is evidence that patients with diabetes who are more focused on the needs and preferences of others and who score high in altruism have higher levels of HbA1c.18 Following on from this, personality traits such as emotional instability or fluctuating self-esteem, which show rapid switches from omnipotence to deflation, the need to cling to significant others for support and advice, lack of impulse control, and low anxiety tolerance appear related to poorer blood glucose control.19,20
We found higher scores in other-nurturing in poorly controlled patients. However, patients with better control were not found to score higher in self-indulgence. This would refine the hypothesis regarding self-care to a theory that greater dependence on others can negatively affect autonomous activities like controlling diet, or calculating and administering insulin, in everyday situations when help to handle the complex interaction of factors involved in insulin therapy is not always available from others. This is more evident in patients with DM1, who depend exclusively on externally administered insulin. Thus, moderate levels of self-indulgence seem to benefit patients with diabetes.18 Nonetheless, an excess of self-indulgence can also lead to overly self-sufficient behaviours, and a lower tolerance for externally imposed rules or adaptation to the strict control regimes necessary in many day-to-day activities to ensure optimal blood glucose control, as we have seen in this attachment style and its relationship with poorer blood glucose control behaviour.19
Another way in which personality could be related to poor diabetes management is through the patient's behaviour regarding variables that modulate blood glucose levels. It has been suggested that personality modifies behaviour patterns and therefore determines blood glucose control, which in turn influences certain complications such as kidney deterioration.21 One characteristic studied in treatment adherence is locus of control and self-efficacy, which has been associated with better blood glucose control22 in subjects with DM1,23 and also with disrupted interpersonal relationships, related to developing eating disorders such as binge eating, which is linked to poor diabetic control.5 In our case, the submissive behaviour style of patients with poor blood glucose control is in line with previous findings. This suggests that submissive and self-deprecating behaviour may reduce capacity for interpersonal control and weaken the resolve to undertake the practices related with autonomous control of the disease and feelings of self-efficacy and internal control.
In the group of poor blood glucose control subjects, we found other personality variables that represent a rebellious style: independent judgement and rejection of pre-established rules and ways of thinking, as suggested by higher scores in dissenting, dissatisfied and innovation-seeking than those with good control. Our results indicate that the type of treatment established for blood glucose control, based on doctors presenting unilateral information and setting restrictive behavioural standards, seems to be a risk factor for poor blood glucose control in people with diabetes (type 1 diabetes in our study) with an adaptive style leaning more towards independent thought and expressed dissent or disagreement.
The two styles, one the patient's own style and the other a different style required by the treatment, thus come into conflict. In light of this, it is unsurprising that individuals with the best blood glucose control are more conformist, are less inclined to express disagreement or reject external or more traditional concepts or customs. An awareness of patients’ psychological characteristics would therefore seem necessary to reshape interventions around the patient's own wishes and needs,24 as ultimately they are the ones who must manage the disease.
These results tie together with interventions based on motivational interviewing as part of diabetes treatment,25 treatments based around patient's autonomy and personal choice which have produced positive outcomes in diabetes patients, both type 126 and type 2.27 Thus, sharing decisions with patients regarding the adoption of regimen components and self-management behaviours can improve diabetes self-efficacy, adherence and metabolic outcomes.4
Differences between patients with good and poor control could be due to certain biological aspects of diabetes, making it more difficult for some patient groups than others to control the disease, despite the same adherence to treatment. This is generally true for both type 1 and type 2 diabetes which, in aetiopathogenic terms, are two distinct entities. In addition, the degree of insulin dependence between patients could bias data in patients with lower pancreatic insulin reserves or higher insulin resistance rates, due to various factors such as weight. However, unlike type 2 diabetes, type 1 diabetes depends exclusively on external blood glucose control. Therefore, as all the patients in our sample were being treated in our diabetes unit by trained medical and nursing staff, all were on treatment with multiple subcutaneous insulin dosage, and none were using an insulin pump, ultimately all blood glucose control must be attributed to patient behaviour, which in turn is very likely based on personality. Psychosocial factors are significantly associated with self-management difficulties, suboptimal blood glucose control, reduced quality of life, and higher rates of acute and chronic diabetes complications.28
However, our study has some limitations. First, we only included a small number of subjects. Furthermore, an important limitation of the study is the fact that to determine the level of blood glucose control we only used HbA1c. Nowadays there are widely available continuous monitoring systems that could help to expand the information with other metrics. However, when we performed the study these new devices were not available. It may be interesting in future studies to analyse the relationship between personality traits and the use of digital devices (frequency of readings, blood glucose control results, etc.) and their impact on blood glucose control.
In conclusion, in our study, conducted in patients with DM1 with poor metabolic control, the rebellious or non-conformist personality style is closely associated with poor blood glucose control. Therefore, personality plays an important role in blood glucose control in DM1. More studies are necessary to determine whether or not psychological intervention combined with increased independence in these patients could be helpful to improve blood glucose control.
Authors’ contributionsWCGH and RM-B devised the project, designed the study and interpreted and analysed the data. JF, FJAB, MP, EB, SM-H and JTR collected and interpreted the data and analysed the data. MJS performed the measurements. All authors discussed the results and contributed to the final manuscript. All authors have read and approved the final manuscript.
Consent to participateAll authors consent to participate.
Consent for publicationAll authors consent for publication.
FundingThis study was supported by a grant from Centro de Investigación Biomédica en Red (CIBER) de Diabetes y Enfermedades Metabólicas Asociadas (CIBERDEM) [Network Centre for Biomedical Research on Diabetes and Associated Metabolic Diseases], Instituto de Salud Carlos III (ISCIII) [Carlos III Health Institute]. CIBERDEM is an ISCIII initiative.
Sergio Martinez-Hervas is an investigator in the ‘Juan Rodes’ programme (JR18/00051) financed by the Instituto de Salud Carlos III and the European Regional Development Fund (ERDF).
Conflict of interestNone of the authors has any conflicts of interest or competing interests.
We thank the patients for their cooperation.