Edited by: Dr. Calos Cerdán
Cirugía General y Aparato Digestivo. Unidad de Cirugía Digestiva. Hospital Universitario de la Princesa. Madrid
Dr. Matteo Frasson
Cirugía general. Hospital Universitario y Politécnico La Fe. Valencia
Last update: November 2025
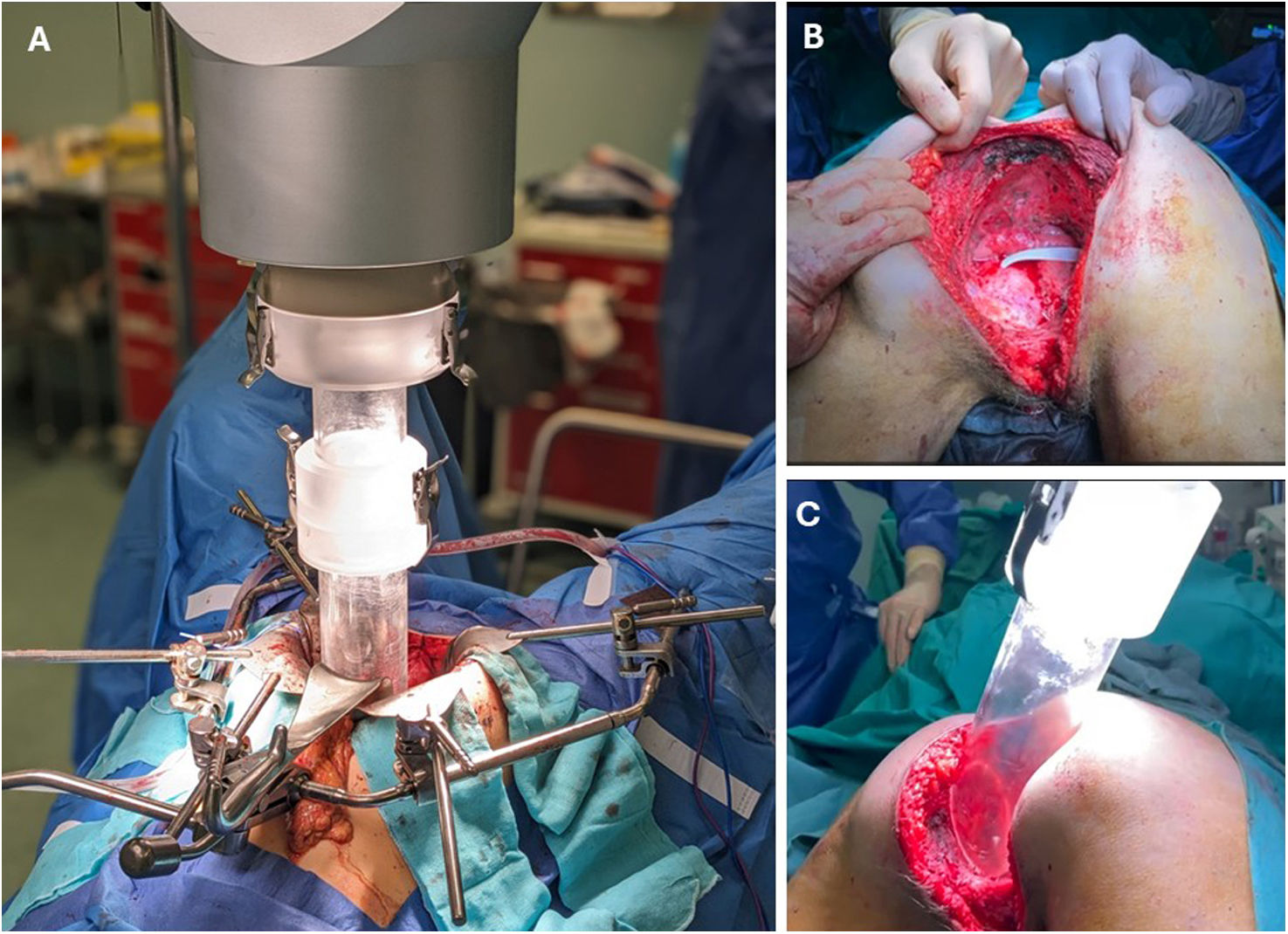
More infoPelvic exenteration (PE) is a potentially curative surgical option for patients with locally advanced rectal cancer (LARC) orlocallyrecurrent rectal cancer (LRRC) involvingmultivisceralstructures. Originally conceived as a palliative procedure, advancements in surgical techniques and multidisciplinary management have broadened its indications, enabling R0 resections in over 60% of cases. Appropriate patient selection, based on advanced imaging and comprehensive functional assessment, is essential to optimize oncologic outcomes. Currently, the surgical indication is primarily determined by the reasonable possibility of achieving an R0 resection with acceptable morbidity in a suitable candidate, which may translate into high survival rates. Surgical planning should follow a compartmental approach and require close collaboration among colorectal, urologic, gynecologic, vascular, orthopedic, plastic, and reconstructive surgeons. Urinary, gynecologic, vascular, osseous, and soft tissue reconstructions are tailored to the tumour’s extent and the patient's individual needs. In selected cases, PE may be performed with palliative intent. Intraoperative radiotherapy (IORT) and minimally invasive approaches have emerged as valuable adjuncts. Long-term oncologic and functional outcomes are closely linked to the achievement of negative margins. While postoperative morbidity remains significant, mortality rates have declined in high-volume centres. Postoperative quality of life has become a key outcome, with increasing emphasis on patient-reported outcome measures (PROMs) to guide clinical decision-making. PE continues to challenge traditional limits of resectability, offering renewed hope to carefully selected patients.
La exenteración pélvica (EP) representa una opción terapéutica potencialmente curativa para pacientes con cáncer de recto localmente avanzado (LARC) o recurrencia local (LRRC) con afectación multivisceral. Inicialmente concebida como un procedimiento paliativo, los avances técnicos y el enfoque multidisciplinar han ampliado sus indicaciones, permitiendo resecciones R0 en más del 60% de los casos. La correcta selección de pacientes, basada en estudios de imagen avanzados y una valoración funcional integral, es esencial para maximizar los beneficios oncológicos. En la actualidad, el límite de la indicación quirúrgica se establece en la posibilidad razonable de lograr una resección oncológica completa (R0) con una morbilidad aceptable en el paciente adecuado, lo que puede traducirse en tasas elevadas de supervivencia. La cirugía debe abordarse de forma compartimental y con la colaboración de múltiples especialidades. La reconstrucción urinaria, ginecológica, vascular, ósea y de tejidos blandos se adapta a la extensión tumoural y las necesidades del paciente. En casos seleccionados, la EP puede utilizarse con intención paliativa. La radioterapia intraoperatoria (IORT) y la cirugía mínimamente invasiva han demostrado ser estrategias complementarias prometedoras. Los resultados oncológicos y funcionales dependen en gran medida de la obtención de márgenes negativos. Aunque la morbilidad puede ser elevada, las tasas de mortalidad han disminuido en centros especializados. La calidad de vida posoperatoria se ha convertido en un parámetro clave, destacando el papel de las medidas reportadas por los pacientes (PROMs) en la toma de decisiones. La EP continúa desafiando los límites tradicionales de la resecabilidad, ofreciendo esperanza a pacientes seleccionados.