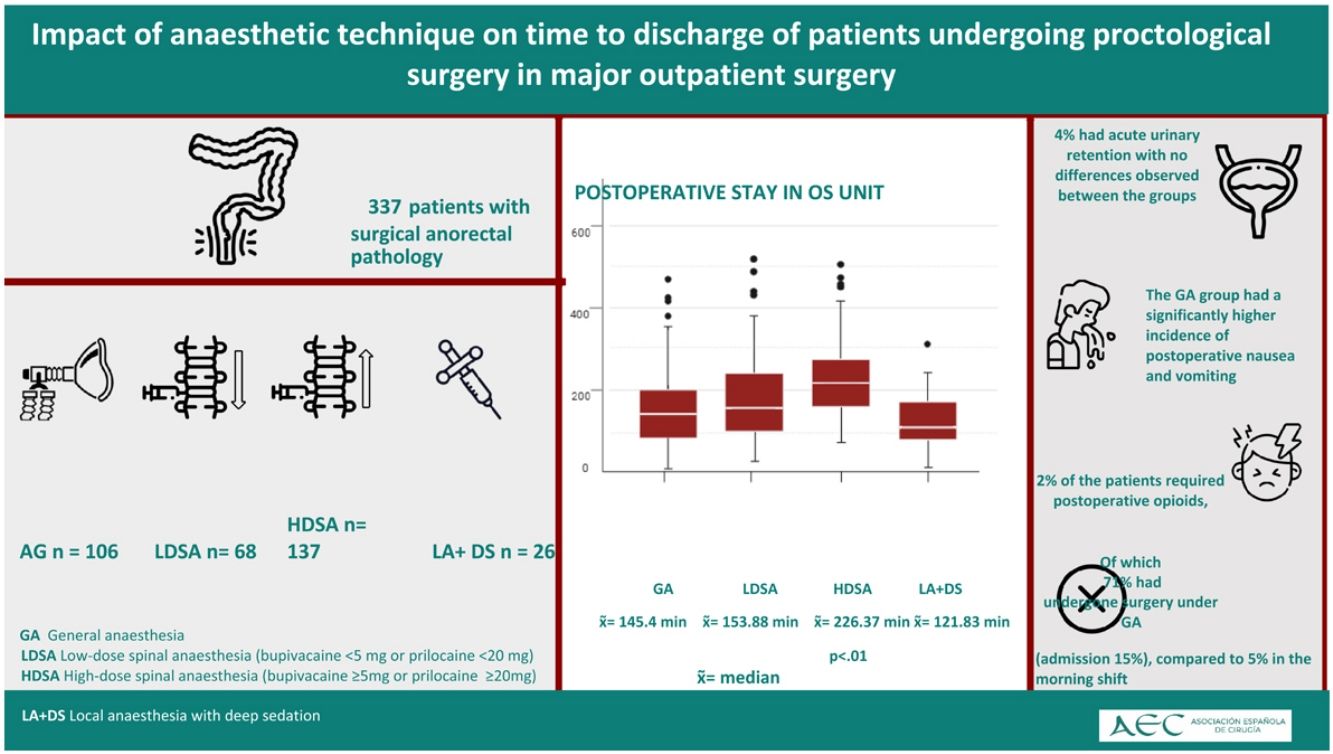
The present study aims to compare the length of postoperative stay in outpatient surgery (OS) setting of patients undergoing anorectal surgery in four different anaesthetic techniques: local anaesthesia with deep sedation (LA + DS), low-dose spinal anaesthesia (LDSA) (less than 5 mg of hyperbaric bupivacaine or less than 20 mg of hyperbaric prilocaine), high-dose spinal anaesthesia (HDSA), and general anaesthesia (GA). Secondary outcomes include analysing postoperative complications and their relationship with the chosen anaesthetic technique.
MethodsRetrospective observational study of patients who underwent scheduled proctological surgery between January 2018 and September 2021. Patients were classified into four groups according to the anaesthetic technique used. The primary outcomes were the length of stay in AS, the need for postoperative opioids, postoperative nausea and vomiting, acute urinary retention, and failure to complete the AS regimen (unscheduled admission to the ward or visit to the emergency room in the first 24 h with or without hospital admission).
ResultsOut of 337 patients, 137 (40.4%) received HDSA, 68 (20.5%) LDSA, 106 (31.3%) GA, and 26 (7.7%) LA + DS. The longest median stay (226 min) was associated with HDSA (p < 0.001). The shortest time was recorded with LA + DS (121 min). Around 2% required opioids. 71% of them were operated under GA (p = 0.06). AUR occurred in 4% of patients, with no significant differences between groups. The rate of PONV was 74% in the GA group compared to 7–19% in the rest of the groups. A higher OS failure rate (15%) was observed in afternoon shifts compared to 5% in morning shifts.
ConclusionsIn ambulatory proctological surgery, spinal anaesthesia with doses less than 5 mg of bupivacaine or 20 mg of hyperbaric prilocaine is effective and reduces postoperative stay times. General anaesthesia is associated with a higher incidence of nausea, vomiting, and increased need for postoperative opioids.
Se han comparado los tiempos de estancia postoperatoria en cirugía mayor ambulatoria (CMA) tras una cirugía proctológica utilizando 4 técnicas anestésicas: anestesia local con sedación profunda (AL + S), anestesia raquídea a dosis bajas (RDB) (< 5 mg de bupivacaína o < 20 mg de prilocaína hiperbáricas), anestesia raquídea a dosis altas (RDA) y anestesia general (AG). Los objetivos secundarios incluyen análisis de las complicaciones postoperatorias y su relacion con la técnica anestésica seleccionada.
MetodologíaEstudio observacional retrospectivo sobre pacientes sometidos a cirugía proctológica programada entre 1/2018 y 9/2021. Los pacientes se clasificaron en 4 grupos según la técnica anestésica. Las variables principales fueron el tiempo de estancia en CMA, necesidad de opioides postoperatorios, náuseas y vómitos postoperatorios, retención aguda de orina (RAO) y fallo en el régimen CMA (ingreso en planta no programado o visita a urgencias en las primeras 24 horas con o sin ingreso hospitalario).
ResultadosDe 337 pacientes, 137 (40,4%) recibieron RDA, 68 (20,5%) RDB, 106 (31,3%) AG y 26 (7,7%) AL + S. La mediana más alta de estancia (226 min) correspondió a la anestesia raquídea a dosis altas (p < 0.001). El menor tiempo se registró con AL + S (121 minutos). Un 2% requirió opioides, siendo el 71% intervenido bajo AG (p = 0.06). Un 4% presentó RAO sin diferencias entre los grupos. La tasa de NVPO fue del 74% en el grupo AG frente a un 7-19% en el resto de los grupos. Se observó un mayor fallo de CMA (15.3%) en turno de tarde frente al 5.3% en el de mañana.
ConclusionesEn cirugía proctológica en CMA, la anestesia raquídea con dosis menores a 5 mg de bupivacaína o 20 mg de prilocaína hiperbárica es eficaz y reduce los tiempos de estancia postoperatoria. La anestesia general está asociada con una mayor incidencia de náuseas, vómitos y mayor necesidad de opioides postoperatorios.