Introduction
Breastfeeding and its possible ability to prevent different types of infection have been the subject of many studies. In developing countries little doubt remains as to its efficacy in lowering the incidence of these processes.1-8 In similar studies done in industrialized countries, however, the results have been contradictory.9-13 A number of possible explanations have been suggested for this variability, eg, biases in the study design (especially selection and reverse causality bias), absence of control for potential confounding factors,14-16 and small sample number.
One recent community-level study showed breastfeeding (BF) to have a protective effect against different types of infection, both when it was the only form of feeding and when it was combined with artificial feeding (AF) (ie, mixed feeding, MF).17 These findings suggest that it would be useful for clinical purposes to analyze the combined effect of both types of infant feeding in comparison with AF. It should be remembered that in fact, a large percentage of mothers currently use MF.
No studies in Spain have tested these hypotheses while controlling for the main confounders that might influence the association.
The present study was designed with two aims in mind:
Main objective
To determine whether breastfeedingalone or in combination with AF (MF)--during the first 6 months of life leads to a decrease in the incidence of upper (URTI) and lower respiratory tract infections (LRTI) during the first year of life, in comparison with AF alone, in babies younger than 12 months of age, born at term and seen at a primary care center.
Secondary objective
To establish the influence of other factors (attending day care, family antecedents of atopy, father´s and mother´s smoking habit, parents´ level of education, and number of persons in the household) on these infections.
Participants and methods
Type of design
Historical cohort design.
Participants
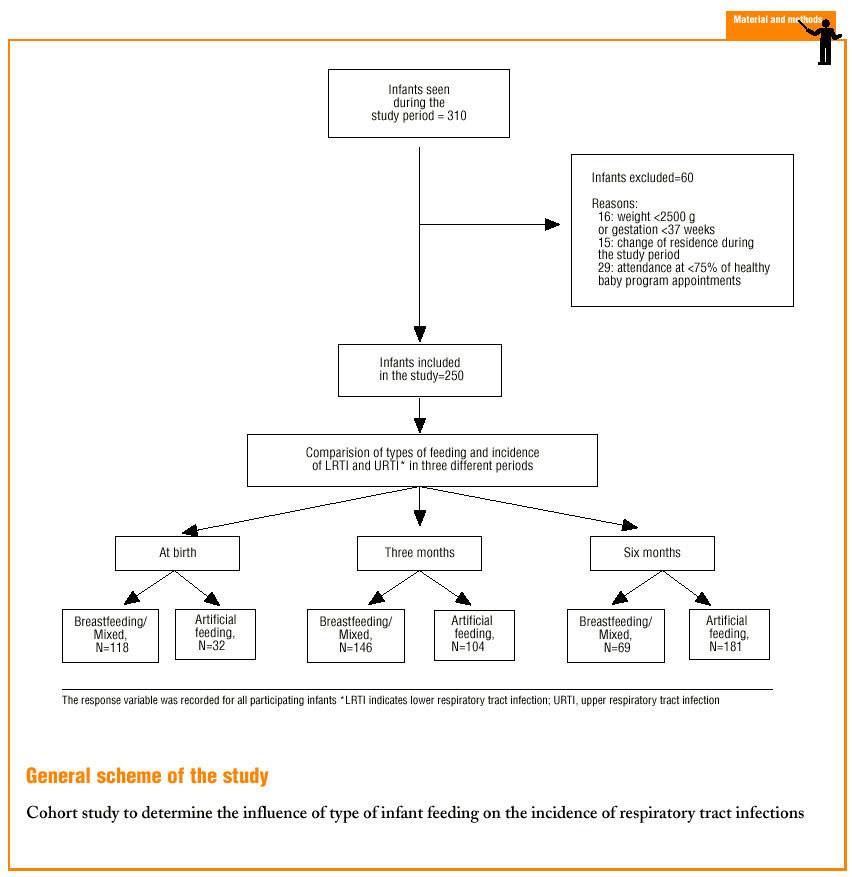
Inclusion criteria: a) children born between 1 October 1994 and 1 February 1998; b) current medical record available at a participating primary care center; c) attendance of at least 6 of 8 scheduled appointments in a Healthy Baby Program (HBP) during the first year of the infant´s life; d) residence within the basic health area involved in the study during the infant´s first year of life, e) birth weight >=2500 g; f) duration of gestation >=37 weeks.
Exclusion criteria: a) habitual residence outside the basic health area at any time during the study; b) underlying chronic respiratory, cardiovascular, neuromuscular or immunodeficient disease that might predispose the child to other infectious processes.
Sample size: During the study period new medical records were started for 310 infants in our basic health area. 60 babies were excluded for the following reasons: weight <2500 g or gestation <37 weeks (16 infants), change in habitual residence to an address outside the basic health area (15 infants), attendance at fewer than 75% of the HBP appointments (29 infants). The final sample size was 250; 80.6% of the babies were born during the study period. The participants were recruited at the age of approximately 15 days, in the course of their first appointment in the HBP, by consecutive sampling.16
Description of the variables
Study factor. The participants were divided into two groups depending on the type of feeding. Infants in BF group were breastfed exclusively or in combination with formula feeding (MF). The duration of BF was recorded in months (quantitative variable). Infants in AF group received artificial feeding only; the duration of AF was also recorded in months (quantitative variable).
Response variable. During the first 2 years of life the most frequent LRTIs are bronchiolitis and pneumonia. In this age group the similarities in the clinical manifestations of these two entities make them difficult to distinguish. Each is defined below, although the two were lumped together for the statistical analysis.
Bronchiolitis: inflammatory process of the lower respiratory tract characterized by bronchospasm, edema and bronchial hypersecretion, producing obstruction of the bronchioles. Clinical manifestations are generalized wheezing and cough on auscultation. Other symptoms (tachypnea, fever, general malaise and vomiting) may or may not accompany the signs detected on auscultation.
Pneumonia: fever, clinically evident respiratory symptoms (cough), physical examination compatible with the diagnosis (localized or disseminated crackles in either of both sides of the chest), or any combination of the above; diagnosis confirmed by chest x-ray and radiologist´s report.
Lower respiratory tract infection: considered the presence of any of the clinical pictures described above (bronchiolitis, pneumonia). This variable was recorded as cumulative incidence (number of new cases of IRTI during a given period/population at risk for IRTI). Cumulative incidence was determined for the ages of 0-3 months, 4-6 months and 7-12 months. All diagnoses noted in the medical record as bronchitis, bronchiolitis, pneumonia or lower respiratory tract infection were recorded for the purpose of the present analysis as LRTI. Visits to the center that took place within #<10 days of each other were considered to represent a single process, and thus a single episode of use (except in those cases when a different disease or disorder included in the present study was diagnosed). Visits that took place >10 days apart were considered to represent different processes.
Upper respiratory tract infections: considered all processes noted in the medical record as upper respiratory airway cold, laryngitis, tonsillitis, pharyngitis and rhinitis. As for LRTI, this variable was recorded as the cumulative incidence. The cumulative incidence of URTI was determined for the ages of 0-3, 4-6 and 7-12 months. Visit to the center that took place within #<10 days of each other were considered to represent a single process, and thus a single episode. Visits that took place >10 days apart were considered to represent different processes.
Potential confounding or effect-modifying variables. The variables considered potential confounders or effect modifiers19 are described below.
Day care attendance, recorded as a dichotomous variable (yes/no).
Parental antecedents of atopic processes, recorded as a dichotomous variable: bronchial asthma (yes/no), allergic rhinitis (yes/no), allergy testing (prick tests) (yes/no). For logistic regression analysis of the variable «atopy,» babies without antecedents were assigned a value of 0, and those with personal antecedents in one or both parents were assigned a value of 1.
Exposure to cigarette smoke: recorded separately for each parent as a quantitative (number of cigarettes/day) and a qualitative variable (smoker/nonsmoker).
Educational level: recorded as primary (up to eighth grade), secondary (technical, general or university track) or higher (university). University-level education was scored as 0, secondary education was scored as 1, and primary education was scored as 2. For logistic regression analysis, a value of 0 was assigned when the sum of the scores for both parents was #<2, and a value of 1 was assigned when the sum of the scores was #>3. For single-parent families (5 cases) the parent who brought the child to the center was questioned about the other parent´s educational level.
Number of persons in the household was recorded as the number of persons living together with the child in the same dwelling.
Mother´s age was recorded in years.
The response variables (cumulative incidence of LRTI and URTI) were recorded independently by two researchers who were unaware of the participants´ exposure status regarding the independent variables (type of feeding, potential confounders). Two other researchers who were unaware of the results for the response variables recorded the independent variables. This diminished the possibility of introducing bias due to prior knowledge of exposure status or disease status.
Sources of information
Data on type of feeding. This information was obtained from the record sheets for all scheduled appointments in the HBP, and from the information on body weight obtained by the nursing service and included in the child´s medical record.
Data on episodes of infection. a) clinical course sheets from all medical records were reviewed; b) reports given to the patient after an emergency visit to the health center. These reports are then given to the pediatrician or primary care physician at the next scheduled appointment. c) reports given to the patient after an emergency visit to the reference hospital.
Statistical analysis
Bivariate analysis. Parametric tests (Student-Fisher´s t test) for comparison of the means. The magnitude of the effect between different groups was expressed as relative risk (RR) with 95% confidence intervals (95% CI).
Logistic regression analysis. This technique was used to analyze the relationship between type of feeding and the dependent variables (LRTI and URTI). For this analysis, the dependent variables were transformed into dichotomous variables (0 episodes of LRTI vs >=1 episodes, 0 episodes of URTI vs >=1 episodes). Logistic regression made it possible to control for confounding variables and to take effect-modifying variables into account. The results were expressed as the odds ratio (OR) and 95% CI. An OR <1 indicated a protective effect of BF.20
Results
Three comparisons were used: at birth, 3 months and 6 months of age. Type of feeding was compared with the incidence of respiratory infections during the period immediately afterward, ie, type of feeding at birth was compared with the incidence of infections during the period from 0 to 3 months, feeding at 3 months with infections from 4 to 6 months, and feeding at 6 months with infections from 7 to 12 months. This type of analysis made it possible to control for reverse causality bias.14-16 Tables 1, 2 and 3 show the distribution of independent variables with respect to the main study variable (type of feeding) at birth, at 3 months and at 6 months of age.
The relation between type of feeding at birth and the incidence of LRTI and URTI during the first 3 months of life is shown in Table 4. There was a significant relationship between the number of persons in the household and the incidence of LRTI (OR, 1.87; 95% CI, 1.18-2.95). There was also a significant relationship between familial antecedents of atopy and increased incidence of LRTI (OR, 2.96; 95% CI, 1.19-7.40). No association was detected for smoking habit, parents´ educational level or mother´s age (all 95% CI included the value of 1). There was no association between the incidence of LRTI and smoking, parents´ educational level, mother´s age, number of persons in the household, familial antecedents of atopy, or day care use (all 95% CI included the value of 1).
The relationship between type of feeding at 3 months and the incidence of LRTI and URTI during the period from 4 to 6 months of age is shown in Table 5. There was a significant relationship between the number of persons in the household and the incidence of LRTI (OR, 1.62; 95% CI, 1.07-2.44). The relationship between day care use and an increased incidence of LRTI was also significant (OR, 4.52; 95% CI, 1.20-17.10). No associations were detected for smoking, parents´ level of education, mother´s age or familial antecedents of atopy (all 95% CI included the value of 1). The incidence of URTI was not associated with smoking, parent´s level of education, mother´s age, number of persons in the household, familial antecedents of atopy or day care attendance (all 95% CI included the value of 1).
The relationship between type of feeding at 6 months and the incidence of LRTI and URTI during the period from 7 to 12 months is shown in Table 6. There was no association between the incidence of LRTI and smoking, parents´ educational level, mother´s age, number of persons in the household, familial antecedents of atopy, or day care attendance (all 95% CI included the value of 1). Nor was there any association between the incidence of URTI and smoking, parents´ educational level, mother´s age, number of persons in the household, familial antecedents of atopy or day care attendance (all 95% CI included the value of 1).
Discussion
In this study no protective effect of BF was found in comparison with AF in decreasing the incidence of LRTI or URTI. These results are consistent with other studies in industrialized countries.21-23 However, some studies in settings with well developed heath care systems have reported such a protective effect.24-26 The relationship between type of infant feeding and the incidence of infections has been evaluated mainly in analytical studies. In this type of design it is not always easy to avoid systematic errors that compromise or even invalidate the results. Variations in the study design might help explain the inconsistencies between the results of research in countries with a well developed model of health care. However, one recent study that might help to clarify the situation is a multicenter, randomized clinical trial involving 17 046 mothers and their infants in 31 maternity hospitals in Belarus, where the national health system ensures universal coverage available to all inhabitants, as in other European countries. The aim was to evaluate the effectiveness of a program to promote BF (study intervention) on the duration of this type of feeding and on infectious processes, including respiratory tract infections, during the first year of life. The control group consisted of mothers who also used BF but did not participate in the promotional program. The program was effective in increasing the intensity and duration of BF and in decreasing the incidence of episodes of acute gastroenteritis and atopic eczema among infants in the intervention group. However, no decrease was seen in the incidence of respiratory tract infections in these babies.27
In the present study every attempt was made to reduce the presence of bias in order to ensure internal validity. Reverse causality bias was controlled for in the statistical analysis by linking the independent variable (type of feeding) with the incidence of respiratory infections during the subsequent period. This strategy has been used by other authors in recent studies that investigated working hypotheses similar to the one we tested.17,23 Moreover, the persons who recorded type of feeding and potential confounding variables (independent variables) were unaware of the value of the dependent variables (number of episodes of LRTI and URTI), and vice versa: those who recorded the LRTI and URTI data were blind as to the independent variables. This diminished the possibility of bias due to prior knowledge of exposure or response.18
The historical cohort design was chosen for this study. This type of study is used when both exposure and the disease have already occurred. To be useful, the data for the factor of interest and the dependent variables must be recorded carefully and completely.28 This type of design was considered most appropriate for the present study for several reasons. Firstly, in our center good records are kept for pediatrics activities, both preventive (HBP sheets) and care-related (clinical course sheets, emergency visit reports). Furthermore, after each emergency visit the patient is given a personal report in which the diagnosis is indicated. This report is given to the primary care physician at the next visit during regular hours, so that it can be added to the center´s medical record. The medical record also contains the reports given to the patient at the reference hospital emergency service, if the patient was seen there first. Our center holds medical records for more than 95% of the children who live within the basic health area it serves (according to the latest municipal census). This makes it possible to obtain detailed medical information on our users.
One of the limitations in the present study is the possible underrecording of the dependent variables. Some parents might have visited a private practitioner on some occasions, and in some cases the reports from the reference hospital emergency room might not have reached the primary care physician. The possible effects of these factors were minimized by using strict inclusion criteria for the participants. These criteria were aimed at selecting a sample of parents likely to comply with the recommendations of the HBP (ie, parents who preferred to bring their child to our health center). These efforts notwithstanding, it is likely that some episodes of respiratory infection went unrecorded. This situation may have contributed to the weak association between type of feeding and the incidence of respiratory infections. Another possible limitation is type II error, ie, the existence of a statistically significant difference in the reference population that went undetected in the sample we selected because of small sample size for some of the comparisons.18
This is the first study in our setting to evaluate the effect of type of infant feeding on the incidence of respiratory infections while trying to control for possible confounding factors that might influence the relationship. Although the cumulative incidence of LRTI was slightly higher in all periods in babies who received AF, the difference never reached statistical significance and cannot be considered clinically relevant. The most likely explanation for this negative result is that in a setting such as ours, where the economic and health care environment is highly developed, BF has no protective influence on the incidence of respiratory infections, although such an influence has clearly been demonstrated in developing countries.1-8
A secondary objective of this study was to analyze the influence of other variables on the incidence of respiratory tract infections. A number of factors that increased the incidence of LRTI were identified, ie, number of persons in the household, personal antecedents of atopic disorder in either or both parents, and day care use. Several earlier studies have noted these associations,29-31 and other authors have emphasized the clear association between day care use and an increase in the cumulative incidence of LRTI.29-31 Interventions aimed at modifying this factor are possible to try to reduce the number of respiratory processes; for example, appropriate training of day care staff helps to decrease the incidence of respiratory infections in children younger than 2 years.32 The strong association with familial antecedents of atopy is interesting and should be communicated to the parents, as in these families day care services may represent an additional increase in the risk of respiratory infections.
To conclude, this study of BF did not show any significant or clinically relevant decrease in the cumulative incidence of LRTI or URTI. Our findings agree with those of Kramer et al,27 whose data can be considered the most solid currently available, as the study design they used--a randomized clinical trial--is the most powerful method for documenting possible causal relationships.18 These results support the hypothesis that BF in settings where health services are highly developed is of secondary importance as a protective factor, in comparison to other variables such as the number of persons in the household, antecedents of atopy in one or both parents, and day care use. Further prospective cohort studies that take all potential confounders into account will be needed in our setting to evaluate the possible protective efficacy of BF. Moreover, these future studies should be designed with adequate statistical power to confirm or rule out the theoretical protective effect of breastfeeding alone or in combination with formula feeding, in order to verify or refute the results of earlier studies.17
Correspondence: José Cristóbal Buñuel Álvarez. Ronda Fort Riog, 13-14, esc. B, 4.º, 4.º. 17007 Girona. España. E-mail:cbunuel@comg.es jcristobal@wanadoo.es The research project this report is based on was awarded the 1999 Special Prize Scholarship from the Official College of Physicians of Girona. Manuscript accepted for publication: 3 October 2001.