To analyse the biomechanical behaviour of the different femoral fixation systems employed in the reconstruction of the anterior cruciate ligament (ACL) using a static load.
Material and methodACL reconstruction of 33 pig femurs. A high resistance finish was used for the graft, with the aim of eliminating variability and premature fractures. Nine devices were analysed: Biosteon, Biocryl and Softsilk (compression); Biosteon Cross-Pin and Cross-Pin ACL (cortical-spongy suspension); Endobutton and XO Button (cortical suspension); staple (cortical compression); Rigidfix (transverse fixation). Static resistance failure tests were performed, calculating the linear rigidity, failure load, and elongation of that load. The bone was sectioned to observe the failure mode.
ResultsThe staple showed a higher load failure (1.173.7 ± 220.0N), but with a greater elongation (58.8 ± 13.2mm). Of the rest of the fixations, the most resistant were Cross-Pin ACL (1.054.6 ± 150.8N) and Endobutton (1.018.6 ± 230.1N), with the former having greater rigidity (43.5 ± 7.1N/mm).
DiscussionCortical suspension fixations seem to be very affected by the geometry of the bone in the cortical support surface, while those of the cortical-spongy suspension produced a better load distribution. Compression and transverse fixations changed their mechanical properties due to using a synthetic graft.
ConclusionsTaking into account the behaviour shown by the model studied, cortical-spongy suspension fixation was shown to be the best option, on having a balanced load distribution on the bone and not very aggressive.
Analizar el comportamiento biomecánico de diferentes sistemas de fijación femoral empleados en la reconstrucción del ligamento cruzado anterior (LCA) ante una sobrecarga estática.
Material y métodoReconstrucción LCA en 33 fémures porcinos. Como injerto se utilizó un cabo de alta resistencia, a fin de eliminar la variabilidad y las roturas prematuras. Fueron analizados 9 dispositivos: Biosteon, Biocryl y Softsilk (compresión); Biosteon Cross-Pin y Cross-Pin ACL (suspensión cortico-esponjosa); Endobutton y XO Button (suspensión cortical); grapa (compresión cortical); Rigidfix (transfixión). Se realizaron ensayos estáticos de resistencia al fallo, calculando la rigidez lineal, la carga de fallo y la elongación en dicha carga. Se seccionó el hueso para observar el modo de fallo.
ResultadosLa grapa mostró una carga de fallo mayor (1.173,7 ± 220,0N), pero con una gran elongación (58,8 ± 13,2mm). Del resto de fijaciones, las más resistentes fueron Cross-Pin ACL (1.054,6 ± 150,8N) y Endobutton (1.018,6 ± 230,1N), presentando la primera una mayor rigidez (43,5 ± 7,1N/mm).
DiscusiónLas fijaciones de suspensión cortical parecen muy influenciadas por la geometría del hueso en la superficie cortical de apoyo, mientras que las de suspensión cortico-esponjosa producen un mejor reparto de carga. Las fijaciones de compresión y de transfixión ven modificadas sus propiedades mecánicas por la utilización del injerto sintético.
ConclusionesAtendiendo al comportamiento exhibido del modelo estudiado, las fijaciones de suspensión cortico-esponjosa se muestran como una opción muy buena, al realizar un reparto de cargas sobre el hueso equilibrado y poco agresivo.
In the first few weeks after anterior cruciate ligament (ACL) reconstruction, and until biological integration is produced, the mechanical behaviour of the implanted fixation system is decisive, as it is the weakest element, with a resistance that is lower than that of the graft.1 During the last few years, different devices have come to the market and this has caused great controversy when having to decide which is the best.1–4
From the mechanical point of view, good ACL fixation should comply with resistance and rigidity requisites, so that there is no plasty failure before biological fixation is produced. Both parameters determine the stability of the knee. From the medical point of view, characteristics such as absorption capacity by the body, a not very aggressive surgical technique or the ease of extraction, if there are later complications, are also assessed.
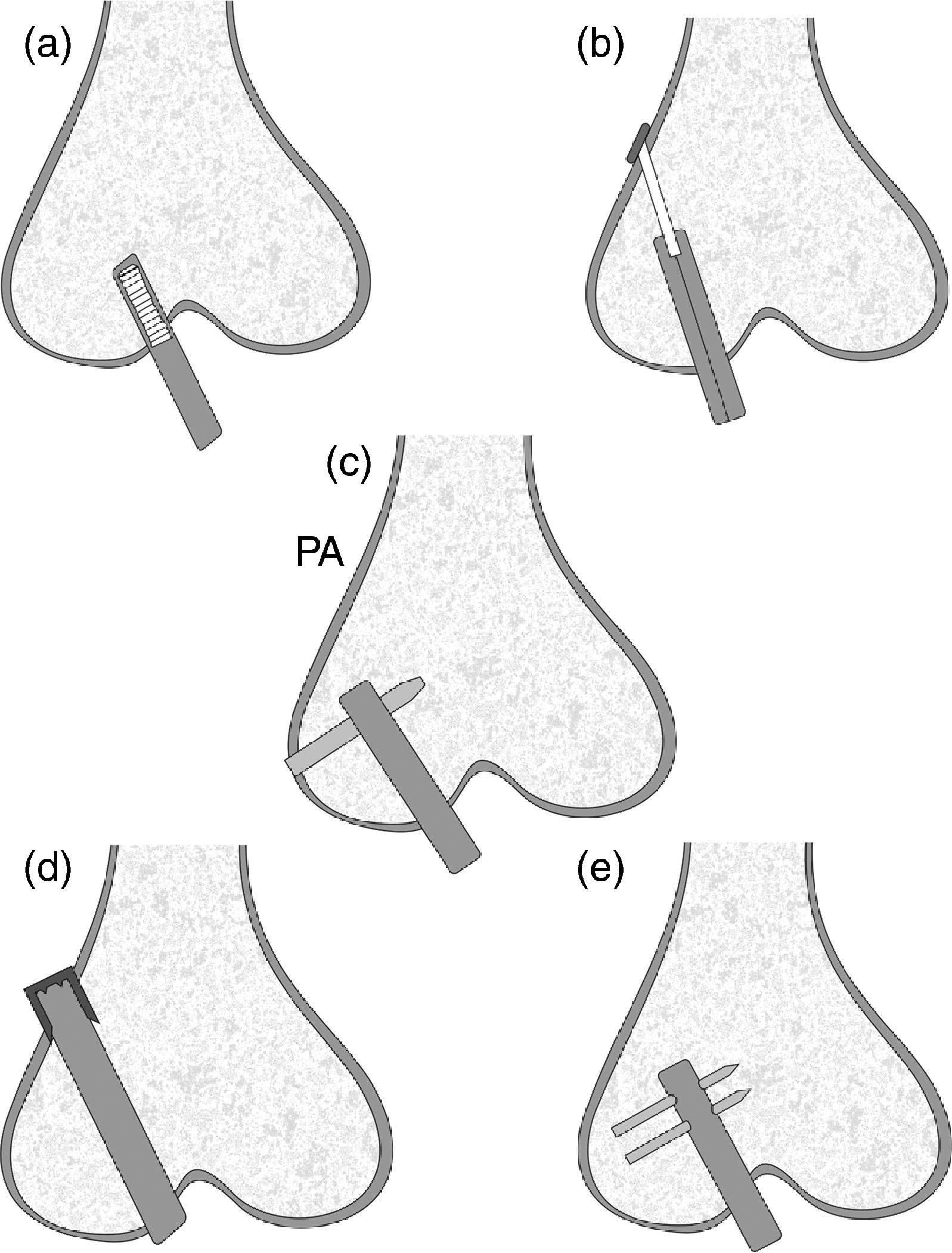
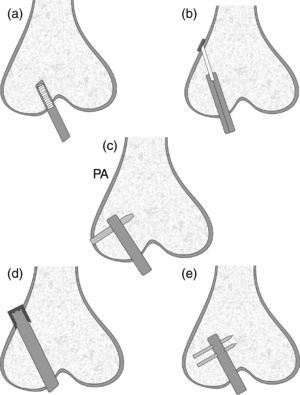
Anterior cruciate ligament femoral graft fixation systems can be classified according to where the loads are applied and their distribution. There are three types: fixation via compression, via expansion or transverse fixation and via suspension. This last group is in turn subdivided into another three sub-groups, according to where the suspension occurs: cortical suspension (the cortical bone bears the load), cancellous suspension (the load is borne by the cancellous bone) and cortical-cancellous suspension (the loads are shared by both areas). In Fig. 1, we can see a diagram with the mode of operation of the different fixation types.
Many biomechanical studies, such as those of Milano et al.3 and Brown et al,4 have compared the behaviour of different femoral types of fixation using biological material. These studies produced mainly two problems: highly disperse results and premature graft breakage in many cases. So as to eliminate or decrease this variability, which could lead to the failure of the whole femur-fixation, we have carried out biomechanical static traction trials until failure, by substituting the biological origin graft with a high resistance braided cord, in such a way that fixation behaviour was observed until the moment of failure. These trials represented the effect of an instant overload after the intervention.
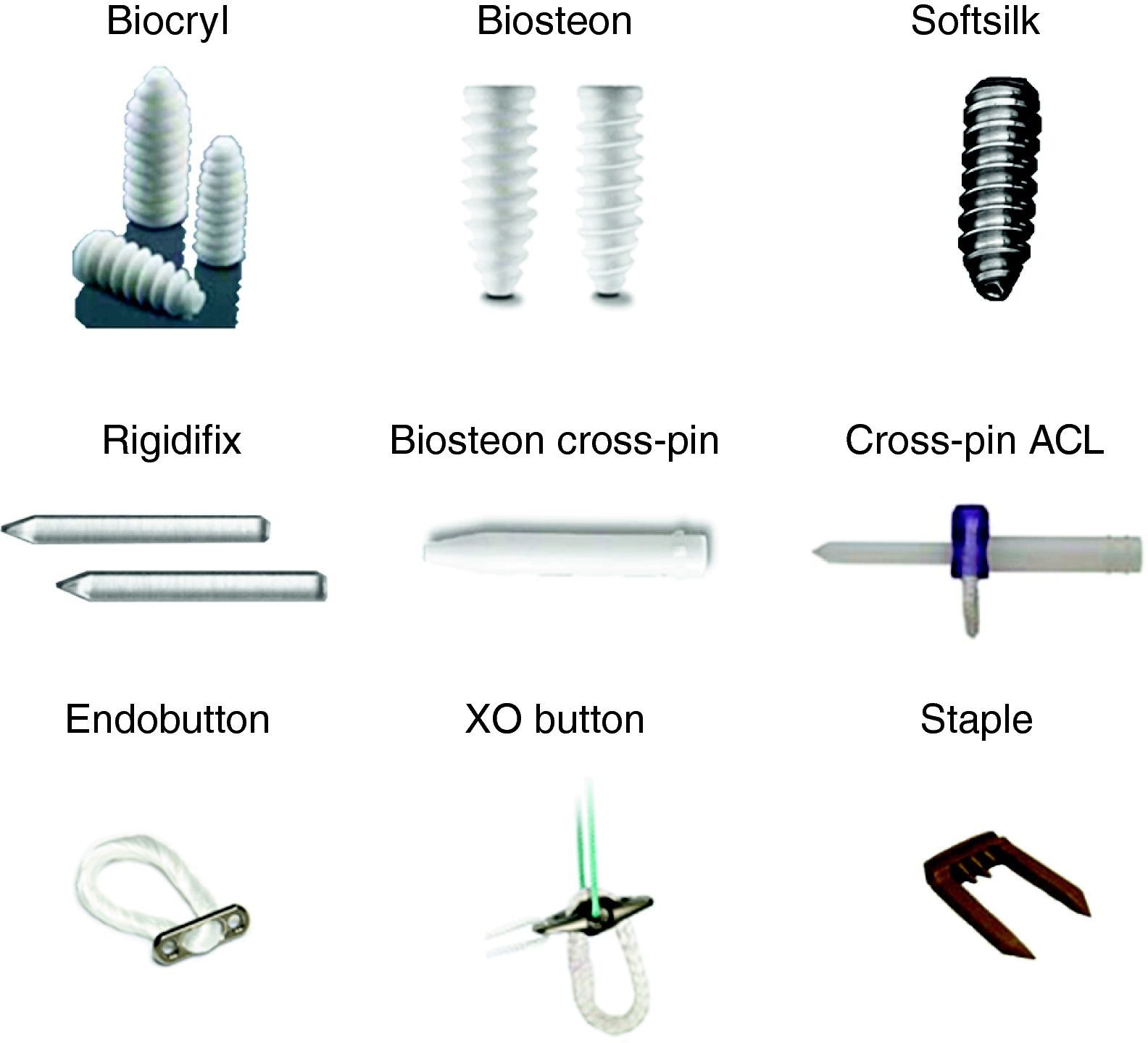
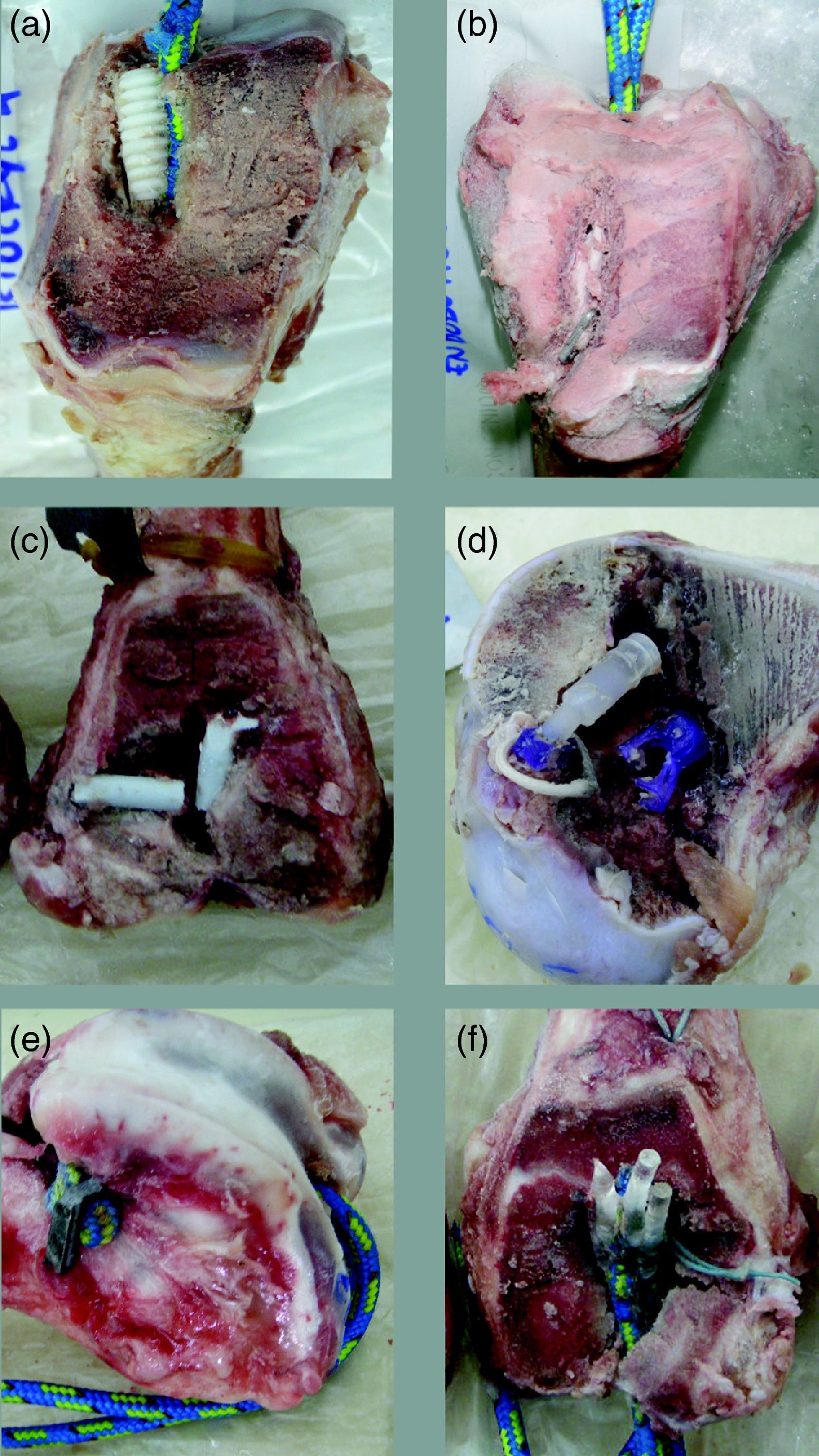
Material and methodWe used 33 distal limbs from adult pigs for this study, all with similar morphology, collected just when the pigs were slaughtered. The surrounding soft tissues were cleaned and the limbs were kept at −20°C; they remained at room temperature for 12h before being used in the trial. A braided cord was used as an artificial graft (DYNEMIC 2002, Polyropes Yachting, Sweden) with high mechanical resistance (7400N for a diameter of 4mm). The cord was folded over itself, so that an artificial 8mm diameter graft was obtained. Nine different fixation systems were analysed. Three systems were compression fixations: Biocryl (Mitek, Norwood, MA, USA) with an 8mm diameter and 23mm length, Biosteon (Stryker, San Jose, CA, USA) with an 8mm diameter and 24mm length and Softsilk (Smith & Nephew, Andover, MA, USA) with an 8mm diameter and 25mm length. There were two cortical suspension devices: Endobutton-CL (Smith & Nephew) and XO Button (Linvatec, Largo, FL, USA), both with a cross-pin of 30mm; there were also two cortical-cancellous suspension systems: the Biosteon Cross-Pin (Stryker), 6mm in diameter and 40mm long, and the Cross-Pin ACL (Linvatec), 50mm long (25mm cortical length) and 8mm in diameter harness. Finally, there was one staple cortical compression system (Surgival, Valencia, Spain), 25mm long by 10mm wide and 3mm thickness, plus one transverse-fixation system (Rigidfix, Mitek), made up of two pins 3.3mm in diameter and 34mm long. In Fig. 2, we can see the different fixation systems analysed.
The implantation method for the fixation systems was the same in all cases. A femoral perforation was performed and the fixation implant was placed according to a standard technique for each of them, using specific instruments and following the technical guidelines of each company strictly. The tunnel was completed after the ACL insertion area had been located on the inside of the lateral femoral condyle in a high anteromedial (AM) disposition. A 2.4mm diameter needle-guide was used together with a specific guide to introduce this needle, with an offset that allowed a constant distance of 6mm from the posterior cortical area. The tunnel was always perforated according to the “inside-out” technique used in all fixation techniques, always scrupulously maintaining the initial tunnelling for cortical suspension systems of 4.5mm, as well as constant diameter for the 8-mm tunnel. Once the tunnel was made, the synthetic graft was introduced according to the technique used in clinic, via traction from the outside of the femur.
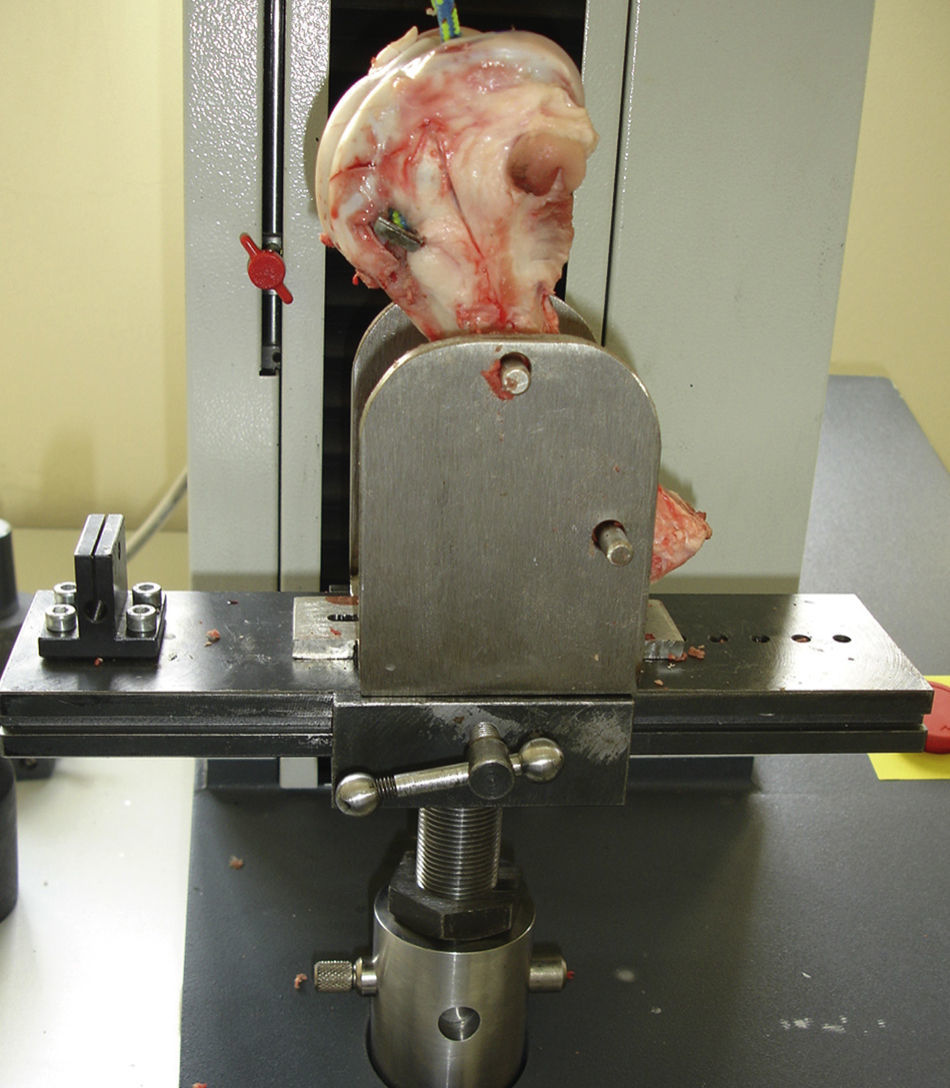
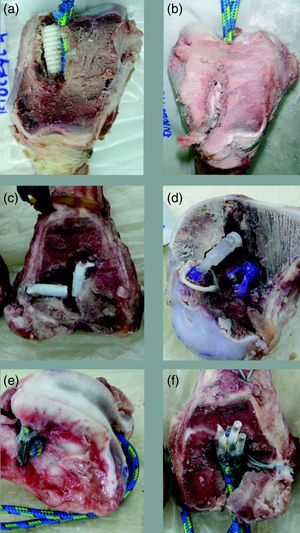
Biomechanical trialsWe carried out at least three biomechanical traction trials to failure for each of the different ALC fixation types previously described. The trials were undertaken using a universal mechanical testing machine (INSTRON, Canton, MA, USA) with a 5kN load cell. The distal femur was fixed to the trial machine using a specially designed device for this job that allowed, via two steel pins that went through the femur, its correct positioning, in such a way that the direction of the load application was parallel to the femoral tunnel in all cases (Fig. 3). The synthetic cord used as a graft was fixed on the upper side of the trial machine using a 10mm diameter steel pin. The length of the cord between the intraarticular tunnel exit and the holding pin was 100mm.
All specimens were preloaded at 10N for 5min before the start of the trial. The application speed of the load was 5mm/min. A load-displacement recording was taken, to enable later calculation of linear rigidity K (N/mm), calculated as the slope of the linear area of the load-displacement curve, the failure load Pu (N) and the elongation corresponding to this load du (mm). To correct the elongation effect of the artificial graft, we conducted a no load trial, which consisted of a traction at a displacement speed of 5mm/min up to 2000N (a load that is higher than the maximum expected for fixations), recording the load-displacement curve.
Once the trial ended, the bone was sectioned with an electric saw, leaving the tunnel and fixation uncovered to be able to see the reason for failure, which was classified as fixation breakage, bone fracture, graft exit or implant migration.
Statistical analysisThe results were statistically analysed using a comparison between the different fixations and between other different types of fixation (compression, cortical suspension, cortical-cancellous suspension, cortical compression and double transverse fixation.) A variance analysis was carried out on each of the corresponding factors so as to be able to compare failure, elongation and rigidity. In cases where significant differences were found, the study was complemented with a Duncan test, as a post-hoc comparative method, for all pairs of possible comparisons. Given that effects on three different variables (load failure, elongation and rigidity) were involved, all the analyses were carried out in triplicate. The significance level used in all of them was the usual one of 5% (significant if P<.05). The analyses were carried out using the statistical package PASW Statistics 18 (IBM, Somers, NY, USA).
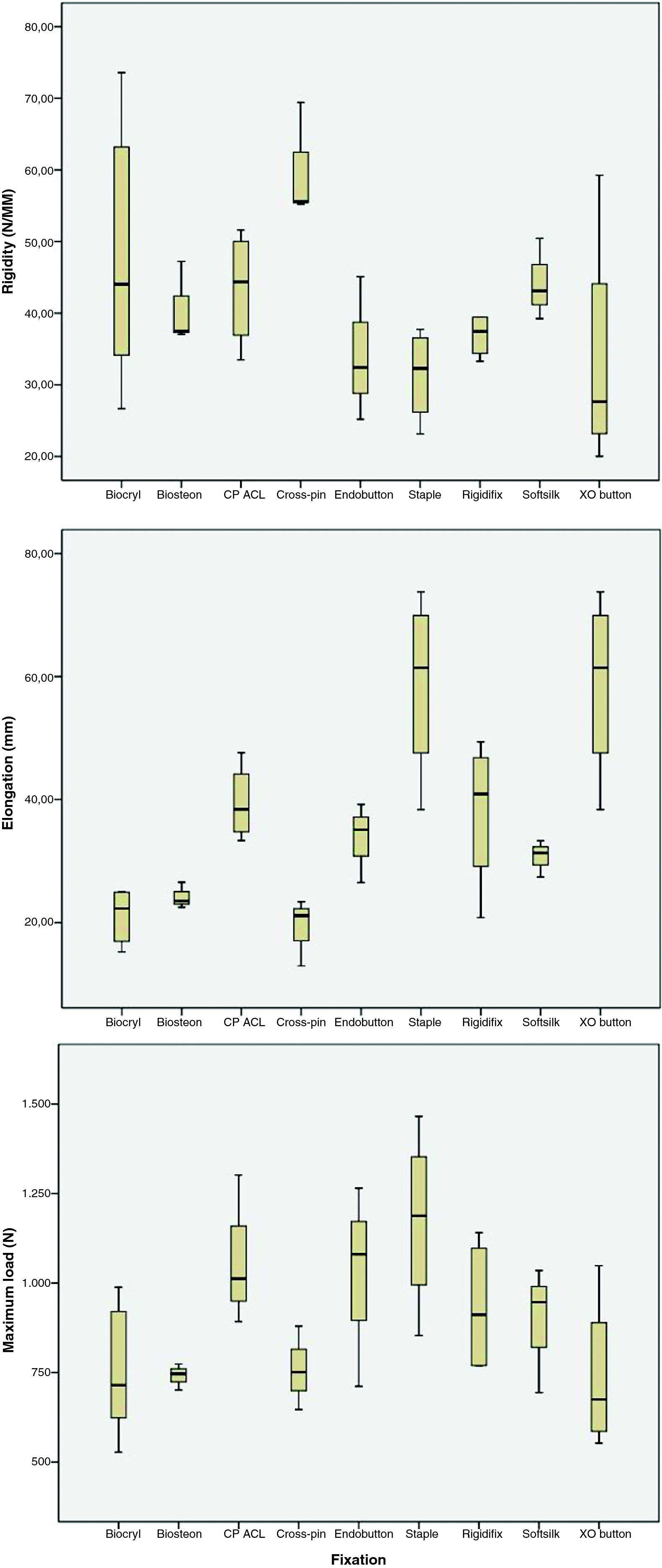
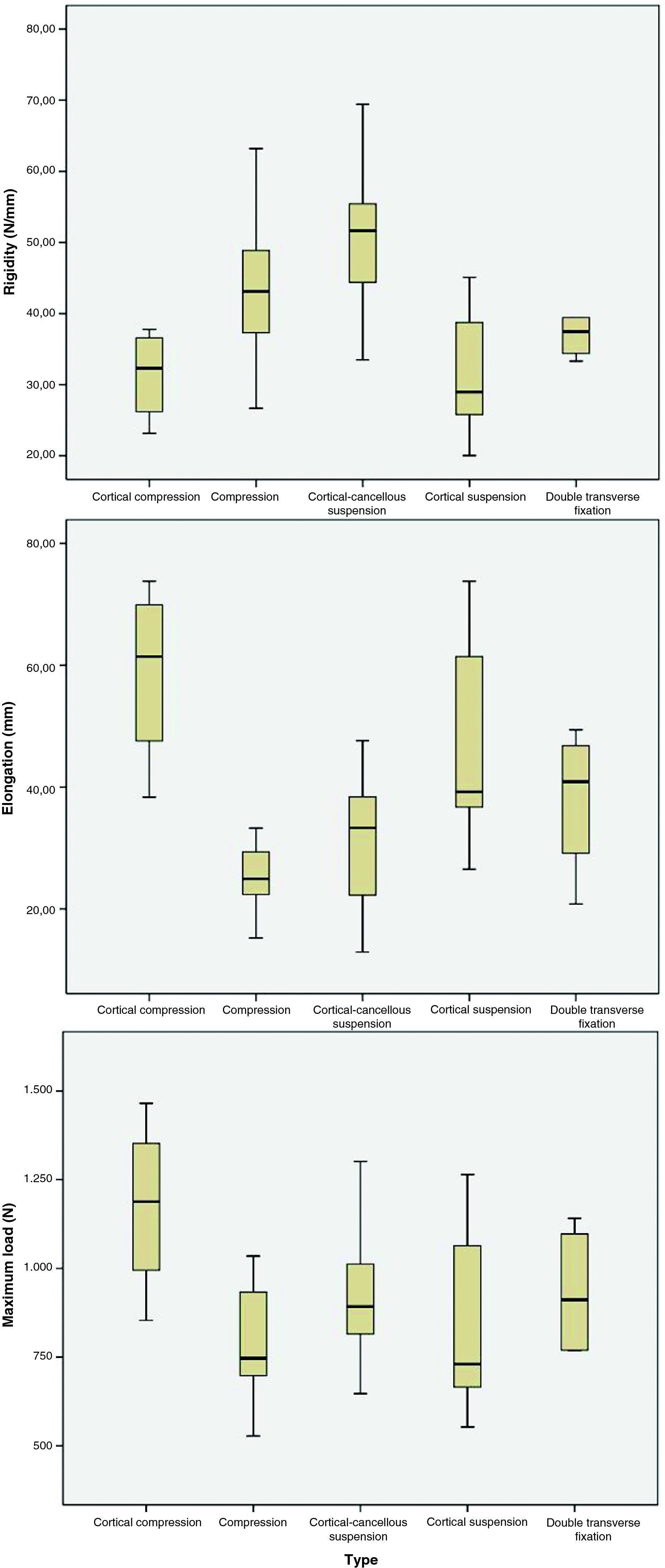
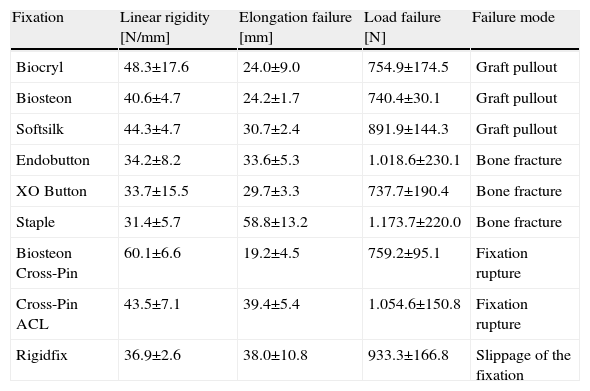
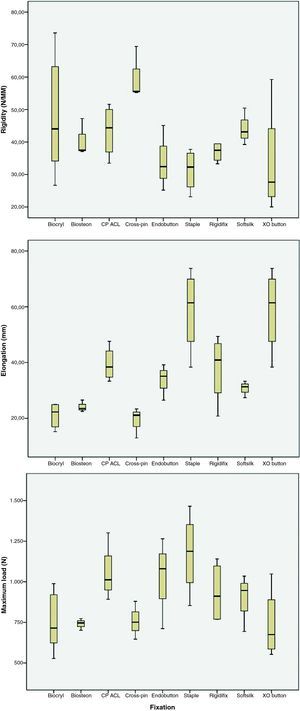
ResultsTable 1 shows the mean values and the standard deviations obtained after analysing the results corresponding to the 9 fixation systems studied, as well as the representative failure modes. Fig. 4 shows a box plot comparing rigidity, elongation and load failure for each fixation.
Mean and standard deviation of the results obtained in the resistance failure tests after intervention.
| Fixation | Linear rigidity [N/mm] | Elongation failure [mm] | Load failure [N] | Failure mode |
| Biocryl | 48.3±17.6 | 24.0±9.0 | 754.9±174.5 | Graft pullout |
| Biosteon | 40.6±4.7 | 24.2±1.7 | 740.4±30.1 | Graft pullout |
| Softsilk | 44.3±4.7 | 30.7±2.4 | 891.9±144.3 | Graft pullout |
| Endobutton | 34.2±8.2 | 33.6±5.3 | 1.018.6±230.1 | Bone fracture |
| XO Button | 33.7±15.5 | 29.7±3.3 | 737.7±190.4 | Bone fracture |
| Staple | 31.4±5.7 | 58.8±13.2 | 1.173.7±220.0 | Bone fracture |
| Biosteon Cross-Pin | 60.1±6.6 | 19.2±4.5 | 759.2±95.1 | Fixation rupture |
| Cross-Pin ACL | 43.5±7.1 | 39.4±5.4 | 1.054.6±150.8 | Fixation rupture |
| Rigidfix | 36.9±2.6 | 38.0±10.8 | 933.3±166.8 | Slippage of the fixation |
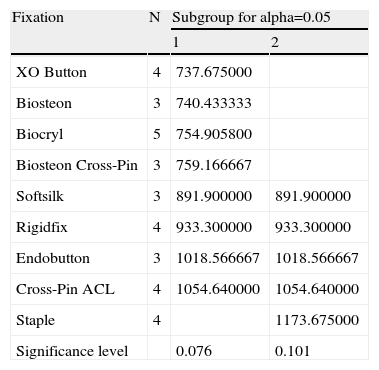
The post hoc analysis (Table 2) showed significantly higher resistance for the staple type fixation, with a value of 1.173.7±220.0N. The ANOVA had a P-value of 0.039. In the rest of the fixations, we can confirm that there were no significant differences for load failure. Those that showed greater resistance were the Cross-Pin ACL (1.054.6±150.8N), Endobutton (1.018.6±230.1N) and Rigidfix (933.3±166.8N).
Duncan test: load failure (N).
| Fixation | N | Subgroup for alpha=0.05 | |
| 1 | 2 | ||
| XO Button | 4 | 737.675000 | |
| Biosteon | 3 | 740.433333 | |
| Biocryl | 5 | 754.905800 | |
| Biosteon Cross-Pin | 3 | 759.166667 | |
| Softsilk | 3 | 891.900000 | 891.900000 |
| Rigidfix | 4 | 933.300000 | 933.300000 |
| Endobutton | 3 | 1018.566667 | 1018.566667 |
| Cross-Pin ACL | 4 | 1054.640000 | 1054.640000 |
| Staple | 4 | 1173.675000 | |
| Significance level | 0.076 | 0.101 | |
Among the most resistant fixations, only the Cross-Pin ACL also presented a good rigidity value (43.5±7.1N/mm), as the other three types (staple, Endobutton and Rigidfix) presented the lowest values. The fixation with the greatest rigidity was the Biosteon Cross-pin (60.1±6.6N/mm), followed by the three interference screws and the Cross-Pin ACL, all showing very similar values of around 45N/mm.
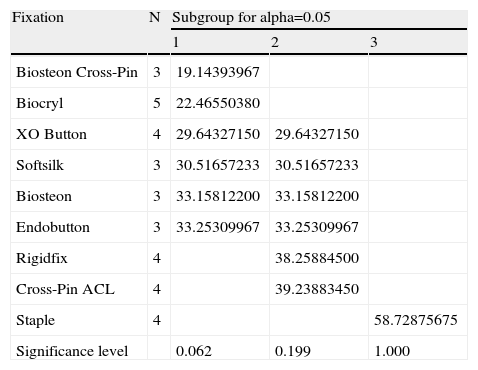
With reference to elongation, the post hoc analysis (Table 3) shows a significantly higher value for the staple (58.8±13.2mm), with there being no significant differences for the rest of the fixations. The least elongation was obtained with Biosteon Cross-Pin (19.2±4.5mm).
Duncan test: elongation (mm).
| Fixation | N | Subgroup for alpha=0.05 | ||
| 1 | 2 | 3 | ||
| Biosteon Cross-Pin | 3 | 19.14393967 | ||
| Biocryl | 5 | 22.46550380 | ||
| XO Button | 4 | 29.64327150 | 29.64327150 | |
| Softsilk | 3 | 30.51657233 | 30.51657233 | |
| Biosteon | 3 | 33.15812200 | 33.15812200 | |
| Endobutton | 3 | 33.25309967 | 33.25309967 | |
| Rigidfix | 4 | 38.25884500 | ||
| Cross-Pin ACL | 4 | 39.23883450 | ||
| Staple | 4 | 58.72875675 | ||
| Significance level | 0.062 | 0.199 | 1.000 | |
The failure mode depended on the type of fixation. In the interference fixations, the failure was due to the graft sliding between the tunnel and the screw. In the case of the Endobutton, XO Button and staple, the failure came about due to a cortical bone fracture when the fixations became embedded in it. With the Biosteon Cross-Pin and Cross-Pin ACL devices, the failure was due to the devices themselves. In the case of the Rigidfix, two types of failure were obsered: in two of the implants studied (those which bore the least maximum load), one pin failed first and then the other one failed immediately afterewards; in the other two cases, the two pins suffered a great deformity on flexion and were dragged by the graft in their migration through the femoral tunnel. Fig. 5 shows the most representative failure modes for each fixation.
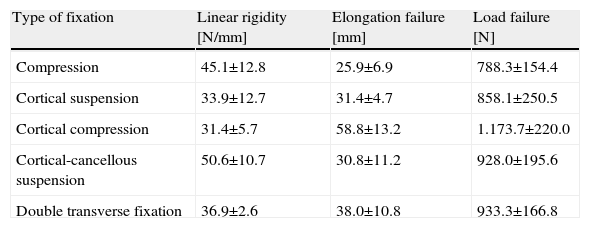
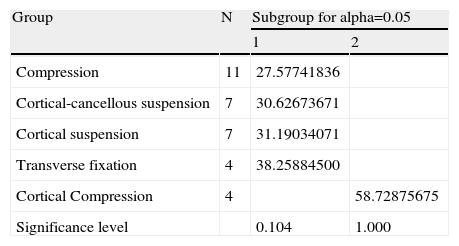
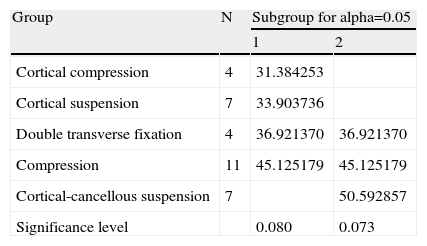
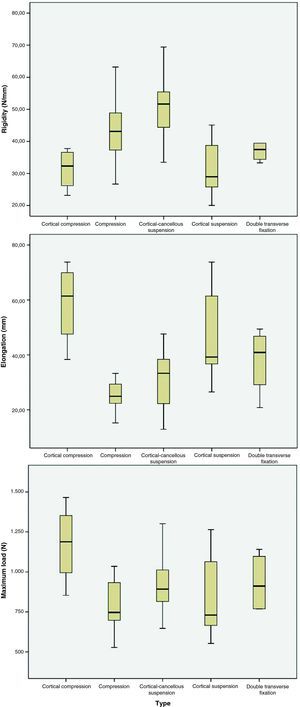
Table 4 shows the mean values and standard deviations obtained by grouping the fixations by mode of operation (type of fixation), while Fig. 6 shows box plots of rigidity, elongation and load failure grouping the fixations according to their classification. In this case, the post hoc analysis showed a significantly longer elongation for the fixation with cortical compression (staple), while it showed greater rigidity in the cortical-cancellous suspension fixations. There was no evidence of significant differences with respect to the failure load. Tables 5 and 6 show the results obtained in the post hoc analysis for elongation and rigidity, respectively.
Mean values and standard deviations for fixations grouped into types of fixation.
| Type of fixation | Linear rigidity [N/mm] | Elongation failure [mm] | Load failure [N] |
| Compression | 45.1±12.8 | 25.9±6.9 | 788.3±154.4 |
| Cortical suspension | 33.9±12.7 | 31.4±4.7 | 858.1±250.5 |
| Cortical compression | 31.4±5.7 | 58.8±13.2 | 1.173.7±220.0 |
| Cortical-cancellous suspension | 50.6±10.7 | 30.8±11.2 | 928.0±195.6 |
| Double transverse fixation | 36.9±2.6 | 38.0±10.8 | 933.3±166.8 |
Duncan test: elongation (N/mm) of the different types of fixation.
| Group | N | Subgroup for alpha=0.05 | |
| 1 | 2 | ||
| Compression | 11 | 27.57741836 | |
| Cortical-cancellous suspension | 7 | 30.62673671 | |
| Cortical suspension | 7 | 31.19034071 | |
| Transverse fixation | 4 | 38.25884500 | |
| Cortical Compression | 4 | 58.72875675 | |
| Significance level | 0.104 | 1.000 | |
Duncan test: rigidity (N/mm) of the different types of fixation.
| Group | N | Subgroup for alpha=0.05 | |
| 1 | 2 | ||
| Cortical compression | 4 | 31.384253 | |
| Cortical suspension | 7 | 33.903736 | |
| Double transverse fixation | 4 | 36.921370 | 36.921370 |
| Compression | 11 | 45.125179 | 45.125179 |
| Cortical-cancellous suspension | 7 | 50.592857 | |
| Significance level | 0.080 | 0.073 | |
The way that the different fixations work allows us to classify them, as well as to explain the results obtained.
The Biocryl, Biosteon and Softsilk interference screws belong to the group called compression fixation, which operates using the radial compression force the screw has on the graft. The first two (manufactured with biocancellous materials) reach 740N resistance and, in the case of Biocryl, 48N/mm of rigidity, while the third (which is metal) reaches 890N and 44N/mm rigidity. These are values that are very similar to those obtained in previous biomechanical studies.5–10 The greater resistance shown by the Softsilk metal screw could be based on its longer length (25mm) compared to those of the biocancellous ones (23 and 24mm), with the same diameter. The greater the screw length used, the greater the force of friction, between the tunnel and the graft, which opposes its extraction. This would corroborate the conclusions set out by Selby et al.11 who studied the effect of length on the failure load of interference screws. In addition to this, the reconstruction quality undertaken with this type of fixation would depend on different parameters, such as the shape and size of the screw threads, the material they are made from, bone mineral density, etc. The great variability of our results, as well as those collected in referenced literature, is determined by the factors previously described, as well as other trial parameters such as the grafts used or the speed at which the load was applied, as seen in the study carried out by Martel et al.5
The fixation mechanism of cortical suspension devices, such as Endobutton and XO Button, basically consists of suspending the graft from a loop that in turn hangs from a metal plate supported on the anterior-lateral area of the distal cortex of the femur. The results obtained for the Endobutton agree, with regards to maximum load (1.018.6N), with those presented by other researchers6,12 who analysed the behaviour of this mechanism. However, the XO Butto, showed less resistance and rigidity (737.7N and 33.7N/mm, respectively). The difference regarding maximum load between the two systems could be based on the different geometry of the anchor plate. The greater support surface area of the Endobutton plate would promote a better spread of the load on the cortical surface of the bone and, consequently, a much later fracture. The low rigidity and high elongations shown by both devices could be based on two factors: on the one hand, the use of loops which are longer than those usually used in clinics, and, on the other hand, the low speed of the load used.5 The failure mechanism of these fixations was the same in all cases: it was produced by a rupture in the cortical bone surface in the area that made contact with the plate; immediately thereafter, the plate turned and faced in the direction of the tunnel sliding across it with hardly any opposition.
The cortical-cancellous suspension devices, such as the Biosteon Cross-Pin and Cross-Pin ACL, transfer the load that comes from the graft to the cortical-cancellous bone through a bar (pin) that is placed transversally to the tunnel and whose ends are supported on these areas of bone. The mechanical behaviour of these fixations is highly influenced not only by pin resistance,13,14 but also by bone quality12 and, above all, by the correct allocation of the load to be supported (the more centred the section by which the graft “hangs” from the pin is, the better). This last point fully justifies the difference regarding the resistance between the Cross-Pin ACL (1.054N) and Biosteon Cross-Pin (759.2N). In the first one, the use of the intermediate harness, positioned in the central section of the pin, ensures a correct load distribution; in the second device, this centering is not completely ensured. The use of an intermediary device (a harness with a loop from which the graft hangs) in the Cross-Pin ACL would also explain why this device shows less rigidity than its homologue (43.5 compared to 60.1N/mm). These design differences also explain the different failure modes: while the Biosteon Cross-Pin failed in all cases through pin rupture, the failure in the Cross-Pin ACL was produced by a break in the transmission harness.
The cortical compression system (staple) consists of literal stapling of the new ligament, passing it through the tunnel to the upper femur head, producing a hold based on the pressure exerted by the staple on the graft and bone. This fixation presented the best value of resistance to failure (1.173.7±220N), but at a cost of great elongation, low rigidity and complete destruction of the cortical bone surface in contact with the staple, which was the failure mode seen. In a previous study by Gerich et al.10 there was a mean load failure of 588N and a rigidity of 86.3N/mm. The greatest resistance obtained in this study is surely based on the greater coefficient of the synthetic graft friction compared to that of the biological one.
Lastly, the Rigidfix system belongs to the group of the so-called expansion or transverse fixation systems. These devices consist of one of more pins placed transversally to the femoral tunnel, crossing the graft and causing it to bulge, which consequently forms a radial pressure against the tunnel walls in this area. Previous biomechanical studies6,15 obtained load failures between 639 and 868N and rigidities between 77 and 226N/mm. In our case, the mean failure rate was slightly higher (933.3N), which would again be based on the use of a synthetic graft, which has a greater resistance to tear than real grafts. The lower testing speed used in our study justifies the lesser rigidity values obtained.5 The biomechanical behaviour of the Rigidfix device depends on variables such as initial pressure of the graft adjustment or bone density and on correct pin positioning above all. In fact, offset pin placement on the inside of the tunnel would produce a non-homogeneous distribution of the load in the bone–graft interface that would notably reduce the resistance to the group. In two of the cases tested, where the pins correctly crossed the graft and worked together, loads of 1.100N were reached; however, in another two cases, where the pin placement was incorrect, the reached loads did not go over 770N.
We should point out that, although this study attempted to reproduce the mechanical behaviour of the ALC femoral fixation systems, using surgical techniques as well as normal fixation systems, this was still a laboratory trial where the lack of human femurs was compensated by using samples from pigs and that of biological plasty by using synthetic grafts. Although the use of a pig femur is fully supported and justified by other similar studies,2,5–8,15 the use of an artificial graft could have influenced the response of some of the fixation types, such as interference screws, transverse fixation and staples.
These static load trials have allowed us to analyse and compare the failure modes in the different fixations, although this obviously does not reproduce the complete rehabilitation process.
ConclusionsFirstly, faced with a possible overload immediately after reconstruction, all the fixations analysed show a failure rate higher than what they should usually bear after an operation, which varies2,12 from between 35 to 450N.
Considering the biomechanical behaviour exhibited with an overload, the cortical-cancellous suspension fixations are profiled as a good alternative. They combine high levels of resistance and greater rigidity, as well as sharing the load in a balanced way on the bone, avoiding concentrations of aggressive tension.
The mechanical behaviour of the cortical suspension systems depends to a great extent on the contact surface area between the plate and bone.
We cannot obtain relevant conclusions on the remaining fixations, given that the test method used (synthetic graft) seems to influence its mechanical behaviour.
Evidence levelEvidence level IV.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors are grateful to the manufacturers ConMed Linvatec, DePuy Mitek, Smith & Nephew, Stryker Corporation and Surgival for donating their fixation devices and providing the necessary instruments for their implant.
Please cite this article as: Rodríguez C, et al. Comportamiento biomecánico bajo carga estática de diferentes siste-mas de fijación femoral para la reconstrucción del ligamento cruzado anterior. Rev Esp Cir Ortop Traumatol. 2011;55(6):428–436.