This study retrospectively analysed the incidence of dislocation and its risk factors in a multicentre series of total hip replacement with a Trident® ceramic acetabular system.
Material and methodCases of dislocation in a series of 401 total hip replacements performed using a Trident® ceramic acetabular system in 10 Spanish hospitals between the years 1998 and 2004, with a mean follow-up of 5.08 years, were analysed and compared to a control group. The influence of different variables, general, clinical and surgical was evaluated and a computer-assisted analysis was made of the radiographic variables possibly involved in the risk of dislocation.
ResultsThe incidence of dislocation in the whole series was 1.75%, lower than incidence rates in series analysed that used other types of artificial joints. The most important dislocation risk factors found were the abduction angles and acetabular inclination (P=0.016), although there was also tendency to dislocation as the patient age and the ASA level increased.
ConclusionWhen performing a ceramic-ceramic joint total hip replacement, the angle of acetabular abduction appears to be the most important factor to take into account to prevent dislocation. Femur head sizes greater than 32mm could act as a limiting factor of the risk of artificial joint dislocation. Clinical variables, such as the age of the subject or ASA level show a tendency as a risk of artificial joint dislocation.
Objetivos: Este estudio analiza retrospectivamente la incidencia de luxación y sus factores de riesgo en una serie multicéntrica de artroplastias totales de cadera (ATC) con sistema acetabular Trident® de cerámica.
Material y Método: Se analizan frente a un grupo control los casos de luxación encontrados en una serie de 401 ATC llevadas a cabo con el sistema acetabular Trident® de cerámica en 10 hospitales españoles entre los años 1998 y 2004, con un seguimiento medio de 5,08 años. Se evaluó la influencia de diferentes variables, generales, clínicas y quirúrgicas, y se realizó un análisis asistido por ordenador de las variables radiográficas posiblemente implicadas en el riesgo de luxación. Resultados: La incidencia de luxación en el total de la serie fue del 1,75%, por debajo de las tasas de incidencia en series analizadas en las que se usan otro tipo de pares protésicos. Los factores de riesgo de luxación más importantes encontrados han sido los ángulos de abducción e inclinación acetabular (P=0,016), aunque también se ha apreciado una tendencia a la luxación a medida que aumenta la edad del paciente y el grado ASA.
Conclusión: A la hora de realizar una ATC de par cerámica-cerámica el ángulo de abducción acetabular parece ser el factor más importante a tener en cuenta para prevenir la luxación. Tamaños de cabeza femoral mayores de 32mm podrían actuar como factor limitante del riesgo de luxación protésica. Variables clínicas como la edad del sujeto o el grado ASA muestran su tendencia como factores de riesgo de luxación protésica.
Total hip replacement (THR) is the most commonly used joint reconstruction procedure and that best deals with the great majority of conditions that this joint may suffer.1 However, a series of factors concur in this surgical procedure, such as aseptic loosening, dislocations, infections and periprosthetic fractures, which limit its functional results and survival.2
The ceramic–ceramic joint has till now been shown to have the lowest in vivo wear, around 0.025mm/year,3,4 compared to 0.03–0.08mm/year of the ceramic–polyethylene joint5,6 and the 0.08–0.14mm/year of the metal–polyethylene joint.7–9 Unlike metals, ceramics do not react with oxygen-rich environments rich, which is why they have no oxidative wear.10
The ceramic joint has been widely accepted, with series such as Hamadouche et al.,4 Nich et al.11 or Murphy et al.12 and 18.5, 16 and 9 years of follow-up, respectively. The mean survival rate was greater than 85% for the first two series and 96% for the third.
Even if the follow-up analysis of these types of implants is starting to be sufficiently documented, there is still a lack of research work that studies the incidence rate and risk factors for dislocation with ceramic–ceramic acetabular systems.13 This type of implants may present a greater incidence rate of dislocations related to fewer alternatives for inserts and neck lengths that reinstate the normal offset joint. Given the possibility, the team led by Colwell et al. analysed the infection rate of early dislocations in THR with modern ceramic–ceramic joints. Out of 1635 THRs analysed over a period of 9 years (1996–2005), the authors observed 3 anterior dislocations and 15 posterior ones, an overall dislocation rate of 1.1%.14
Dislocation in the latest generation of ceramic-ceramic joints has generally been related to poor implantation technique, with placement that leans too much towards the cupula,15 or to insufficient bone fixation of the implant.16,17
Based on the above, the aim of this study was to retrospectively analyse the incidence, types and risk factors of dislocation in a multi-centred THR series using the ceramic acetabular Trident® system, placing a special emphasis on the influence that the positioning of the acetabular component and the diameter of the artificial femoral head could have on it.
Material and methodA retrospective multi-centre study was carried out in 10 public hospitals in the Spanish National Health System. The study included primary THRs performed using the ceramic acetabular Trident® system (Stryker Corporation, Kalamazoo, MI, USA). A total of 401 THRs from 396 patients were analysed, with a mean follow-up period of 5 years (4–9 years), surgery being carried out during the period 1998–2004.
The mean age of the patients in the series was 51±11 years old, with 8.97% being over 65 years of age. The majority of patients in the series were men (63.1%). The main diagnosis in the majority was primary osteoarthritis (53.5% of the cases), followed by avascular necrosis (26.4%), and to a lesser degree fractures (4.4%), rheumatoid arthritis (4.1%) or hip dysplasia (3.9%). The American Society of Anaesthesiologists (ASA) level was 1 in 48.5% of cases, 2 in 41.3% and 3 in 9.7%; it was 4 only in 0.05%. The surgical approaches used in the operations were posterior (55.0%), anterolateral (23.0%), lateral (21.7%) and anterior (0.03%). The diameter of the femoral head used was 32mm in the majority of patients (66.8%), 28mm in 21.5% and 36mm in 11.7%. According to the Dorr classification,18 65% of the cases in the series presented a type 1 femur, compared to 28.2% of type 2 femur and 6.8% type 3.
Standardisation, digitalisation and computer assisted analysis of the radiographic images.
All patients included in the study had an anterior–posterior X-ray of the pelvis and both hips following American College of Radiology19 recommendations during the preoperative and immediate post-operative periods, at each of the follow-up visits (3, 6, 12 months and annual) and during the artificial joint dislocation episode.
The analogue–digital conversion of the X-rays was carried out using a Vidar DiagnosticPro Advantage (Vidar Systems Corporation, Herndon, VA, USA) high-resolution image digitiser. The different coxometric measurements and the radiographic variable analysis were carried out using the computer system Trabeculae® SACRA-ATC® (Trabeculae® Empresa de Base Tecnológica, S.L. Ourense, Spain).
GroupsWe selected a non-dislocated THR for each case of dislocated hip replacement through a random number table to determine the risk factors of dislocation and to obtain a control group.
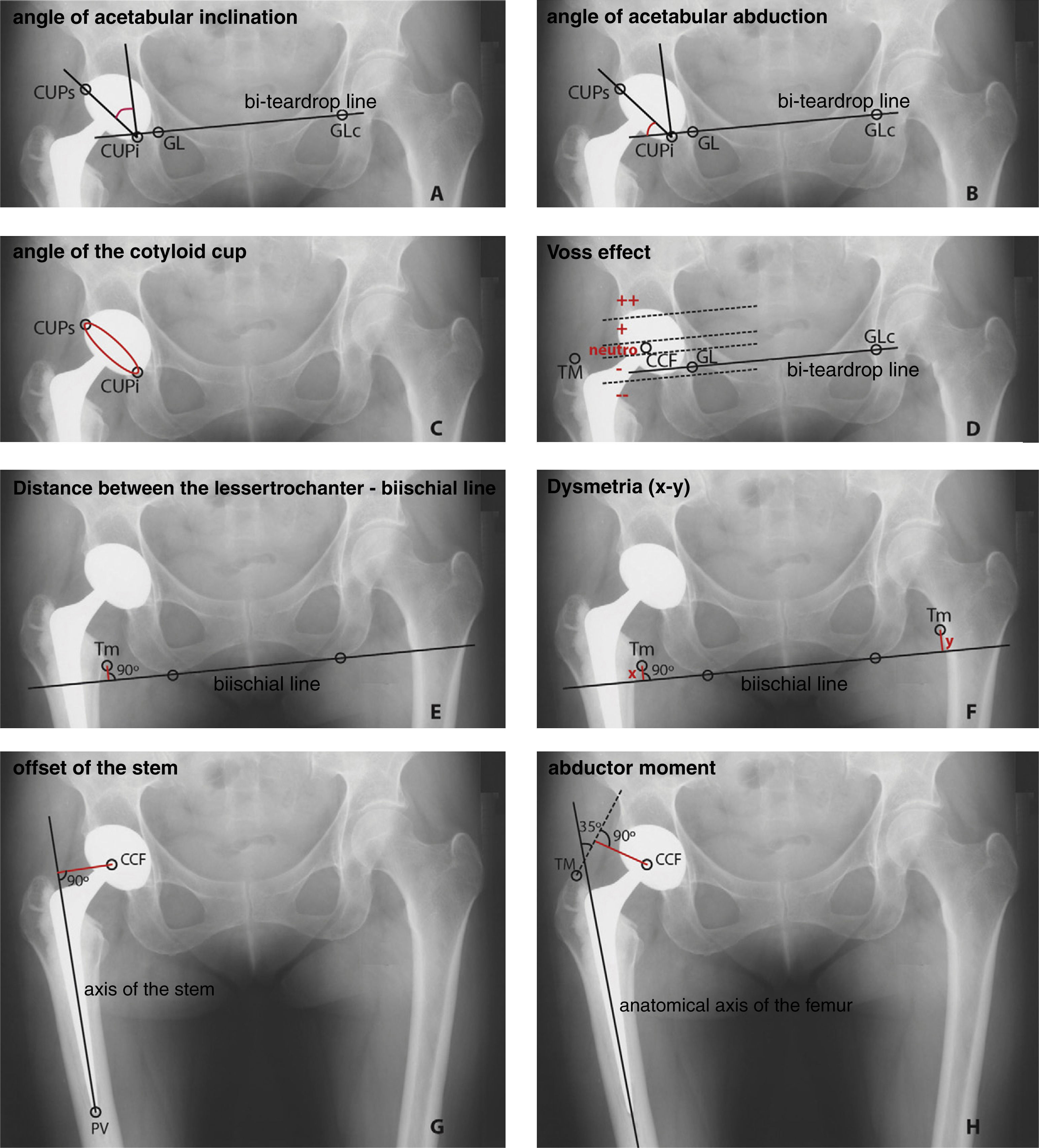
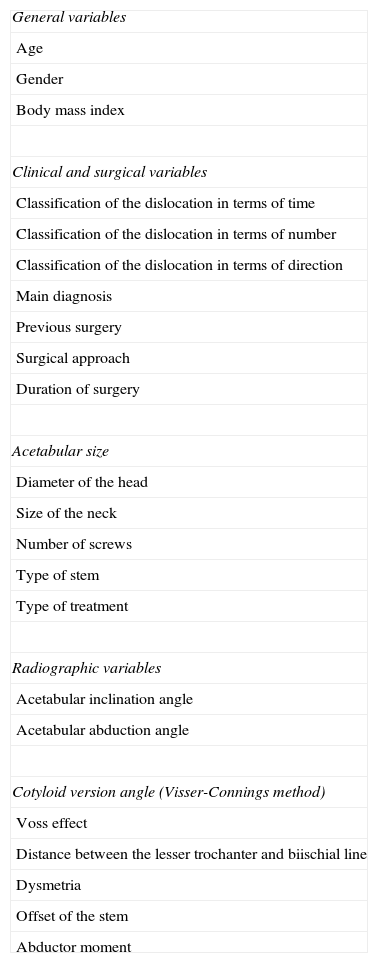
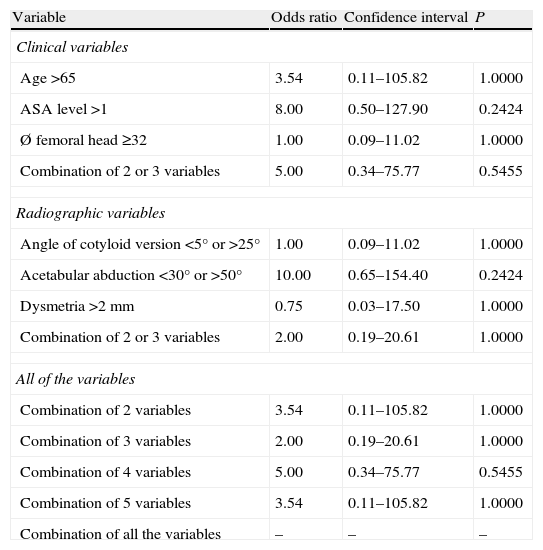
Study variablesIn Table 1, all the variables analysed are presented, separated into 3 groups according to whether they belong to patient data, surgical data or measurements carried out in the corresponding analysis. The method to determine the latter by using computer applications is shown in Fig. 1.
List of general, clinical-surgical and radiographic variables analysed in the study.
| General variables |
| Age |
| Gender |
| Body mass index |
| Clinical and surgical variables |
| Classification of the dislocation in terms of time |
| Classification of the dislocation in terms of number |
| Classification of the dislocation in terms of direction |
| Main diagnosis |
| Previous surgery |
| Surgical approach |
| Duration of surgery |
| Acetabular size |
| Diameter of the head |
| Size of the neck |
| Number of screws |
| Type of stem |
| Type of treatment |
| Radiographic variables |
| Acetabular inclination angle |
| Acetabular abduction angle |
| Cotyloid version angle (Visser-Connings method) |
| Voss effect |
| Distance between the lesser trochanter and biischial line |
| Dysmetria |
| Offset of the stem |
| Abductor moment |
Representation of the radiographic measurements analysed with the Trabeculae® SACRA-ATC® application. (A) The angle of acetabular inclination is formed by the line that crosses the CUPs and the CUPi with the perpendicular of the bi-teardrop line. (B) The angle of acetabular abduction is calculated as that complementary to the angle of acetabular inclination. (C) The angle of the cotyloid cup model in the AP plane is determined using the Visser-Connings method. (D) The Voss effect is given by the distance between the GT and the CFH. If both are parallel, the Voss effect is neutral; if the GT is below the CFH, it is negative; and if it is above the CFH, it is positive. (E) The distance between the LT of the affected femur and the biischial line. (F) Dysmetria is calculated as the difference between the biischial GT line of the affected side and that of the contralateral joint. (G) The offset of the stem is the distance between the CFH to the longitudinal axis of the artificial joint stem. (H) The abductor moment is calculated by tracing a line from the GT that forms a 35° angle with the anatomical axis of the femur, and measuring the distance between this and the CFH. CUPi, lowest internal point of the dome plane; CUPS, highest external point of the dome plane; CFH, centre of the femoral head; GT, greater trochanter; LT, lesser trochanter; ST, stem tip; TDC, teardrop on the contralateral joint; TDS, teardrop of the affected side.
The data obtained were gathered in a database, which was later exported to the statistical package SPSS 15.0 (SPSS Inc., Chicago, IL, USA), a computer application that carried out the statistical analysis of the variables. A common descriptive study for the quantitative variables was undertaken, with a confidence level of 95% for all of them. Due to the low number of cases, the criteria for data normality were not complied with, and the Mann–Whitney–Wilcoxon U test was therefore used for means comparison. The comparison of qualitative variables was undertaken using the Chi squared test.
Association strength was determined calculating the odds ratio with confidence intervals of 95%. The statistical programme Epidat 3.1 (a programme for the epidemiological analysis of tabulated data, Ministry of Health, Xunta de Galicia) was used to carry out this analysis.
ResultsWe found a total of 7 dislocations (no cases of bilateral dislocation), representing an incidence rate of 1.75%. One of these 7 cases was rejected for the risk factor study as it was impossible to gather all the clinical data and X-rays necessary for its analysis. The chronology of the dislocations was 4 early dislocations against 2 late ones, the late ones being considered as those that occurred later than 3 months after the date of surgery.
In 3 cases the patients with dislocations were male, while all patients in the control group were male (P=0.046). The mean age of the group with dislocation was 61±11 years, this being similar in females (66±15) and males (56±4) (P=0.400). The mean age of the control group was 47±12 years old, less than in the group with dislocation (P=0.065). The mean IMC of the group with dislocation was 28.6±5.7g/cm2, with the control group also being less (26.7±4.8g/cm2).
The main diagnosis in 3 of the cases of dislocation was primary osteoarthritis, compared to 3 that had been diagnosed with avascular necrosis. Four patients presented a normal acetabulum compared with 2 who had protusio acetabuli. Five of the patients presented a Dorr type 1 femur, while 1 of them had a type 2 femur. There were no significant differences with the control group regarding acetabular and femoral morphology (P=0.426).
In 5 of the cases of dislocation, the surgical approach was posterior, with only 1 lateral approach. In the control group, there were 4 posterior approaches and 2 lateral (P=0.505).
The average size of the acetabular component in the group with dislocation was 52±3.7mm, with the maximum size being 56mm and the minimum 46mm.
In 4 of the cases of dislocation, a femoral head with a diameter of 32mm had been used, while a 28mm diameter used in only 2. The control group was also composed of 4 hip replacements with a diameter of 32mm and 2 with a diameter of 28mm.
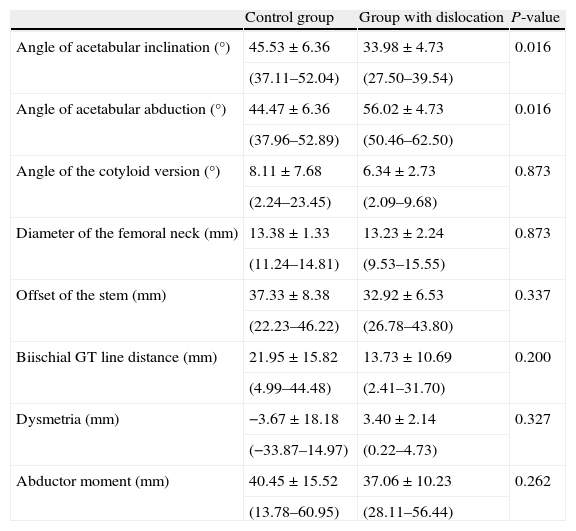
With respect to the X-ray variables, the angle of acetabular inclination was 33.98±4.73° in the group with dislocation, against 45.53±6.36° in the control group (P=0.016). This variable and, evidently, the angle of acetabular abduction (complementary angles), are the only radiographic parameters that present significant differences between both groups.
The results of the radiographic variables analysed for not only the group with dislocation but also the control group are shown in Table 2.
Results of the analysis of radiographic variables in the non-dislocated THR group (control group) and in the THR group with dislocations.
| Control group | Group with dislocation | P-value | |
| Angle of acetabular inclination (°) | 45.53±6.36 | 33.98±4.73 | 0.016 |
| (37.11–52.04) | (27.50–39.54) | ||
| Angle of acetabular abduction (°) | 44.47±6.36 | 56.02±4.73 | 0.016 |
| (37.96–52.89) | (50.46–62.50) | ||
| Angle of the cotyloid version (°) | 8.11±7.68 | 6.34±2.73 | 0.873 |
| (2.24–23.45) | (2.09–9.68) | ||
| Diameter of the femoral neck (mm) | 13.38±1.33 | 13.23±2.24 | 0.873 |
| (11.24–14.81) | (9.53–15.55) | ||
| Offset of the stem (mm) | 37.33±8.38 | 32.92±6.53 | 0.337 |
| (22.23–46.22) | (26.78–43.80) | ||
| Biischial GT line distance (mm) | 21.95±15.82 | 13.73±10.69 | 0.200 |
| (4.99–44.48) | (2.41–31.70) | ||
| Dysmetria (mm) | −3.67±18.18 | 3.40±2.14 | 0.327 |
| (−33.87–14.97) | (0.22–4.73) | ||
| Abductor moment (mm) | 40.45±15.52 | 37.06±10.23 | 0.262 |
| (13.78–60.95) | (28.11–56.44) |
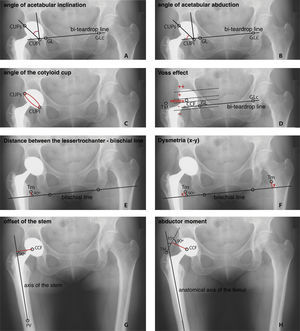
Using the clinical variables (age, ASA level and diameter of the femoral head) and the radiographic variables (angle of cotyloid version, angle of acetabular abduction and dysmetria), we have analysed the different patient groups using 2×2 tables and odds ratios (probability of reasons). When the different variables were analysed individually, none of them was statistically significant, probably due to the small number of cases of dislocation in the series. The same thing happened when the variables were analysed jointly (Table 3).
Odds ratio.
| Variable | Odds ratio | Confidence interval | P |
| Clinical variables | |||
| Age >65 | 3.54 | 0.11–105.82 | 1.0000 |
| ASA level >1 | 8.00 | 0.50–127.90 | 0.2424 |
| Ø femoral head ≥32 | 1.00 | 0.09–11.02 | 1.0000 |
| Combination of 2 or 3 variables | 5.00 | 0.34–75.77 | 0.5455 |
| Radiographic variables | |||
| Angle of cotyloid version <5° or >25° | 1.00 | 0.09–11.02 | 1.0000 |
| Acetabular abduction <30° or >50° | 10.00 | 0.65–154.40 | 0.2424 |
| Dysmetria >2mm | 0.75 | 0.03–17.50 | 1.0000 |
| Combination of 2 or 3 variables | 2.00 | 0.19–20.61 | 1.0000 |
| All of the variables | |||
| Combination of 2 variables | 3.54 | 0.11–105.82 | 1.0000 |
| Combination of 3 variables | 2.00 | 0.19–20.61 | 1.0000 |
| Combination of 4 variables | 5.00 | 0.34–75.77 | 0.5455 |
| Combination of 5 variables | 3.54 | 0.11–105.82 | 1.0000 |
| Combination of all the variables | – | – | – |
The rate of dislocation after primary THR with a metal–polyethylene joint is usually between 3% and 5%,20–22 although there are studies where an even greater incidence rate has been found.23,24 In this study using the ceramic acetabular Trident® system, we found an incidence rate of dislocation of 1.75%, less than that of series where conventional joints were used. This incidence rate is also in concordance with the value reflected in the work of Colwell et al.,14 where the author had dislocation of 1.1% in a series of 1635 hip replacements with a ceramic–ceramic joint undertaken over a 3-year period.
General, clinical and surgical variablesA patient's advanced age has been associated with a greater risk of dislocation in various studies.21,25,26 However, other works do not reflect this relationship.27–29 In our case, the results for the group with dislocation were 61±11 (52–83) years old, and 47±12 (26–59) years old for the control group. Although no significant differences were found (P=0.065), a circumstance that was possibly due to the small number of patients with dislocation, there does seem to be a certain tendency for an increase in dislocations as the age of the patient increases.
Likewise, there is also no agreement as to whether the dislocations are more common in females than in males. Although some studies dismiss this theory,27 others refute it.30 In our study, we found a greater incidence of dislocations in females (2.02%) with respect to males (1.18%), even if the results were not significant (P=0.808).
The IMC was not significant when comparing cases of dislocation with the control group.
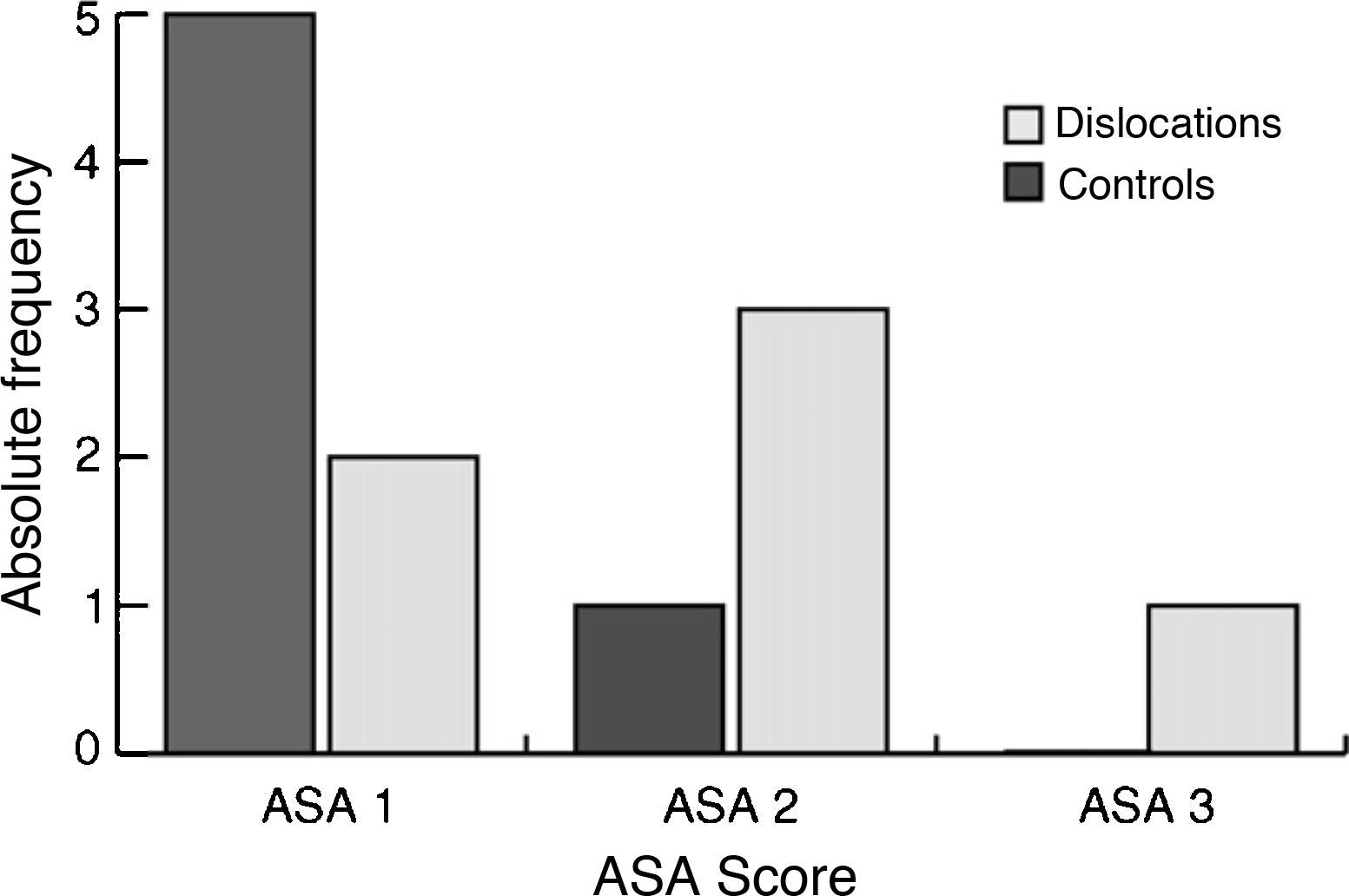
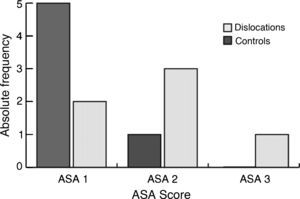
In 2002, Jolles et al.,2 concluded that the ASA anaesthetic risk level was an important factor in risk of dislocation after a primary THR. In their work, an ASA level equal to or greater than 3 was highly predictive of dislocation (P=0.01). In our case, the differences in the ASA level in the patients studied were not significant (P=0.132); even so, we see a growing tendency of this value in the group with dislocation (Fig. 2).The influence that the type of clinical diagnosis could have on the incidence of dislocations has been assessed by different authors. In our study, patients initially diagnosed with avascular necrosis seem to present a greater relative risk (RR) of dislocation compared to patients diagnosed with primary osteoarthritis (RR=2.01), although the differences are not significant due to the low number of cases of dislocation. These results are consistent with those reflected in other works, where the diagnosis of avascular necrosis is considered a risk factor for artificial joint dislocation.31–33
The type of surgical approach also seems to affect the rate of dislocation in the entire series. Woo and Morrey23 had 5.8% dislocations in THR with a posterolateral approach. In 2001, Levi and Gebuhr24 confirmed these results when they had 5.6% of dislocations in a series of 427 primary THRs with posterolateral approach without reinsertion of the external rotators.24 However, in work where this surgical technique is added to the posterior approach, the rates of dislocation drop to 2%.34 When an anterolateral approach is used, the rate of dislocation is about 2.3%.23 Although in our case we found 5 dislocations of hip replacements using the posterior approach and only 1 with lateral approach, there were no significant differences with the control group (P=0.699) or with the entire series (P=0.168).
In recent years, there have been studies that show an upward trend in the risk of dislocation with the decrease in size of the femoral head.22,33 In these studies, femoral heads of 22–36mm in diameter were used. In our study, the heads used were 28mm, 32mm or 36mm, and there were no significant differences found between the different diameters (P=0.322). This was also probably due to the low number of cases of dislocation. We should point out that no 36mm diameter head was dislocated in our series, which is why the sizes of the femoral heads larger than 32mm could act as a limiting factor in the risk of artificial joint dislocation.
We did not see significant differences in the rest of the clinical and surgical variables (size of cotyloid cup, size of neck, type of femur, etc.).
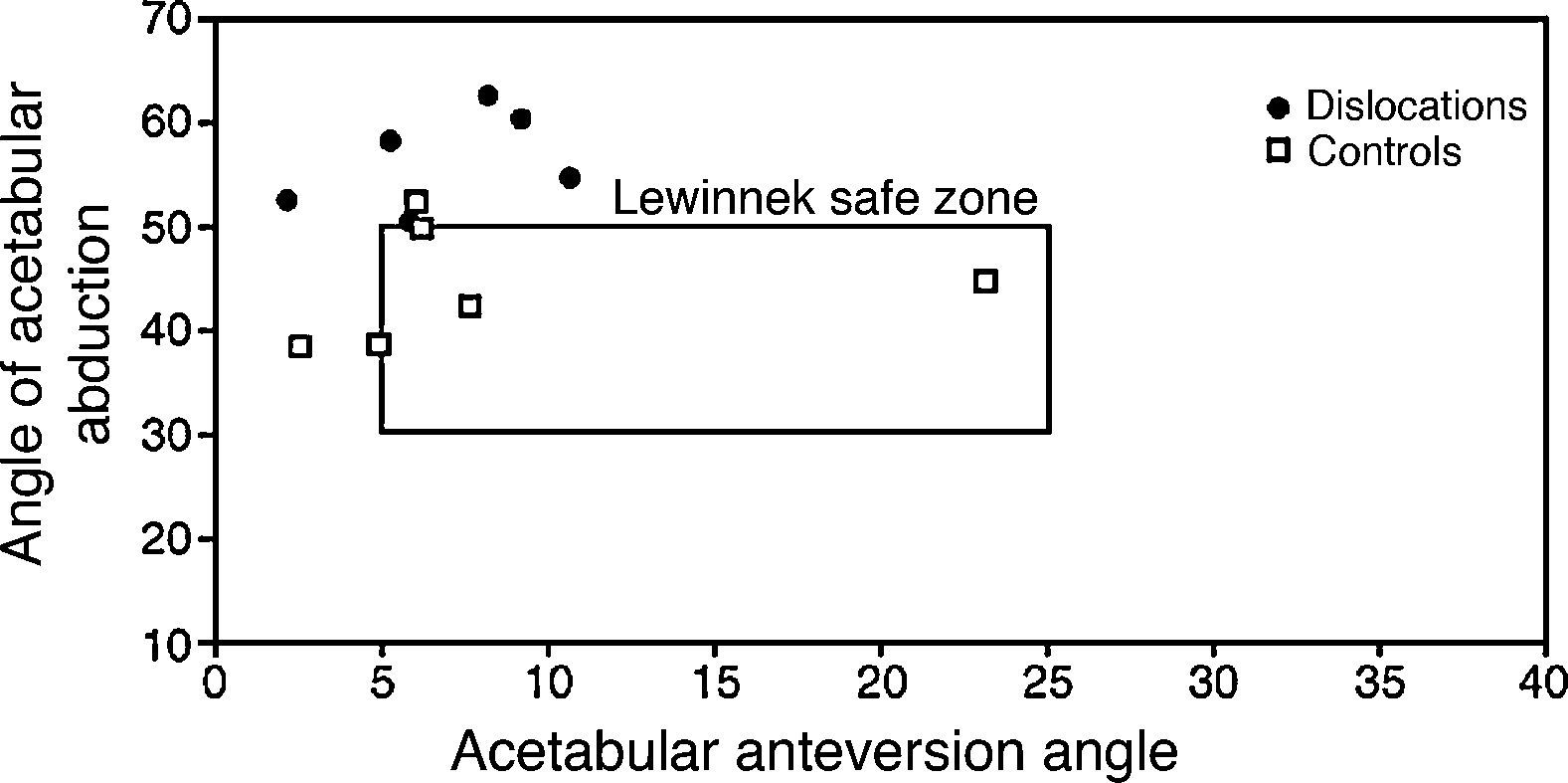
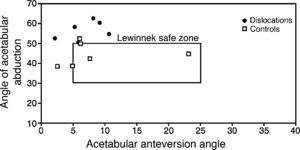
Radiographic variablesThere has been no agreement yet on the best position for the artificial joints to achieve the greatest stability and minimise the risk of dislocation. Müller35 proposed an acetabular anteversion of between 10° and 15°.35 However, Harris recommended 20–25°.36 Lewinnek et al.,20 correlated acetabular abduction and anteversion, describing a “safe zone” of between 30–50° of abduction and 5–25° of anteversion where the risk of dislocation was much less.
Although the theory of the Lewinnek safe zone is quite accepted, there are some studies that suggest that it is not valid in all circumstances. Masaoka et al.37 found that 40% of the dislocations in their series were within the safe zone.37 Other groups have gone even further by proposing that the best implant orientation should change according to the surgical approach used in the hip replacement; when carrying out a posterior approach, they would recommend a greater anteversion of the acetabular component than when there is a lateral or anterolateral approach.38 Other groups have even suggested changing the implant orientation according to the patient's gender, recommending anteversion around 45° in females and only 20–30° in males.39
In this study, although the cases of dislocation and the controls had similar values for the angle of the cotyloid cup model, we did find significant differences in the angle of acetabular abduction between both groups (P=0.015). We observed that the values of the cases of dislocation are further away from the Lewinnek safe zone (Fig. 3), results that coincide with those obtained by Giurea et al.,40 who showed there was a greater angle of acetabular inclination (P=0.02) in the group with dislocation (40 THRs) in a series of 2,605 THR.40
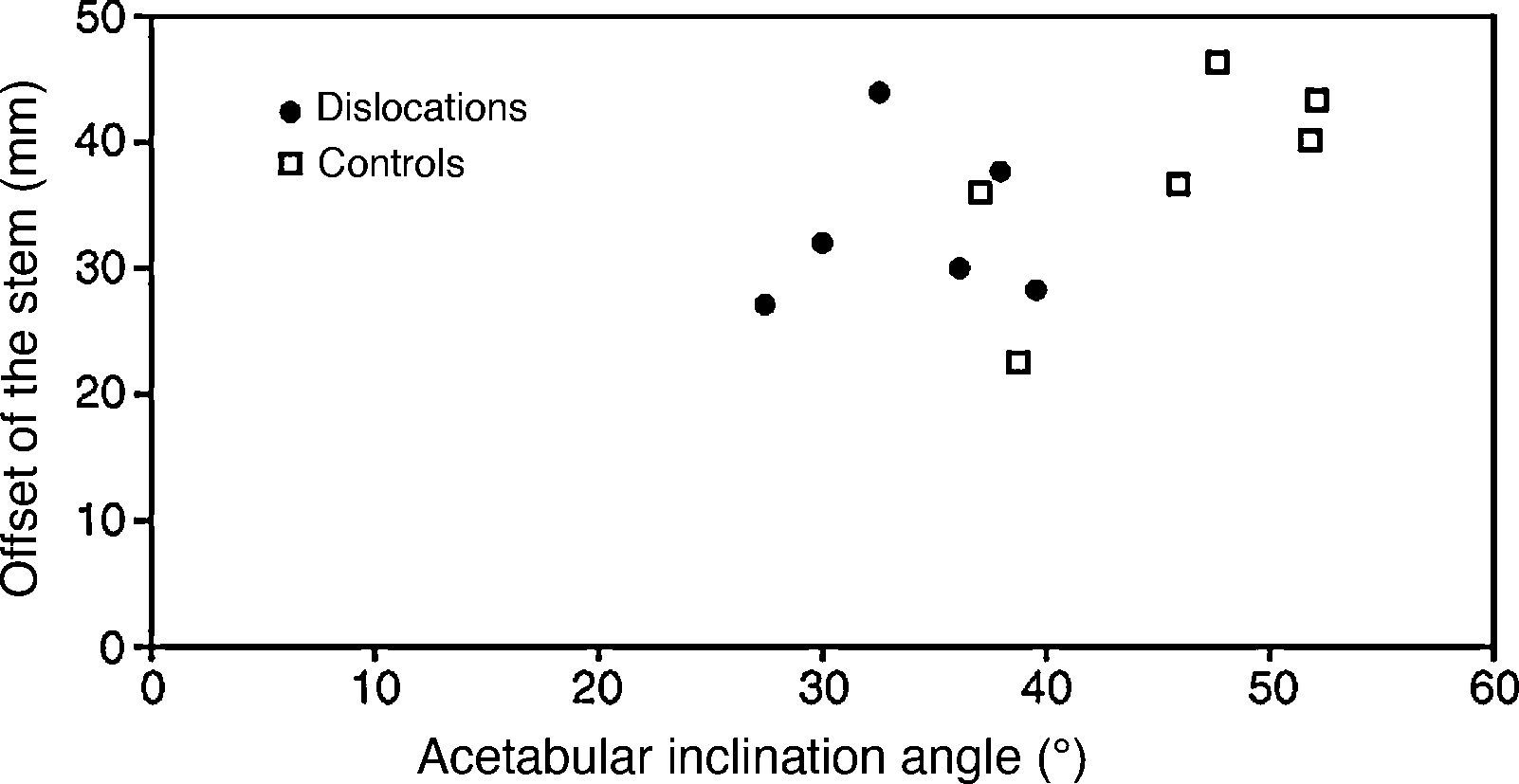
No significant differences were found between the control group and the group of cases of dislocation for the rest of the radiographic variables studied (Voss effect, dysmetria, abductor moment and offset of the stem).
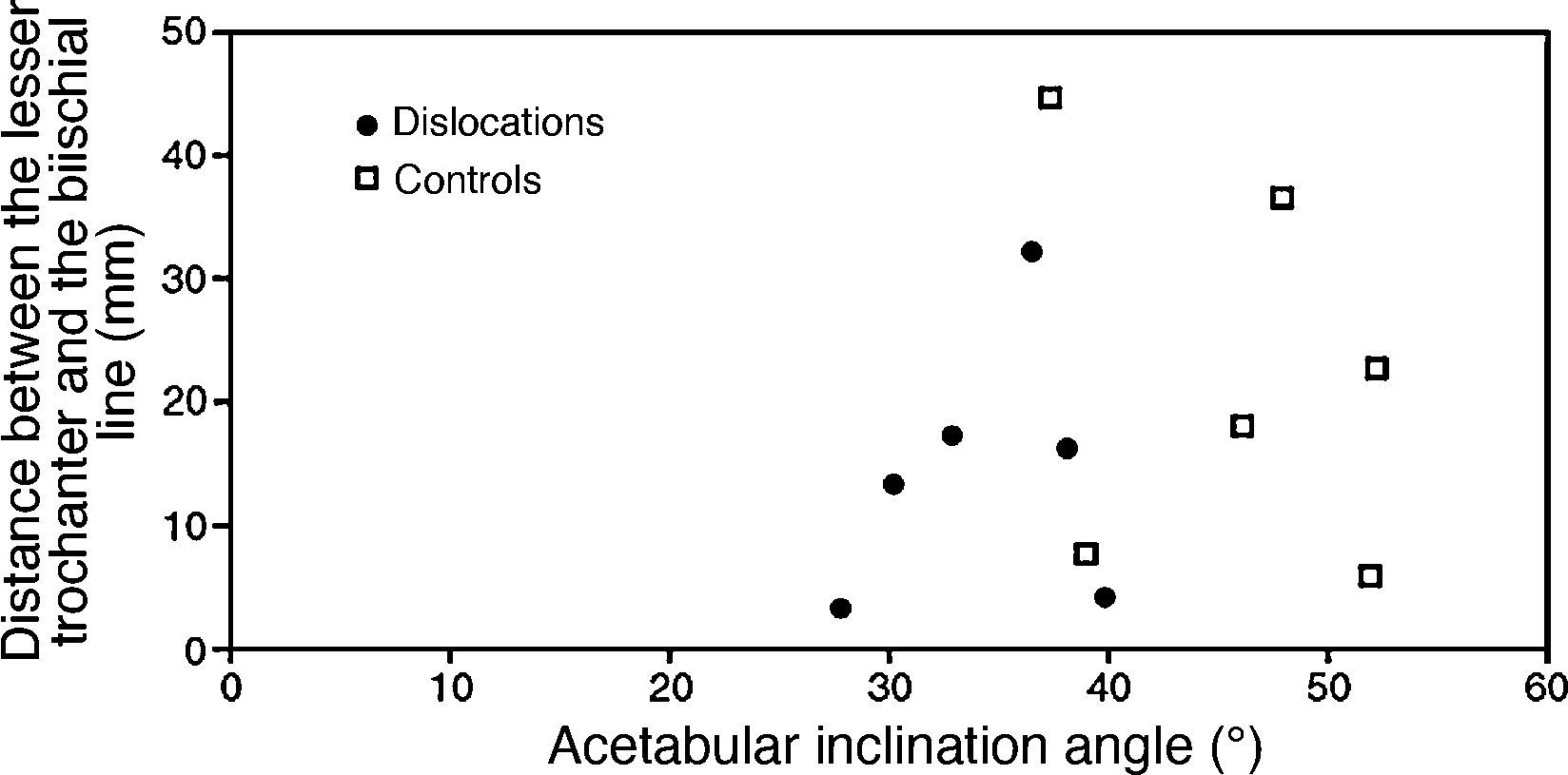
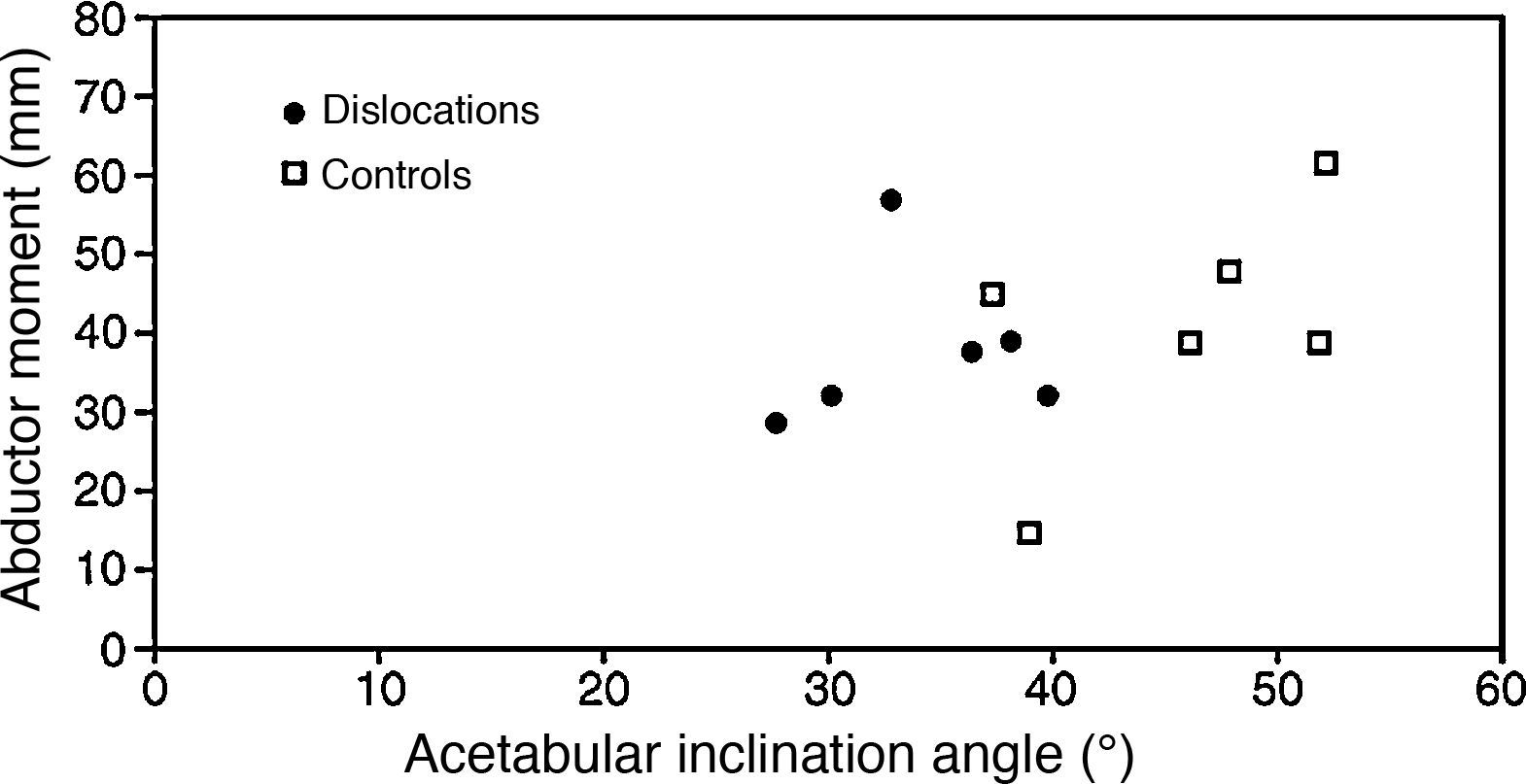
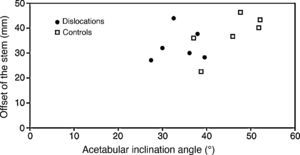
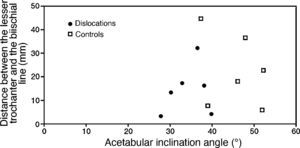
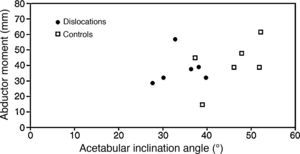
So as to establish other safe zones like those proposed by Lewinnek, we depict the offset of the stem, the distance between the lesser trochanter and the biischial line and the abductor moment compared to the acetabular inclination angle in Figs. 4–6, respectively. As can be seen in these figures, there are no significant differences between both groups for the values of the different variables represented.
Many risk factors for dislocation after THR have been found in different studies, ranging from the patient's own characteristics such as age and gender, to factors that are solely clinical or surgical. In this study, the most significant variable was the angle of acetabular abduction, with big differences being seen between the control group studied and the cases of dislocation. Other variables, such as the subject's age or ASA level, show trends that are not statistically significant, although we believe that this is due to the low number of patients with dislocation found in the series. In this study, we did not find significant differences between the different diameters regarding risk of dislocation; even so, a femoral head larger than 32mm could act as a limiting risk factor of artificial joint dislocation.
We consider that the greatest limitation of this study was precisely the low number of patients presenting artificial joint dislocation. Despite the fact that the study included a series of 401 THRs, the low incidence rate of dislocation with the ceramic acetabular Trident® system (7 cases) could have hidden some significant differences when compared to the control group in some of the variables analysed.
FinancingThis research has been performed thanks to funding by Stryker Iberia.
Evidence levelEvidence level IV.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank Stryker Iberia for funding this research.
Grupo de Estudio Español del Sistema Acetabular Trident® de Cerámica: Fermín Abellá, Agustín Blanco, Luis Bonilla, Antonio Bru, José M. Fernández-Carreira, Roberto Casal, Guillermo de la Barreda, José L. Díaz-Almodóvar, Luis Espejo, Roberto Iglesias, Carlos Jiménez, Manuel Monfort, Fernando Muñoz, Antonio Murcia, Luis García-Paíno, Santiago Suso, Jenaro A. Fernández-Valencia.
Please cite this article as: Caeiro JR, et al. Incidencia y factores de riesgo de luxación tras artroplastias totales de cadera con sistema acetabular de cerámica. Rev esp cir ortop traumatol. 2011;55(6):437–445.