Minimally invasive total knee arthroplasty performed by orthopaedic surgeons who are specialised in total knee arthroplasty leads to similar functional results and rates of complications as conventional procedures. The aim of this study is to find out whether this can be extrapolated to general orthopaedic surgeons, and also to describe the learning curve in this procedure.
Materials and methodsWe included 259 patients over a three-year period. The population was divided into 10 groups, 26 knee replacements in each group, allocated in chronological order. The following variables were recorded: hospitalisation in days, radiological angles, length of incision, tourniquet time, complications, Hospital for Special Surgery (HSS) score, haemoglobin values and need for blood transfusion.
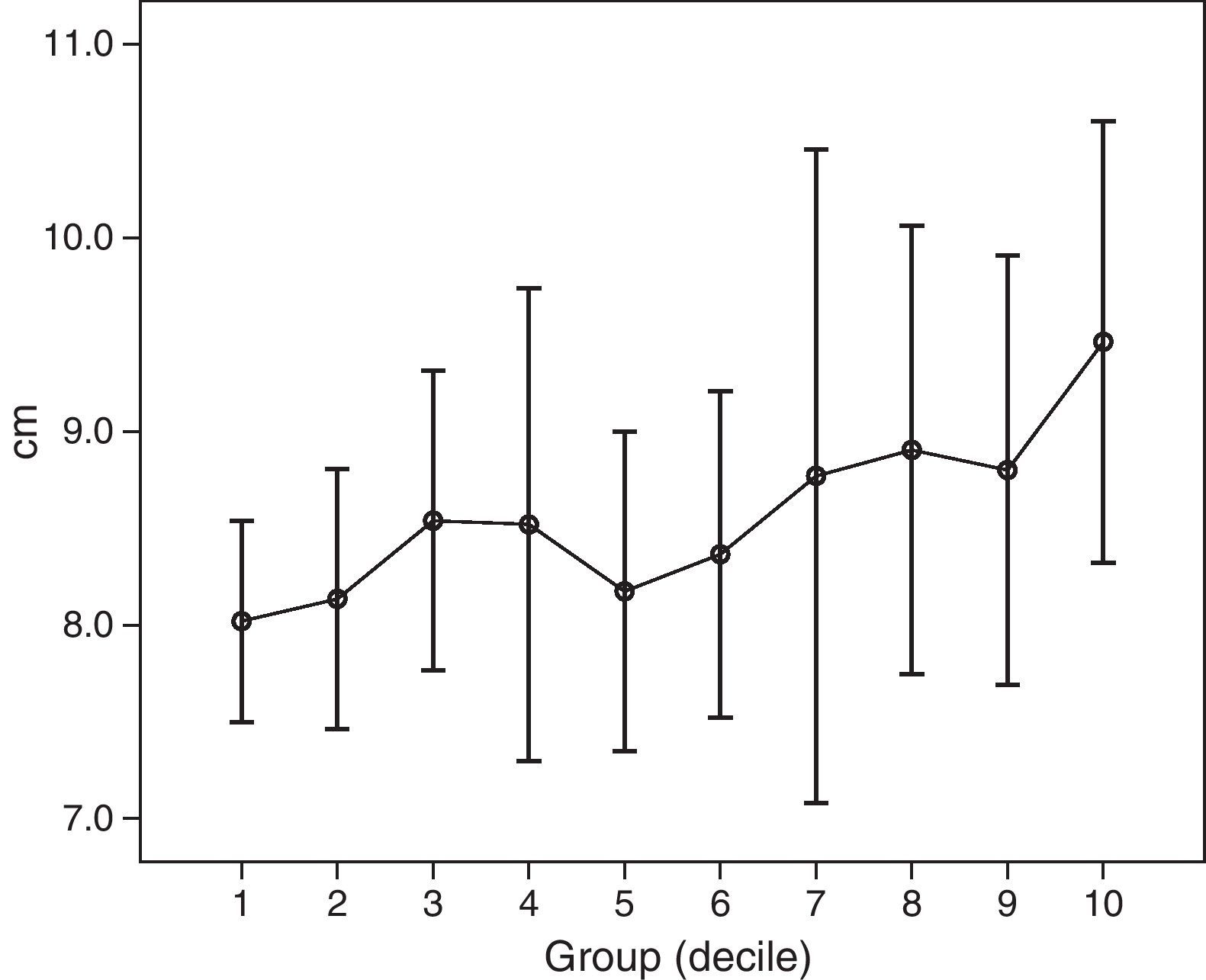
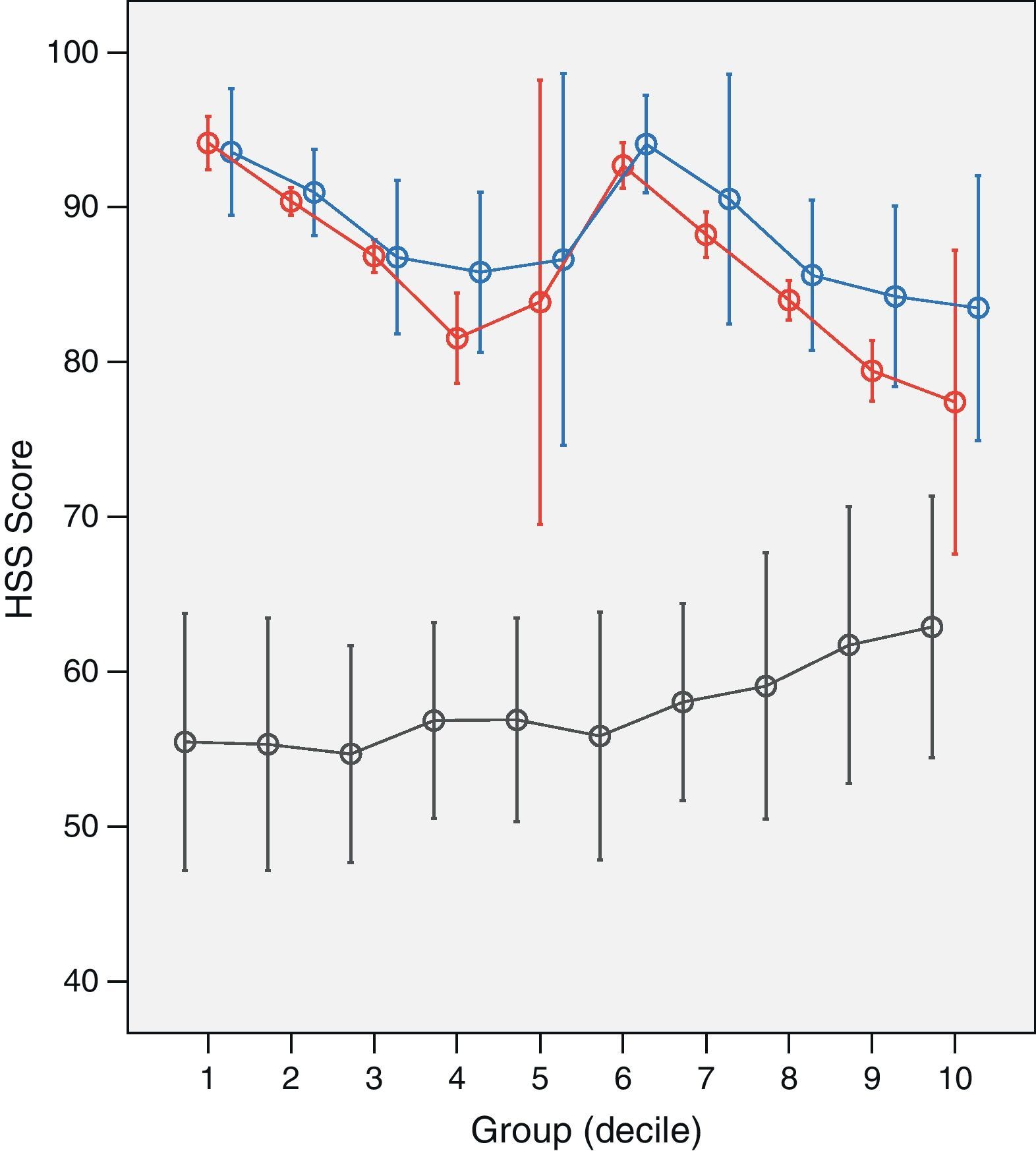
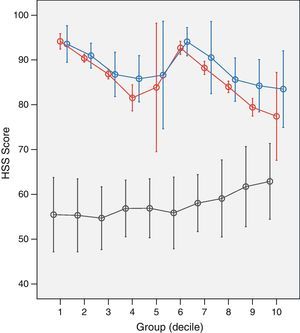
ResultsThe mean number of hospitalisation days decreased from 7.9 to 6.2 days. Mean tourniquet time decreased from 120±15 to 95±20min. Packed red blood cells administration decreased from a median of 2 packed cells to 0. Mean incision length increased from 8±0.5 to 9.5±1.1cm. Complications dropped from 11.5% to 3.8%. No differences were observed in the radiological angle of the prosthesis and HSS scores of patients in the different groups, 6 months and one year after surgery.
ConclusionsMinimally invasive total knee replacement surgery (MIS) can be performed by general orthopaedic surgeons with results that are comparable in the medium-term with conventional surgery, and with the short-term advantages afforded by MIS. The learning curve was 26 knee replacements. The variables that improve were tourniquet time, need for blood transfusion and length of hospitalisation. The final functional result and radiological positioning were not affected.
Distintos estudios demuestran que la prótesis total de rodilla por un abordaje mínimamente invasivo (CMI) tiene unos resultados funcionales y complicaciones semejantes a las series clásicas. Se pretende estudiar si esto es extrapolable al cirujano ortopédico general y describir la curva de aprendizaje.
Material y métodoSe incluyen 259 pacientes prospectivamente durante tres años. Se dividieron en 10 grupos de 26 prótesis cada uno, por orden cronológico. Se relacionaron las siguientes variables: días de ingreso, ángulos radiológicos, longitud de la incisión, tiempo de isquemia, complicaciones, puntuación de la escala HSS, niveles de hemoglobina y necesidad de transfusión sanguínea.
ResultadosLa media de días de ingreso hospitalario disminuyó de 7,9 días a 6,2 días. El tiempo medio de isquemia pasó de 120±15 a 95±20minutos. Disminuyó la necesidad de transfusión. La longitud de la incisión aumentó de 8±0,5 a 9,5±1,1cm. El número de complicaciones descendió de 11,5% a 3,8%. No se encontraron diferencias en la colocación radiológica de los componentes ni en la escala HSS a los 6 meses ni al año.
ConclusionesLa prótesis de rodilla por CMI tipo Quad Sparing realizada por un cirujano ortopédico general ofrece resultados a medio plazo equiparables a la cirugía convencional, con las ventajas de la CMI a corto plazo. La curva de aprendizaje para esta técnica es de 26 prótesis mejora el tiempo de isquemia, la necesidad de transfusión sanguínea y los días de ingreso hospitalario, no influye el resultado funcional final ni la colocación radiológica.
Total knee replacement has proven to be effective for long-term pain reduction and for enhancing functional recovery in patients with arthritis of the knee.1 Ongoing improvement in the design of the materials and in surgical techniques has made this surgery successful. The development of surgical approaches that are less aggressive and more sparing of the soft tissues has improved the post-operative course and short-term results in total knee replacement.
A number of minimally invasive surgery (MIS) techniques have been described for implantation of a total knee prosthesis.2–14 The subvastus approach avoids cutting the quadriceps and may promote faster recovery following the prosthesis.15,16 Bonnutti et al.17 have used an MIS technique successfully on more than 420 knees. Laskin has reported good results using a limited midvastus approach.18 Tria and Coon13 have published data using the medial parapatellar limited subvastus approach known as the quad-sparing approach. The first articles published comparing the different techniques and surgical approaches show slight differences in terms of the clinical results and complications associated with the learning curve for each technique.
The ideal minimally invasive technique for total knee replacement should retain the quality and safety of today's conventional approach, using the appropriate instruments to make a more limited skin incision, thereby minimizing damage to the extensor mechanism and soft tissues of the knee. This technique should also feature conservative bone resection, precision components placement, and meticulous prosthesis cementing, and it must not compromise the final functional results of the prosthesis.
The objective of this study is to analyse whether MIS is a procedure indicated for performance by general orthopaedic surgeons in a tertiary hospital; to determine whether the learning curve in these cases is longer; to evaluate whether it offers the patient better short-term functional results and a lower incidence of complications than other techniques; and to identify objective patient parameters that would contraindicate a minimally invasive approach.
Materials and methodsClinical information was obtained using a protocol specifically designed for this study. This protocol was developed on the basis of the Hospital for Special Surgery's knee assessment system (HSS Knee Score).19 The protocol and the questionnaire were tested 1 month prior to the study, and this served as training for the personnel who would be conducting the survey.
Information on the patients was collected in the clinic 1 month prior to the intervention, during the hospital admission, and at 6 months and 1 year after the surgery. All factors were evaluated prospectively. All clinical interviews were conducted by an orthopaedic surgeon from the Orthopaedic Surgery and Traumatology Service who, in all cases, knew the study protocol beforehand. At the pre-operative visit, the patient's demographic and clinical information was recorded, and weight-bearing X-rays were taken. During the patient's hospital admission, the following information was collected: medical treatment received, variables recorded during the procedure and in the recovery room, the need for transfusions, the degree of joint mobility, the date of hospital discharge, and complications, if any, during the admission. A post-discharge follow-up period was established with functional and X-ray evaluation. This included check-ups at 6 weeks, 6 months, and 1 year following the surgical procedure. Follow-up data was obtained in the respective clinics, and control X-rays of the prosthesis were taken the same day as the clinic appointment. X-rays (anteroposterior and lateral projections) were taken weight-bearing. All radiographic angles were measured by the same orthopaedic surgeon from the hospital to whom the primary surgeon performing the procedure was unknown. The study took place over a period of 3 years.
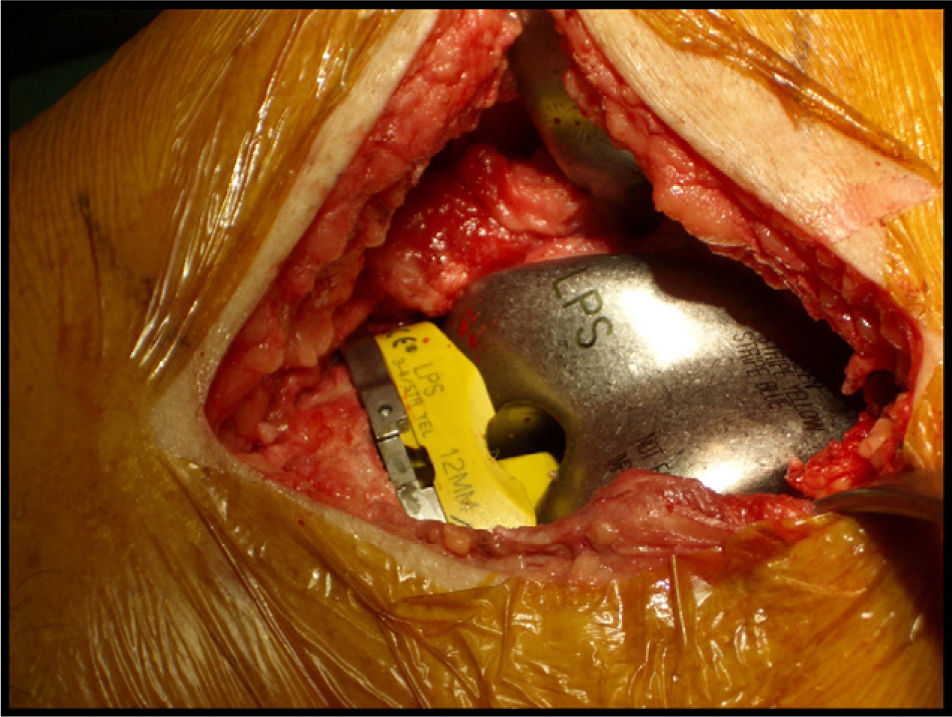
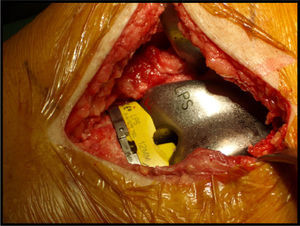
Inclusion criteria and patient selectionThe study enrolled 259 patients who had been diagnosed radiographically with osteoarthritis of the knee by the hospital's Orthopaedic Surgery and Traumatology Service and for whom medical treatment to control the osteoarthritic pain had failed. A Zimmer® NexGen Legacy PS total knee prosthesis was implanted in all study patients using a limited subvastus approach without invasion of the vastus internus (quad-sparing13).
Exclusion criteriaAll patients who did not meet the criteria for indications for this surgical technique were excluded. We defined the exclusion criteria on the basis of other studies previously published.13,20 This group included patients who had previous surgeries on that joint via a different surgical approach; valgus or varus deformities of more than 20° in the joint; flexion contractures of more than 10° in the knee with less than 90° range of motion; ligament instability; as well as patients who refused this type of surgery. The patient's age, body mass index (BMI) and previous pathology were not used as exclusion criteria.
Parameters evaluated during the studyThe following parameters were recorded prospectively by a single observer:
- –
Pre-operative data: age, sex, side, BMI, previous state of health (ASA classification), haemoglobin and hematocrit levels, pre-operative HSS score.
- –
Pre-operative X-rays: anatomical femorotibial angle in coronal plane on weight-bearing X-ray.
- –
Intra-operative data: date of the intervention, ischaemia time, primary surgeon and assistants who performed the procedure.
- –
Post-operative data: length of the incision in extension, haemoglobin and hematocrit levels, number of blood transfusions, range of motion at discharge, date of discharge from hospital.
- –
Intra-operative and post-operative complications.
- –
Post-operative data at 6 months: post-operative HSS score, plain X-ray.
- –
Post-operative data at 12 months: post-operative HSS score.
Any axial deviation of 5° or more from the ideal was defined as a poor radiographic result.21,22 The ideal femorotibial alignment in the coronal plane was considered to be 6° of valgus, with the femoral component at 5–7° of valgus and the tibial implant at neutral.5 We considered a femorotibial angle of 6°, a distal femoral angle of 6° of valgus, and a proximal tibial angle at neutral to be ideal.
Statistical analysisFor the statistical analysis, the Student's t-test and the non-parametric Mann–Whitney test were used for group comparison and the Wilcoxon test for paired data. ANOVA (analysis of variance) and the Student–Newman–Keuls multiple comparison test for 3 or more groups were used. Results were expressed as the mean±standard deviation (SD). Categorical variables were compared using the χ2 test and a non-parametric test to relate the dichotomous variables. For all tests, a significance value of less than .05 was accepted in bilateral comparison. SPSS version 14.0 was used for the statistical analysis. The mean and standard deviation are shown in bar graphs.
Pre-operative dataThe study included 259 cases: 184 females (71%) and 75 males (29%), with a mean age of 71.02±8.68 years (range: 36–88). In 130 cases (50.2%), it was the right knee. The most common aetiology was primary osteoarthritis in 249 patients (96.1%), followed by osteoarthritis secondary to rheumatoid arthritis in 5 patients (1.9%); osteoarthritis secondary to trauma in 3 patients (1.2%); osteoarthritis secondary to osteonecrosis in 1 patient (0.4%); and osteoarthritis secondary to septic arthritis in 1 patient (0.4%). The mean BMI was 30.85±4.96kg/m2 (range: 15.76–49.52). In terms of anaesthesia risk classification, 8 patients were ASA 1, 196 were ASA 2, 52 were ASA 3, and 3 were ASA 4. The mean pre-operative haemoglobin level was 13.7±1.2g/dL (range: 10.6–17.7), and for hematocrit it was 40.8%±3.9% (range: 31.3–52.9%). All patients had a normal pre-operative coagulation study. The pre-operative HSS score was 57.65±8.05 points.
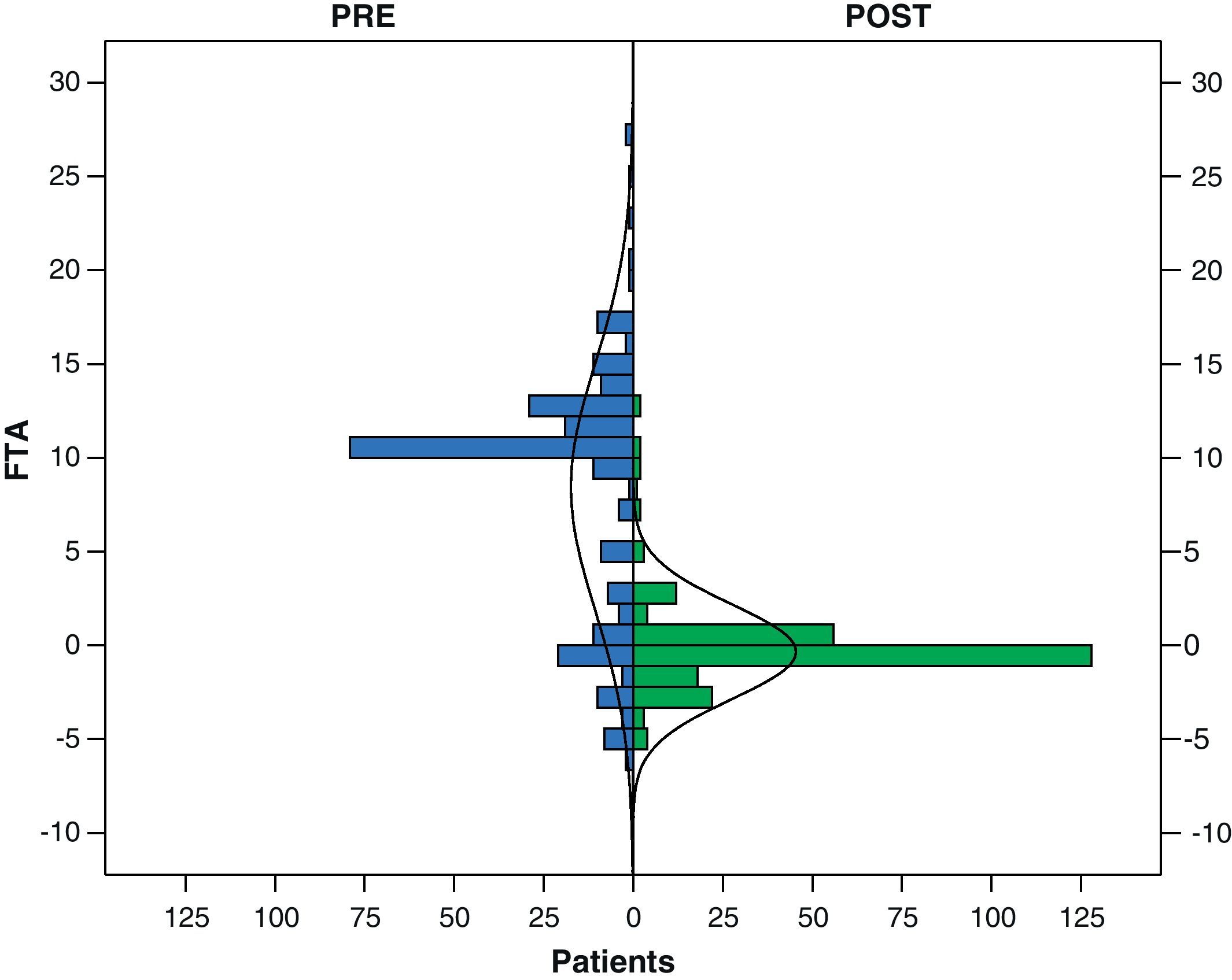
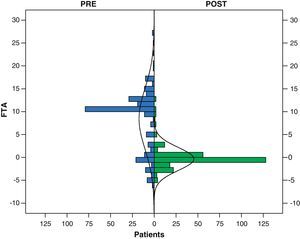
On X-ray, the femorotibial angle in the coronal plane was +8.44°±6.63° (range: +21° varus to 12° valgus); 38 (14.7%) had an initial valgus deformity and 200 (77.2%) a varus deformity, while 21 (8.1%) had no axis changes.
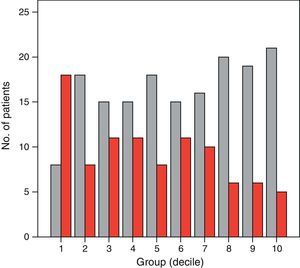
Intra-operative dataSince this surgical technique was implemented on the Service, 11 traumatologists have participated as primary surgeons. The decile distribution is by chronological order. Before performing the prosthesis surgery, the primary surgeon participated in other interventions as first or second assistant. The results are detailed below. Since this surgical technique was implemented on the Service, 11 traumatologists have participated as primary surgeon – surgeon 1 (97 prostheses), surgeon 2 (54 prostheses), surgeon 3 (36 prostheses), surgeon 4 (11 prostheses), surgeon 5 (21 prostheses), surgeon 6 (9 prostheses), surgeon 7 (10 prostheses), surgeon 8 (14 prostheses), surgeon 9 (5 prostheses), surgeon 10 (1 prosthesis), and surgeon 11 (1 prosthesis) – 17 traumatologists as first assistant, and 24 traumatologists as second assistant. The surgical procedure was done under local-regional anaesthesia in 168 patients (64.9%) and under general anaesthesia in the remaining patients.
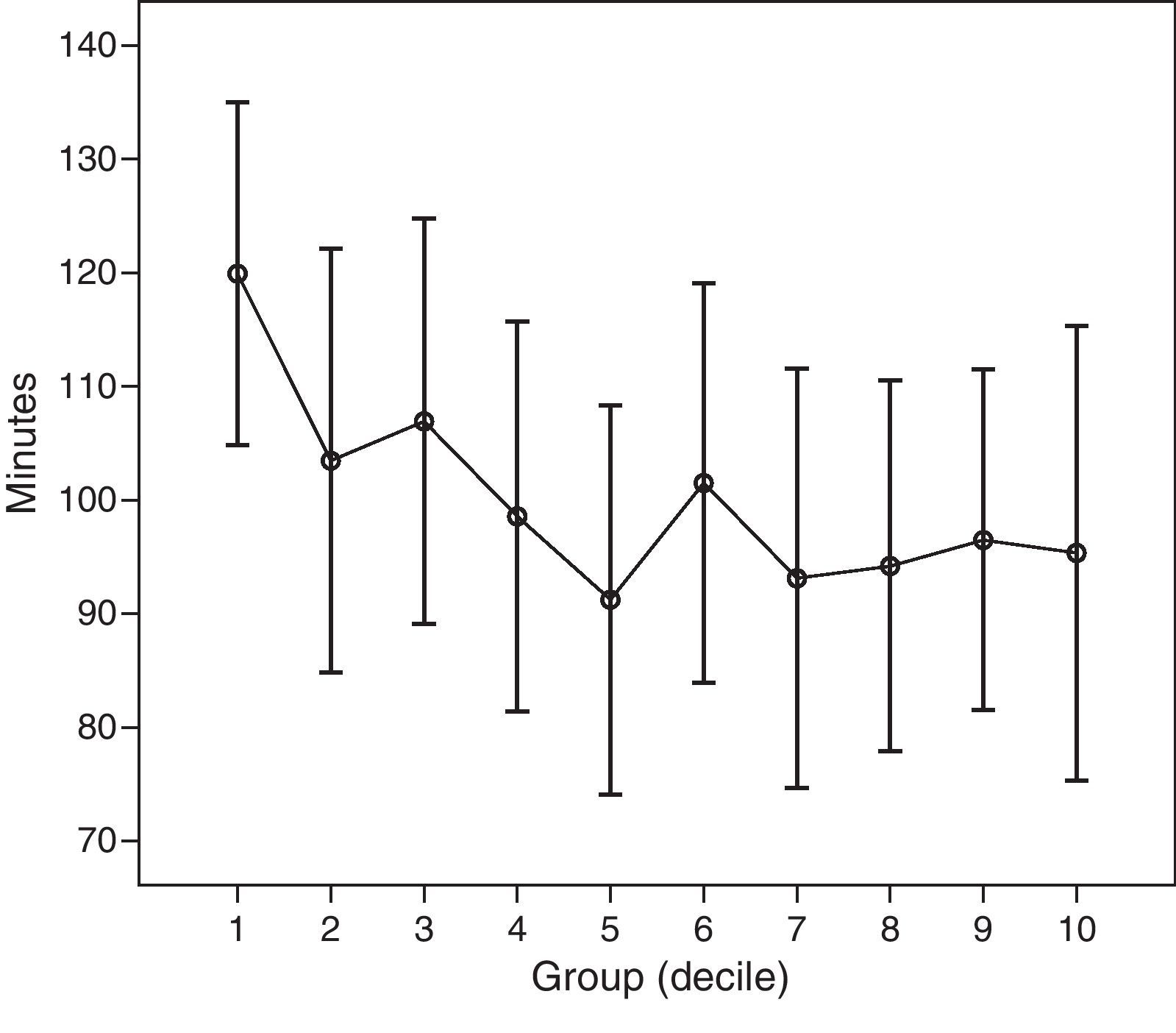
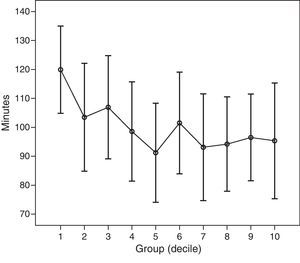
ResultsThe mean incision length, measured with the knee in extension, was 8.56 centimetres (range: 6.5–12.5) (Fig. 1). The mean ischaemia time was 100.11±18.92min (range: 62–135). The mean duration of the procedure was 119.43min. A statistically significant reduction in ischaemia time was found over the course of the 3-year follow-up, the mean ischaemia time decreasing by 28.51min between the first year and the last year. There were no intra-operative complications.
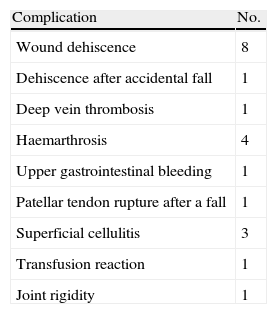
Post-operative dataMean blood loss via drains was 940.04cc (range: 200–2800); these drains were removed 48h after the procedure. The mean decrease between the mean pre-operative haemoglobin and the mean haemoglobin at 24h was 3.62g/dL, this being a statistically significant difference. The mean percentage decrease between the mean pre-operative hematocrit and the hematocrit at 24h was 11.11%, this being a statistically significant difference. There were no differences between surgeons in terms of post-operative blood loss. During the post-operative period, 63.7% (165 patients) required no blood transfusion. The mean degree of knee flexion upon discharge from the hospital was 90.14°±14.76° (range: 35–135°). The mean degree of extension was −2.70°±7.01° (range: 0–15°). Patients were in the hospital for 7±4.5 days, on average (range: 3–42). The most common complication was problems related to the surgical wound (Table 1). No intra-operative complications were perceived, and all the complications recorded occurred during the immediate post-operative period.
The mean femorotibial angle following implantation of the prosthesis was 6.34°±2.5° of valgus (range: 8° of valgus to 1° of varus) (Fig. 2).
The mean HSS score at 6 months after surgery was 85.86±7.79 points, with 258 patients evaluated. At 1 year, 257 were evaluated, with a mean of 88.18±7.39 points.
Learning curveThe 259 patients were grouped into deciles according to when they underwent the procedure, the first 26 prostheses being the first decile and the last 26 prostheses implanted on the Service being the last decile. To attempt to determine the learning curve, the following variables were linked: length of hospital stay, radiographic angles, length of the incision, ischaemia time, complications, post-operative HSS score, post-operative haemoglobin levels, and whether blood transfusion was required (expressed as packed red cells the patient received post-operatively). The different deciles were compared to each other.
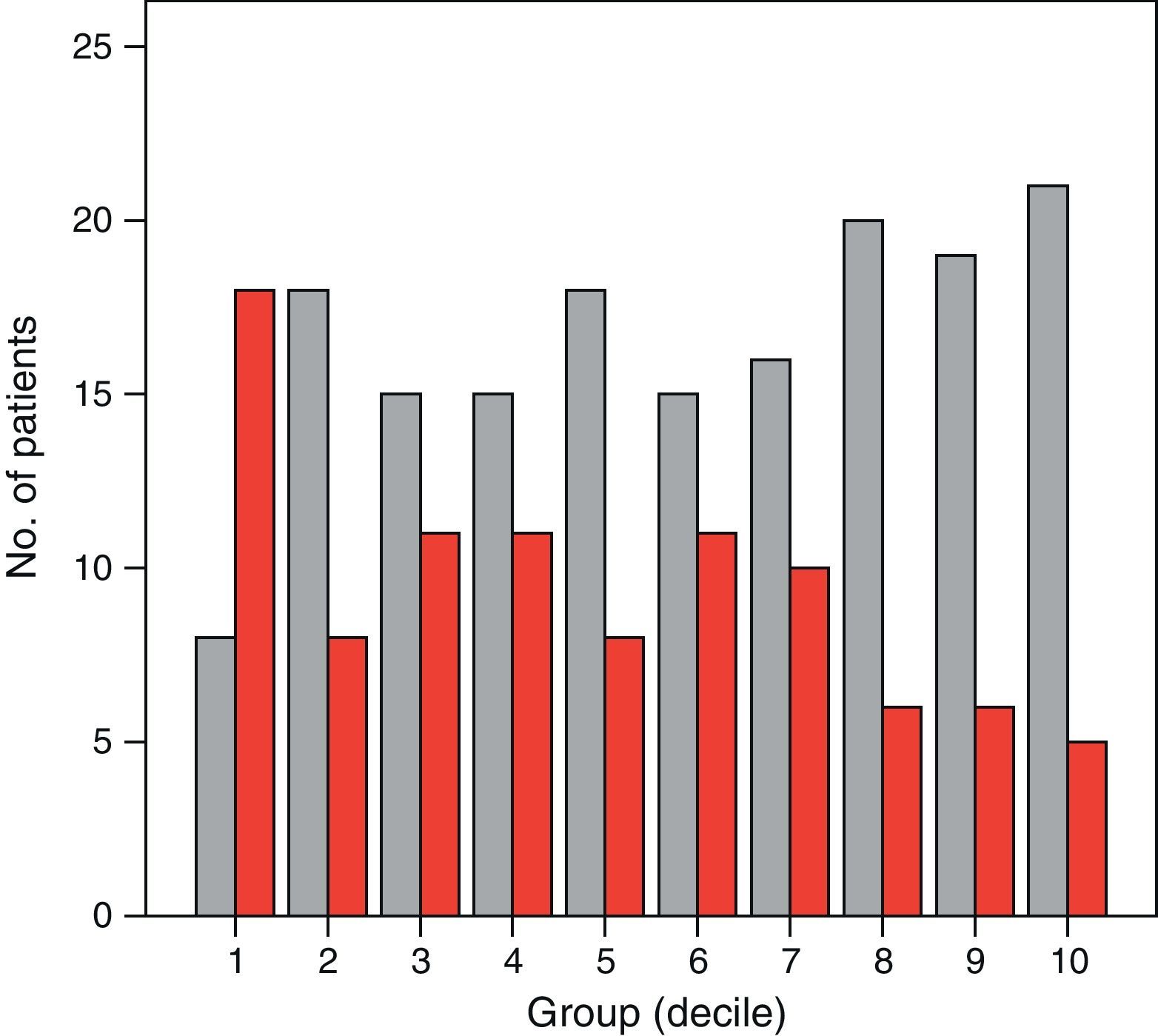
Analysing developments from the first to the last decile, we highlight the following results: the mean length of hospital stay dropped from 7.9 days (5–17) to 6.2 days (4–11), with P=.006. The mean ischaemia time dropped from 120±15min to 95±20min, with P<.001. Packed red cells dropped from a mean of 2 (0–4) units in the first 26 prostheses (18 patients received packed red cells) to a mean of 0 (0–4) units in the last 26 knee prostheses (5 patients received packed red cells, P<.001 (Fig. 3). Analysing the difference between pre-operative haemoglobin level and post-operative haemoglobin at 24h, we found a significant difference between the 2 prosthesis groups—the last group of 26 prostheses experiencing less decrease in haemoglobin.
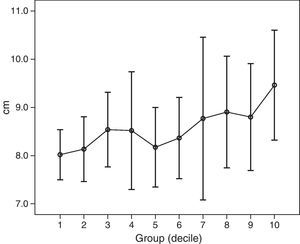
Comparing ischaemia time among the different deciles, no statistically significant differences were found except between the first decile and the rest. Fig. 4 shows the mean ischaemia times for the different deciles. Lastly, there was an increase in mean incision length from 8±0.5cm to 9.5±1.1cm, P<.001 (Fig. 5).
The number of complications dropped from 11.5% to 3.8%, which we consider notable, even though the differences found were not statistically significant due to the small number of complications recorded.
No statistically significant differences were found among patients in the different groups in terms of the HSS score at 6 months and at 1 year after surgery (Fig. 6). We also found no differences among the groups with regard to placement of the prosthetic components (expressed as femorotibial angle), nor were there differences in terms of deformity of the anatomical axis of the knee prior to surgery, as measured on X-ray in the anteroposterior plane—thus, the groups were confirmed to be homogeneous.
DiscussionMIS has been criticized as a technique in arthroplasty of the knee because it is difficult to perform and has a steep learning curve. Although this technique has a number of advantages, such as decreased post-operative pain,11 a shorter hospital stay, less pain, faster functional recovery, and less need of rehabilitation,3,7,10,18,20,23,24 numerous previous studies have shown it to be associated with drawbacks, such as increased surgery time,23,25 greater difficulty placing the prosthetic components,5,26 and a higher incidence of complications.6,27,28 These last factors may be modified by the learning curve.29,30
In reviewing the literature to determine the minimum number of knee replacements that must be performed using minimally invasive techniques before clinical and functional results are achieved that are similar to those for other techniques, the problem we encounter is that most studies report the experience of only 1 surgeon. The objective of our study was to analyse the results that more closely resemble everyday practice in our setting, where total knee replacement is performed by general orthopaedic surgeons.
It is very difficult to determine the minimum number of prostheses required to improve the final results. There are very few studies that consider this parameter. King et al.7 have established 25 knee prostheses as the learning curve for each surgeon. Comparing this surgical technique with the traditional one, they use duration of the procedure, radiographic alignment of the implant, and the patient's clinical results as variables indicating the learning curve for this surgical technique.
In our study, the population sample was divided into deciles (26 knee prostheses per group) in such a way as to confirm that the results for the first decile were different from those for the other 9 deciles. There were no statistically significant differences among the 10 groups in terms of age, sex, previous functional assessment (expressed as the HSS score), or pre-operative radiographic deformities of the femorotibial angle; thus, the groups may be considered homogeneous.
We analysed different variables that could have an effect on learning this technique. Just as in the King study, the following variables were examined: duration of the procedure (expressed as ischaemia time), radiographic placement of the prosthetic components, and functional results (HSS score). Variables related to improved surgical technique and a more experienced surgeon, which could have an effect, were also analysed—these being the mean length of hospital stay, the need for blood transfusion, the length of the skin incision, and the number of complications during and after the procedure.
Thus, between the first decile and the rest, a statistically significant improvement in ischaemia time was confirmed. For Aglietti et al.2 MIS means the procedure is 30min longer, on average, than with a conventional technique, once the learning curve has been overcome, but they do not specify the number of procedures required to reduce the length of the surgery. In another recent project, Lubowitz et al.30 designed a study in which a single surgeon performed 100 knee prostheses using a minimally invasive midvastus approach; they determined that the learning curve was 10 knee prostheses. The major limitation of that study is that reduction in surgery time is the only variable it uses; it does not take into account functional results, complications, or placement of the prosthetic components as indicators of learning. We do not believe that final results are necessarily proportional to surgery time. Another limitation of that study is that homogeneity among the 10 patient groups is based solely on age, sex, and body mass index; it takes into account neither the patient's previous knee deformities and previous functional status nor the aetiology of the osteoarthritis in the knee. In our study, prior to the surgery, all groups were homogeneous in terms of these variables.
Placement of the prosthetic components, expressed as femorotibial angle in the coronal plane on X-ray, was analysed, confirming that placement of the prosthesis was similar in all deciles with no differences found among them. This was also the case with the HSS score, where no differences were found between deciles in terms of post-operative improvement.
The mean hospital stay was longer in the first 26 prostheses group compared to the other 9 groups, this difference being statistically significant. However, we do not consider this variable a good indicator of the learning curve for our setting because, in many instances, the patient's discharge from the hospital depends on not only medical or functional criteria but also other social parameters that result in the hospital stay being prolonged.
Regarding the number of complications, there was a difference between the first group and the last group – 11.5% and 3.8%, respectively – but this difference was not statistically significant. Aglietti et al.2 raise the question of whether all surgeons are able to perform this surgical technique, having determined that complications are being seen with MIS that are no longer an issue with conventional techniques—femoral condyle fracture, patellar tendon rupture, wound-related problems, malpositioning of the prosthetic components, and retained cement debris, among others. Jackson et al.28 designed another prospective study with 209 patients operated on by the same surgeon; they showed that the quad-sparing technique is associated with a higher incidence of intra-operative complications, although the functional and radiographic results were similar to those with a conventional technique. According to the author, once 100 prostheses have been implanted using a quad-sparing approach, these complications are comparable to those seen with a traditional approach. Both studies relate the learning curve to a decreased incidence of complications without taking any other type of variable into account. Kashyap et al.29 find that there is no higher incidence of complications when MIS is used during the learning phase. The scant number of complications seen in our study – similar to that in other series – makes it difficult to determine the minimum number of prostheses to be performed before the incidence of complications is reduced. Although we did not find statistically significant differences between deciles, there is confirmation that the number of complications decreases as the new surgical technique is learned.
Another variable analysed was the need for blood transfusion. To do this, we put forth the hypothesis that proper surgical technique, with a careful incision and reduced surgery time, could mean less blood loss and, consequently, less need for blood transfusion. A statistically significant difference between the first decile and the rest was confirmed, with blood transfusion required more often in the first 26 prostheses. We found no differences among the other 9 groups.
When incision length was analysed, a significant finding surfaced. In contrast to all the variables analysed that decrease or remain the same as experience with the technique is gained, incision length increases proportionally—and it is a statistically significant difference. The reason for this is difficult to explain. It has been proven, as this technique is practiced, that the longer skin incision has no effect on functional results (HSS score) nor on the radiographic prosthetic angle; however, it could reduce the incidence of complications – especially wound-related complications – and the duration of the procedure. These findings are similar to those of Yu et al.14 in their study demonstrating that a longer incision and a 1–2cm invasion of the quadriceps has no effect on functional results, in the short term, and reduces the number of complications.
Lastly, there is a variable that was not taken into account but could also affect some of the variables studied: knowledge of the technique and the instruments on the part of the nursing staff. Knowledge of the instruments could have an effect in reducing surgery time; as stated, however, this is a variable that was not evaluated in this study. For Aglietti et al.2 the surgical team should be well trained, and there should be proper interaction with the assistants to reduce the number of complications during the procedure.
In conclusion, we may state that a general orthopaedic surgeon may perform total knee replacement using MIS techniques with short-term results comparable to conventional surgery and with the advantages of MIS. The variables that improve once the learning curve is overcome are ischaemia time, the need for blood transfusion, and the length of hospital stay, with no effect on final functional results or on the radiographic placement.
Evidence levelEvidence level II.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Jiménez-Cristóbal J, et al. Curva de aprendizaje de la cirugía mínimamente invasiva tipo subvasto limitado en la prótesis total de rodilla. Rev Esp Cir Ortop Traumatol. 2011;55(6):420–427.