Febrile infection-related epilepsy syndrome (FIRES) is a serious epileptic encephalopathy of unknown aetiology, which leads to refractory epileptic status and neuropsychological deterioration. It appears mainly in children and has 3 phases: initial, acute and chronic. In the chronic phase, educational intervention is important to reduce and address exacerbations. Its prevalence is low (1/100,000 children in Europe) which makes it a disease of interest to present as a clinical case with a nursing care plan.
CaseThis is a 16-year-old male patient who debuted at age 7 and has intellectual impairment and abehavioural disorder. Approximately every 21 days he has exacerbations requiring hospitalisation, a situation that we address in this case.
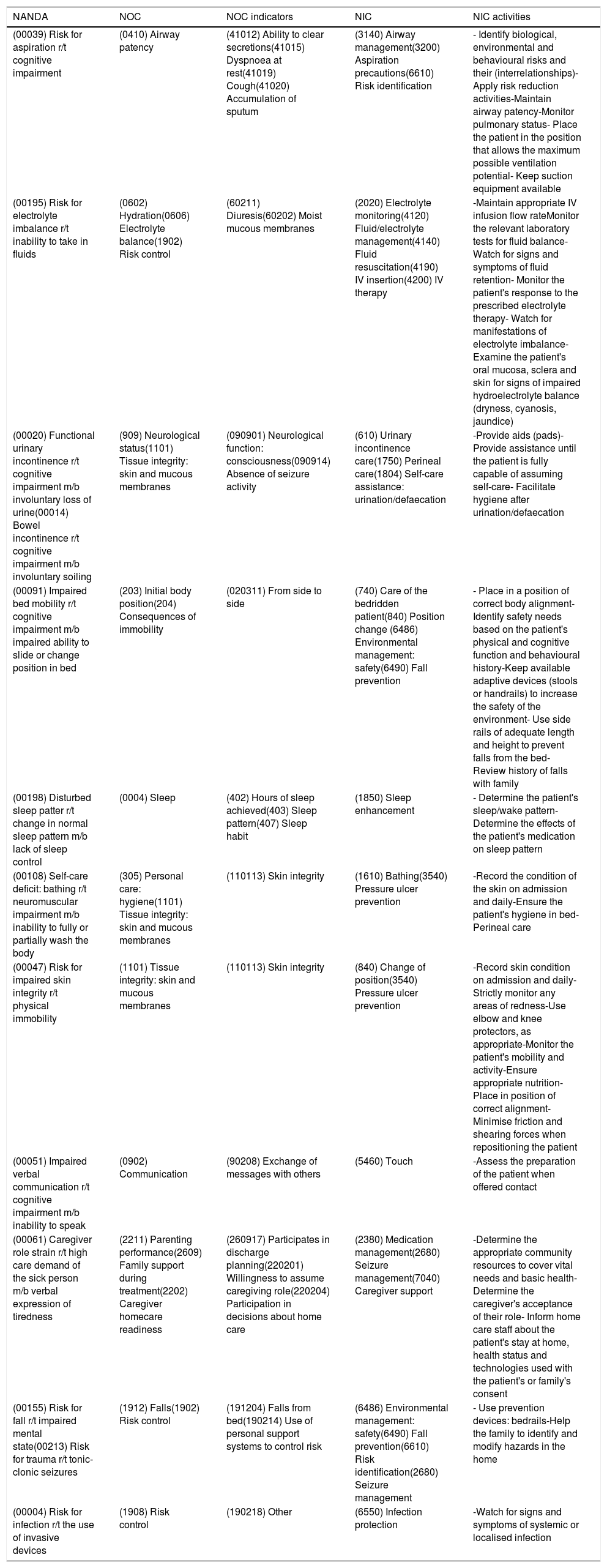
Care plansThe main needs we find are breathing (risk of aspiration), food (risk of electrolyte imbalance), elimination (urinary and faecal incontinence), mobility (deterioration of physical mobility), communication (deterioration of verbal communication) and safety (tiredness of the caregiver's role, risk of falls, risk of infection, risk of deterioration of skin integrity).
ConclusionsIn the acute phase, the need for safety is the most affected, requiring the necessary prevention measures. On the other hand, hospitalisation is a good time to work with the family, optimising the resources provided (home service, ketogenic diet, among others). A multidisciplinary approach is essential for planning and carrying out care.
El síndrome epiléptico relacionado con infección febril (FIRES) es una encefalopatía epiléptica grave de etiología desconocida, que deriva a estatus epiléptico refractario y a un deterioro neuropsicológico. Aparece en niños principalmente y presenta 3 fases: inicial, aguda y crónica. En la fase crónica es importante la intervención educativa para reducir y afrontar las agudizaciones. Su prevalencia es baja (1/100.000 niños en Europa) lo que lo convierte en una enfermedad de interés para presentar en un caso clínico con su plan de cuidados de enfermería.
CasoSe trata de un paciente varón de 16 años que cuya enfermedad se inicia a los 7 años, y presenta un retraso mental y un trastorno del comportamiento. Cada 21 días aproximadamente presenta agudizaciones requiriendo hospitalización, situación que abordamos en este caso.
Plan de cuidadosNos encontramos principalmente alteradas la necesidad de respiración (riesgo de aspiración), alimentación (riesgo de desequilibrio electrolítico), eliminación (incontinencia urinaria y fecal), movilidad (deterioro de la movilidad física, riesgo de deterioro de la integridad cutánea), comunicación (deterioro de la comunicación verbal) y seguridad (cansancio del rol del cuidador, riesgo de caídas, riesgo de infección).
ConclusionesEn la fase aguda, la necesidad de seguridad es la más afectada, requiriendo las medidas de prevención necesarias. Por otro lado, la hospitalización es un buen momento para el trabajo conjunto con la familia, optimizando los recursos proporcionados (servicio a domicilio, dieta cetogénica, entre otros). El abordaje multidisciplinar es indispensable para la planificación y realización de los cuidados.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.