Chronic neuropathic pain treatment is currently one of the biggest challenges for health care professionals because of its high impact on quality of life. Neurostimulation therapy is shown as a widely-accepted treatment for patients who have completed the pharmacological treatment options with no results.
ObjectivesTo show the importance of early detection of post-surgical complication in spinal cord stimulation patients with spinal electrode as well as an adaptation and personalisation of nursing care in the event of post-surgical complications.
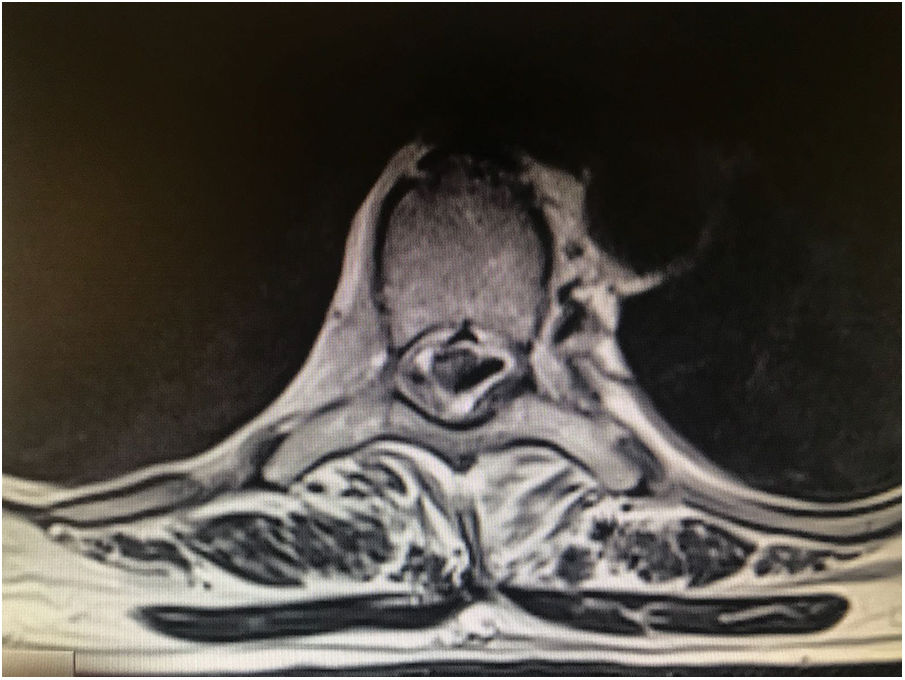
MethodA case of a woman suffering long-term chronic neuropathic pain following a serious traffic accident and subsequent spinal trauma. A study of a number of possible medical options was undertaken to decide the best outcome for the patient; finally, fitting a spinal electrode implant was decided as the best option, in order to start spinal cord stimulation therapy. Post-surgical paraplegia and cerebrospinal fluid leak were detected and incorrect placement of the electrode was observed on magnetic resonance imaging. A re-intervention was carried out for repositioning.
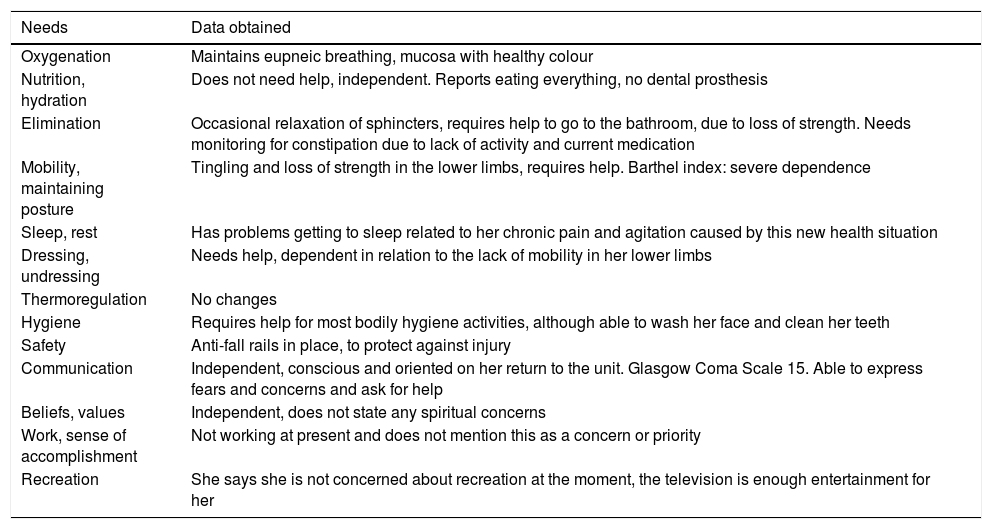
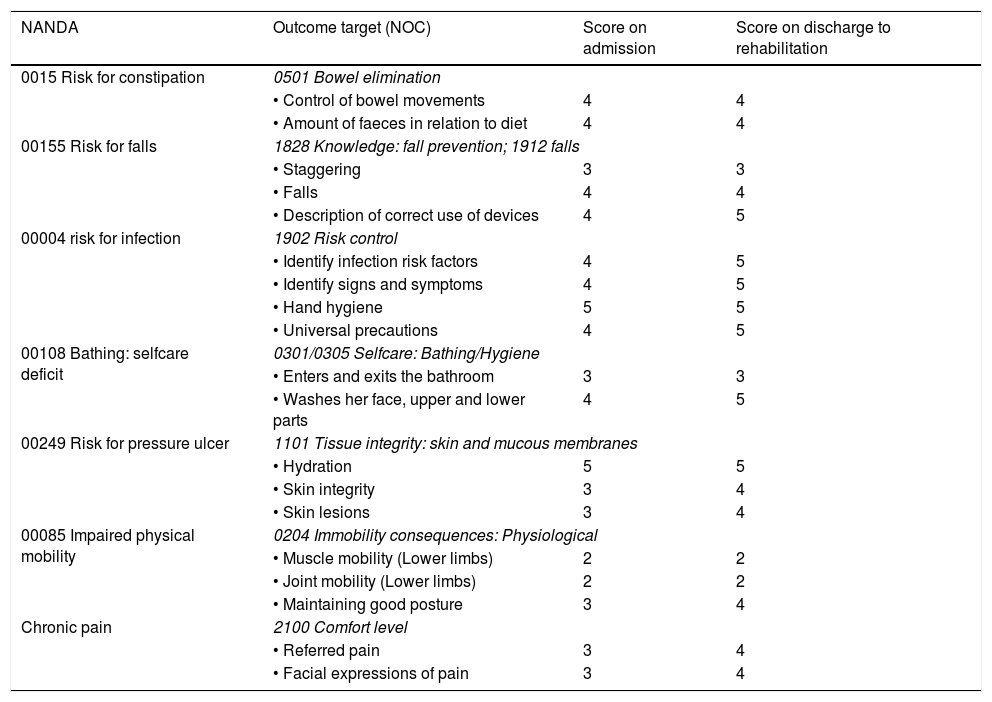
ResultsNursing care of post-surgical complications, the identification of nursing diagnoses and the ideal adaptation of the initial care plan as well as possible activities and objectives are described.
ConclusionsThe importance of the adaptation and personalisation of the nursing care plan for patients with postoperative surgical complications must be highlighted.
El tratamiento del dolor crónico neuropático se encuentra entre uno de los grandes retos para el personal sanitario en la actualidad debido al gran impacto que produce en la calidad de vida de los pacientes. La neuroestimulación profunda se plantea como tratamiento para los pacientes que han agotado las posibilidades de tratamiento farmacológico sin resultados.
ObjetivosMostrar la importancia de la detección temprana de complicaciones posquirúrgicas en pacientes con implantes de electrodo medular, así como de una adaptación y personalización de los cuidados de enfermería en complicaciones posquirúrgicas.
MétodoSe refleja un ejemplo de caso clínico de una mujer con dolor crónico neuropático de larga duración tras traumatismo en accidente de tráfico. Después del estudio de posibles opciones se decide conjuntamente la implantación de un electrodo medular para proceder a la terapia de neuroestimulación profunda. Tras la aparición de paraplejia posquirúrgica y fístula de líquido cefalorraquídeo se detecta una errónea colocación del electrodo y se procede a la realización de una segunda intervención para recolocación.
ResultadosSe describe la actuación de enfermería ante complicaciones posquirúrgicas, identificación de diagnósticos, adaptación del plan de cuidados inicial, así como actividades y objetivos posibles.
ConclusionesResaltar la importancia de la adaptación y de la personalización de los cuidados de enfermería en pacientes con complicaciones posquirúrgicas.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.