Psychosocial adjustment affects the quality of life of patients with Parkinson's disease (PD) and his/her family/carers. However, this is not usually addressed in clinical practice.
ObjectiveTo evaluate coping skills, psychosocial adjustment and quality of life of patients with PD and their family/carers from a quasiexperiment at baseline time.
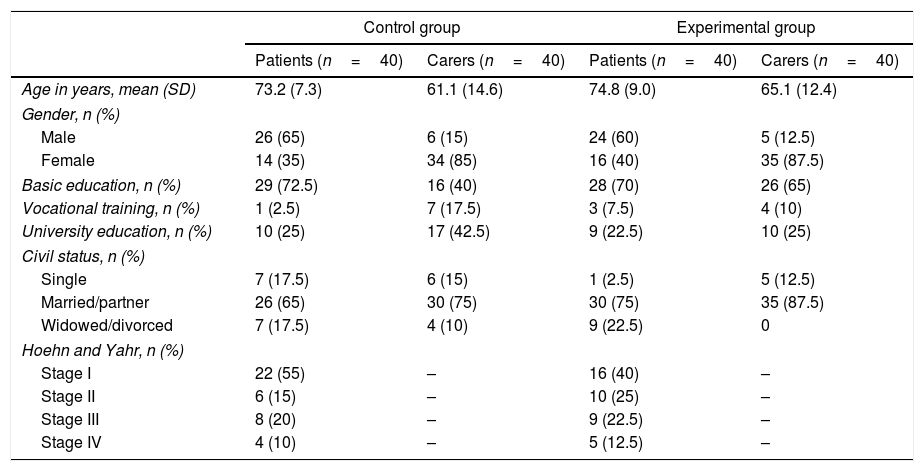
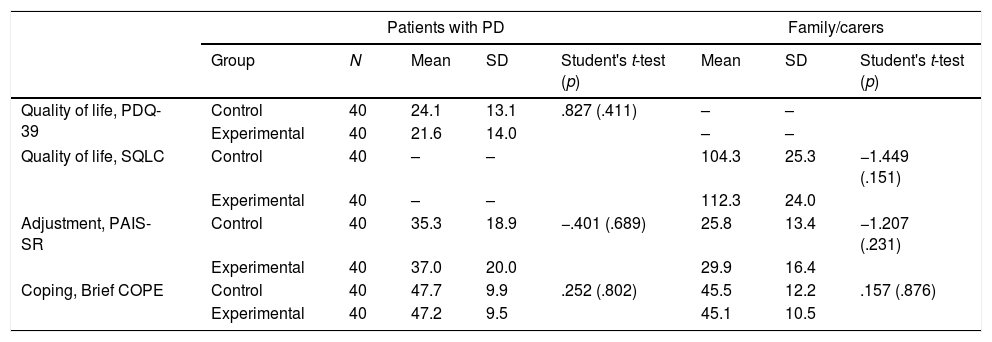
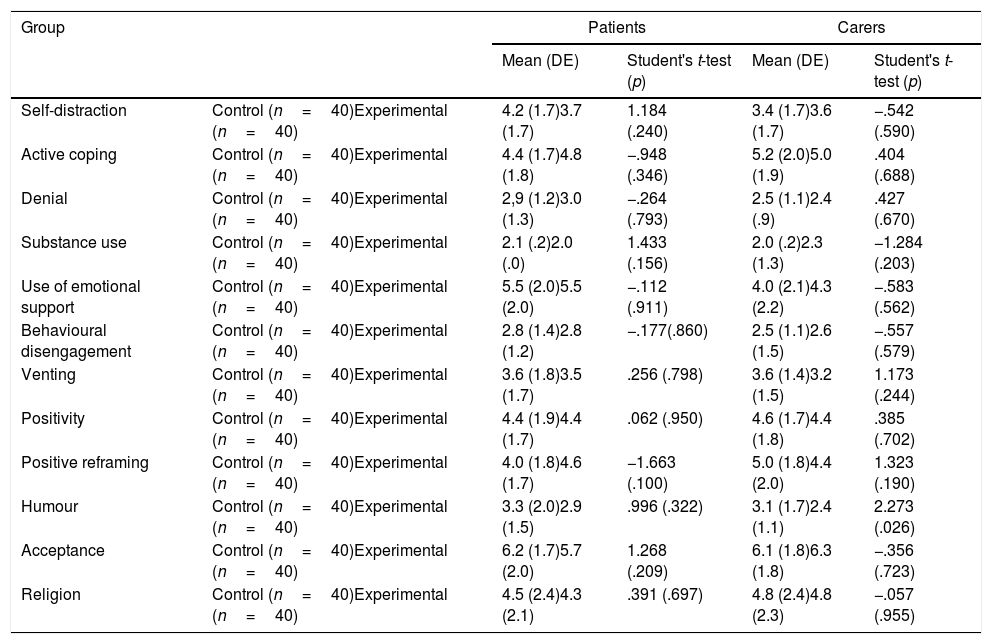
MethodQuasi-experimental study carried out in Primary Care centres to evaluate the impact of a psychoeducational intervention in contrast with an informative intervention. The sample comprised 80 patients with PD and 80 family carers, divided into a control group and an experimental group. The psychosocial adjustment scale PAIS-SR, the coping scale Brief COPE and the quality of life scales PDQ-39 and SQLC were used in the data collection. The analysis of sociodemographic data and Student's t tests was performed using SPSS 23.0.
ResultsThe patients and family/carers from the control group and the experimental group noticed a mild impairment in their quality of life and some difficulties in their psychosocial adjustment to illness. Both groups used coping skills with a medium-low frequency. Acceptance was the most used coping skill by patients and family/carers. No statistically significant differences were found between the control group and the experimental group.
ConclusionsWe observed that the quality of life and psychosocial adjustment to their illness was impacted in patients with PD and their family/carers, which could be addressed with psychoeducational interventions focused on developing their coping skills.
La adaptación psicosocial influye en la calidad de vida del paciente con enfermedad de Parkinson (EP) y de su familiar/cuidador. Sin embargo, desde la práctica clínica generalmente no se aborda.
ObjetivoEvaluar habilidades de afrontamiento, adaptación psicosocial y calidad de vida, en tiempo basal, en pacientes con EP y familiares/cuidadores de un cuasiexperimento.
MétodoEstudio cuasiexperimental realizado en centros de Atención Primaria que evalúa el impacto de una intervención psicoeducativa en comparación con una intervención únicamente informativa. La muestra está constituida por 80 pacientes con EP y 80 familiares/cuidadores, distribuidos en un grupo control y un grupo experimental. En la recogida de datos se emplea la escala de adaptación psicosocial PAIS-SR, la escala de afrontamiento Brief COPE y las escalas de calidad de vida PDQ-39 y SQLC. En el análisis de datos sociodemográficos y t de Student se utiliza SPSS 23.0.
ResultadosLos pacientes y familiares/cuidadores del grupo control y el grupo experimental presentaron una afectación leve de su calidad de vida y algunas dificultades en su adaptación psicosocial. Ambos grupos utilizaban las habilidades de afrontamiento con una frecuencia baja-media. La aceptación fue la habilidad de afrontamiento más utilizada tanto por los pacientes como por sus familiares/cuidadores. No se identificaron diferencias estadísticamente significativas entre el grupo control y el experimental.
ConclusionesEn los pacientes con EP y en sus familiares/cuidadores se observa un impacto a nivel de la calidad de vida y la adaptación a la enfermedad, que podría ser abordado con intervenciones psicoeducativas centradas en desarrollar su capacidad de afrontamiento.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.