In 1890 four cases of headache associated with visual symptoms and hysterical disorder were described by the French neurologist Babinski as migraine ophthalmique hystérique, or hysterical ophthalmic migraine. Since that time this association has seldom been described, and the possibly high frequency previously reported still remains to be established. This paper has reused Babinski's description and it tries to rehabilitate the syndrome described by the French semiologist across the relatively frequent experience of this type of patients in a public hospital. Also it analyzes the reason of the oblivion of his description.
MethodThis study presents a series of 43 cases of headache of the migraine type associated with other symptoms, most consistent with basilar-type migraine according to IHS criteria. Diagnosis of conversion disorder (hysteria) was grounded in the criteria set forth in the DSM-IV.
ResultsAll patients exhibited one or more manifestations of hysteria (conversion symptoms) during migraine attacks, and some did in the intervals between attacks as well. Details of the headaches, associated symptoms, and hysterical manifestations are discussed. Most patients improved with antimigraine medication. Altered consciousness may have contributed to the onset of hysterical symptoms.
ConclusionsThe basilar type migraine associated with conversion symptoms described of systematized form by Babinski, it is not a rare entity. Similar pictures have been described along the history of the medicine. The later silence possibly is due to the historical difficulty in defining accurately the conversión disorders. The Babinski's migraine is a certain well entity and must be recovered for the clinic.
En 1890 el neurólogo francés Babinski describió como migraine ophthalmique hystérique o jaqueca oftálmica histérica, cuatro casos de cefalea asociada a síntomas visuales y trastornos histéricos. Desde entonces esta asociación ha sido raramente descrita, aunque la frecuencia, posiblemente elevada de acuerdo con descripciones anteriores, está por establecer.
Este trabajo recupera la descripción de Babinski e intenta rehabilitar el síndrome descubierto por el semiólogo francés en la relativamente alta frecuencia de este tipo de pacientes observada en un hospital público. Asimismo, se especula sobre los motivos del olvido de esta descripción.
MétodoEl estudio presenta una serie de 43 casos de jaqueca, la gran mayoría compatibles con jaqueca de tipo basilar de acuerdo con los criterios IHS, asociados a síntomas de conversión. El diagnóstico de trastorno de conversión (histeria) se basa en los criterios establecidos por el DSM-IV.
ResultadosTodos los pacientes mostraron una o más manifestaciones de histeria durante las crisis de jaqueca, y algunos en los intervalos. Se discuten los detalles de las cefaleas, de los síntomas asociados y de las manifestaciones histéricas. La mayoría de los pacientes mejoró con medicación antijaquecosa. La alteración de la conciencia pudo haber contribuido al desencadenamiento de los síntomas histéricos.
ConclusionesLa jaqueca basilar asociada a trastorno de conversión descrita de forma sistematizada por Babinski no es una entidad rara. Cuadros similares se han descrito a lo largo de la historia de la medicina. El silencio durante el último siglo sobre la entidad se debe posiblemente a la dificultad histórica en definir de forma apropiada los trastornos de conversión. La jaqueca de Babinski es una entidad bien establecida y debe ser recuperada para el clínico.
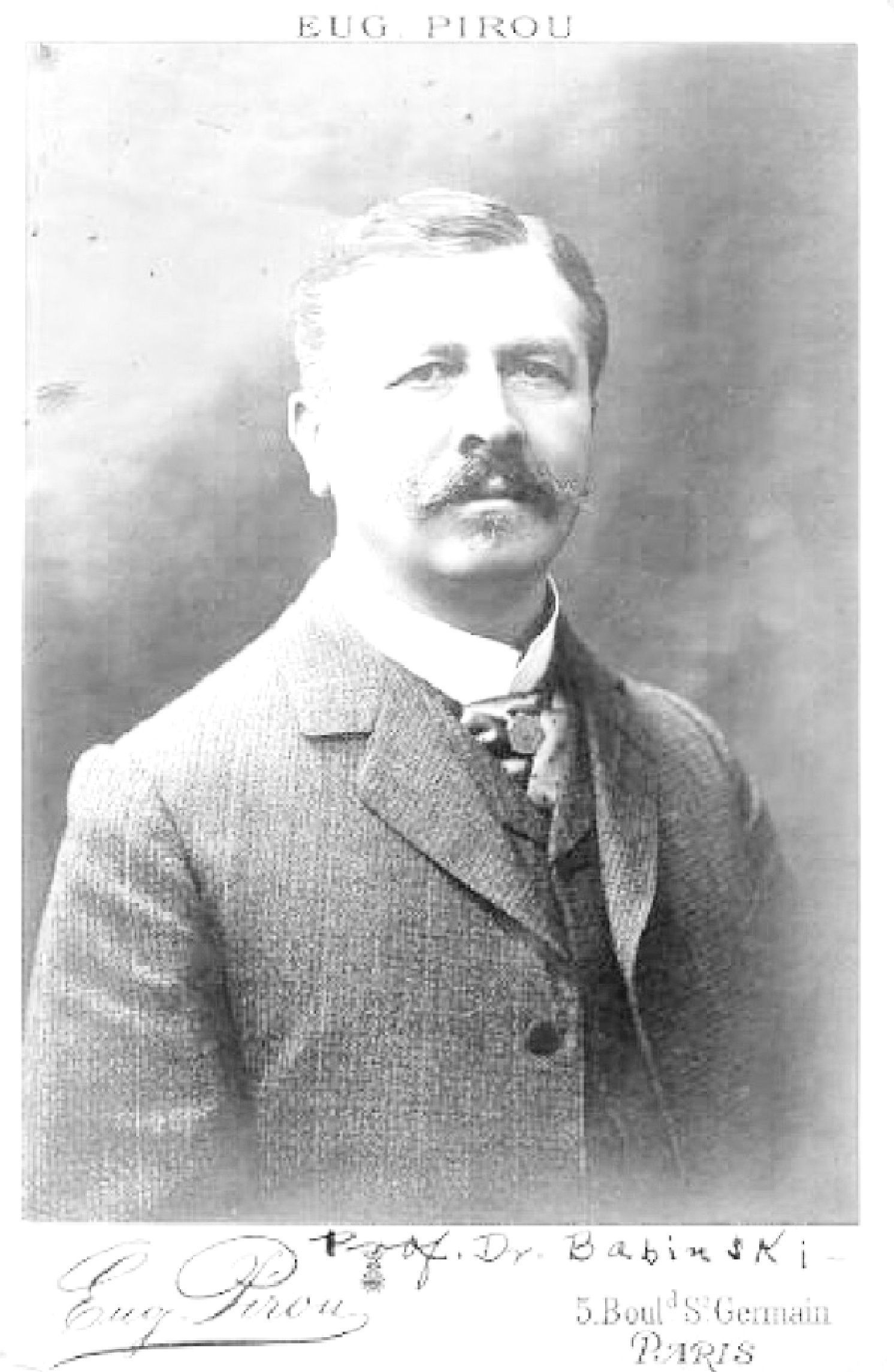
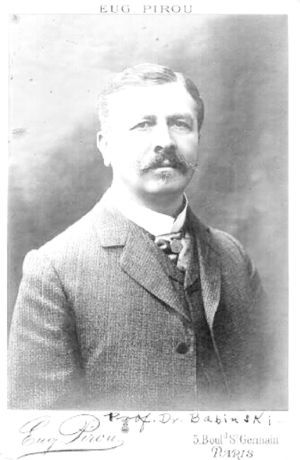
The appearance of psychiatric alterations during episodes of headache is not uncommon and was described as “mental migraine”1 or hemicrania dysphrenica by Mingazzini in 1893.2 The association between conversion symptoms and migraine attacks, however, seems to be infrequent. The great French semiologist Joseph François Felix Babinski (1852–1932) (Fig. 1) was the first to describe, in 1890, a series of 4 patients suffering from migraine with visual aura that was associated with hysterical symptoms, which he called migraine ophthalmique hystérique.3 Oddly, this association has only been cited in passing in isolated cases since then. Hypothesizing that this association is relatively common and that Babinski's migraine should be revived as an entity and the syndrome re-established, a protocol intended to compile full clinical details was applied to a series of 43 cases consistent with the 2004 International Headache Society (IHS) criteria for migraine,4 mostly basilar-type migraine (BM), that also exhibited conversion disorders (abnormal movements, pseudo-epileptic fits or motor, sensation or sensory deficits) according to the criteria of DSM-IV.
MethodsA total of 43 patients with symptoms consistent with migraine and conversion disorder seen at the Headache Unit of our hospital's Neurology Department between 1998 and 2009 were included. This unit specialises in headache and accepts only those patients meeting 1 of 3 criteria: (1) refractory headache; (2) clinically singular cases; (3) participants in clinical tests or research. The Headache Unit saw a total of 2030 new patients over the period considered. Of these, 1650 were migraine patients, with 140 suffering from basilar-type migraine (BM) and probable BM. Over the same period, the Neurology Department's general neurology units saw 29270 new ambulatory patients.
The hospital is part of a public tertiary care teaching hospital (Hospital Universitario Príncipe de Asturias in Alcalá de Henares, Madrid, Spain) serving a population of 398000 inhabitants. Case referral source was quite variable, mostly from the general neurology units and specialised epilepsy units (for assessing “pseudo-seizures”), with only 3 patients referred by the psychiatry unit. Six patients were sent by the Meco Penitentiary for evaluation of seizures and headache. Eight were immigrants (from Latin America, Romania, and Poland). The immigrant population makes up less than 10% of the population in the area served by our hospital.
The study was retrospective for the first 12 cases (presented at the 55th Annual Meeting of the Spanish Society of Neurology in Barcelona, 2003)5 and prospective for the remaining 31 patients. Patients were evaluated by at least 2 experienced neurologists (1 always the same) and a psychiatrist. The protocol employed included a general clinical, neurological and psychiatric history, and a general, neurological and psychiatric examination. There was also at least 1 surface electroencephalogram (EEG) with electrode placement according to the International 10–20 System. A cranial CT scan and a video-EEG were performed for all patients. Complementary magnetic resonance (MR), positron emission tomography (PET) using fluorodeoxyglucose as radiotracer, or single-photon emission computed tomography (SPECT) with an isotope of technetium were also carried out for certain patients.
Inclusion criteria were for patients with evidence of migraine, conversion symptoms during the headache episode and no known organic cause. Three patients with episodic headache and conversion symptoms separate from the episodes were excluded.
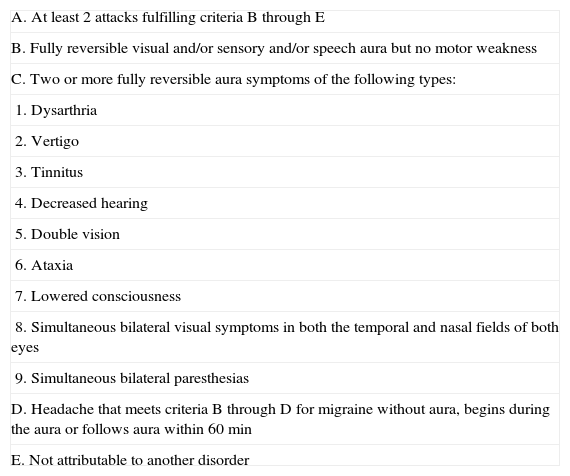
Diagnosis of migraine or basilar-type migraine was based on the criteria of the recent IHS International Classification of Headache Disorders (Table 1).4
Criteria for basilar-type migraine.
| A. At least 2 attacks fulfilling criteria B through E |
| B. Fully reversible visual and/or sensory and/or speech aura but no motor weakness |
| C. Two or more fully reversible aura symptoms of the following types: |
| 1. Dysarthria |
| 2. Vertigo |
| 3. Tinnitus |
| 4. Decreased hearing |
| 5. Double vision |
| 6. Ataxia |
| 7. Lowered consciousness |
| 8. Simultaneous bilateral visual symptoms in both the temporal and nasal fields of both eyes |
| 9. Simultaneous bilateral paresthesias |
| D. Headache that meets criteria B through D for migraine without aura, begins during the aura or follows aura within 60min |
| E. Not attributable to another disorder |
Diagnosis of conversion disorder (hysteria) followed the criteria set forth in the Spanish version of the Diagnostic and Statistical Manual of Mental Disorders: DSM-IV (American Psychiatric Association, 1995), Criterion F44.x (300.11).6 Diagnosis was based on inconsistencies in the clinical history, the absence of exploratory signs indicative of an organic lesion that would account for the conversion manifestations, and inconclusiveness of the findings of ancillary tests. The following additional factors were also taken into account to refine the diagnosis of conversion disorder:
- (1)
Manifestations suggestive of hysteria such as preserved consciousness during seizures, arc hystérique (opisthotonos), linkage to emotional stimuli or complete recovery.
- (2)
Presence of positive signs for hysteria7 during episodes or where sustained neurological deficit was identified (Hoover's test, sternocleidomastoid test, midline splitting, splitting of vibration test and others).
- (3)
Fulfilment of various published inventories for specific conversion disorders, such as psychogenic gait,8 psychogenic seizures9,10 or psychogenic abnormal movements.11,12
- (4)
Suggestion (hypnosis) able to bring on episodes.
Thirty-two patients underwent suggestion (hypnosis) to try to elicit an episode for evaluation. The method employed was always the same and was carried out by the same person. It comprised:
- (1)
Informed consent. A family member who was able to compare the episodes that had caused the patient to seek medical help with the episode triggered by suggestion was in attendance.
- (2)
The patient was told that he or she would have an attack during the test.
- (3)
In a relaxed setting the patient was asked to concentrate deeply while the glabella was softly tapped with a reflex hammer. An episode ordinarily occurred after 5–10min.
- (4)
Suggestion and pressing on the glabella with the thumb were used in an effort to abort the attack.
Episodes were brought on by suggestion in 14 patients, who were monitored by video-EEG recording at the time.
ResultsA diagnosis of migraine associated with conversion symptoms was made in 43 patients. There were 33 women and 10 men (a female:male ratio of 3.3:1). Mean age at initial patient presentation was 36 years, although there were 3 adolescents (14, 16 and 17 years of age) and two retirees who were 68 and 75 years old. However, the mean age at headache onset was 20 years of age (14 patients experienced onset as teenagers and 6 as children).
A total of 33 patients from the same source population with conversion symptoms using the same diagnostic criteria but without headache were seen by the Neurology Department during the same period (9 years). Consequently, in our specific context, migraine sufferers made up a majority (56%) of all patients with conversion symptoms (76 hysteric patients).
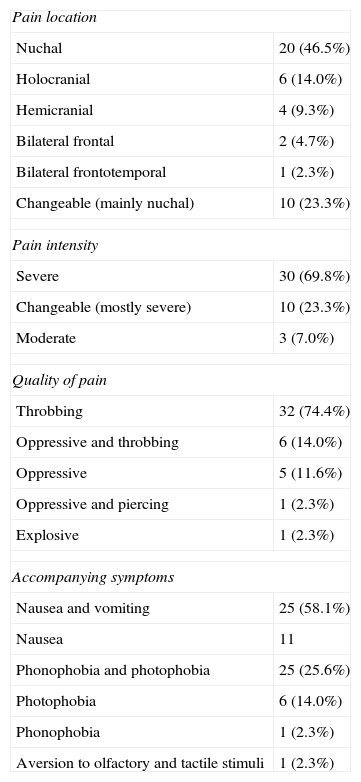
MigraineTable 2 sets out the headache data. All patients suffered from similar recurring (more than 5 attacks) episodes of migraine headache. These were, however, variable in terms of frequency, pain severity and the presence of associated symptoms.
Headache characteristics (n=43).
| Pain location | |
| Nuchal | 20 (46.5%) |
| Holocranial | 6 (14.0%) |
| Hemicranial | 4 (9.3%) |
| Bilateral frontal | 2 (4.7%) |
| Bilateral frontotemporal | 1 (2.3%) |
| Changeable (mainly nuchal) | 10 (23.3%) |
| Pain intensity | |
| Severe | 30 (69.8%) |
| Changeable (mostly severe) | 10 (23.3%) |
| Moderate | 3 (7.0%) |
| Quality of pain | |
| Throbbing | 32 (74.4%) |
| Oppressive and throbbing | 6 (14.0%) |
| Oppressive | 5 (11.6%) |
| Oppressive and piercing | 1 (2.3%) |
| Explosive | 1 (2.3%) |
| Accompanying symptoms | |
| Nausea and vomiting | 25 (58.1%) |
| Nausea | 11 |
| Phonophobia and photophobia | 25 (25.6%) |
| Photophobia | 6 (14.0%) |
| Phonophobia | 1 (2.3%) |
| Aversion to olfactory and tactile stimuli | 1 (2.3%) |
Headache location was well defined in most of the cases. The pain was exclusively nuchal in 20 patients, holocranial in 6, hemicranial in 4, bilateral frontal in 1, bilateral frontal–parietal in 1 and bilateral frontal–temporal in 1. In the remaining 10 patients, the pain shifted position depending on intensity, being nuchal in most cases when episodes were extremely severe.
Pain varied in intensity with each episode but was described as extremely severe and incapacitating by 30 patients. Pain was throbbing in 32 cases and oppressive, piercing or explosive in the rest.
During the attacks, 36 patients were nauseated and 16 experienced vomiting. Vomiting was particularly intense in 11 cases. Phono/photophobia was present in 30 cases, 6 patients had photophobia only, 1 phonophobia only and 1 had aversion to olfactory and tactile stimuli.
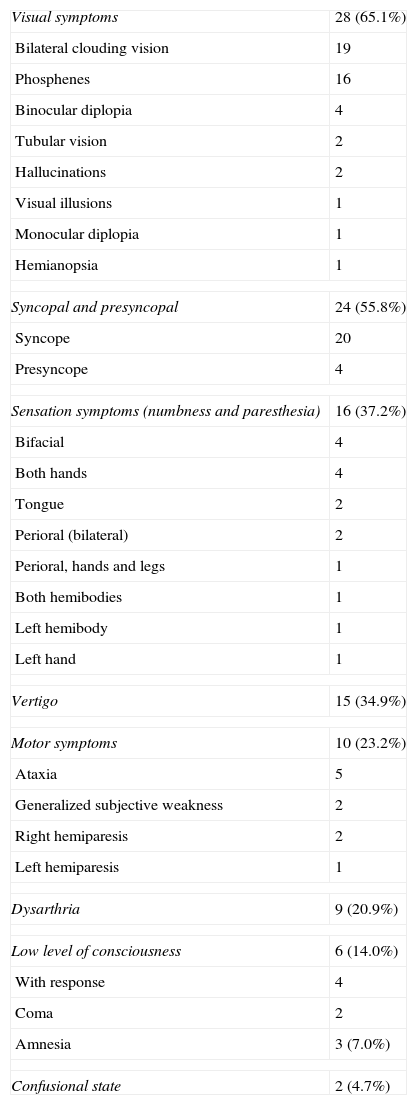
In 38 patients headache met the criteria for BM. Table 3 summarises the symptoms of basilar-type dysfunction. There were no cases of elementary visual hallucinations suggesting occipital epilepsy (brightly coloured, multiple, circular spots).13 Only a single, fully reversible symptom suggestive of involvement of the basilar territory was identified in 4 cases (vertigo in 2, bilateral hemifield visual blurring and phosphenes in 2), whereas conventional IHS criteria require 2 or more symptoms. Three cases exhibited hemiparesis in addition to basilar-type symptoms. Accordingly, there were 38 cases of BM and 5 cases of “probable” BM.
Basilar-type manifestations (n=43).
| Visual symptoms | 28 (65.1%) |
| Bilateral clouding vision | 19 |
| Phosphenes | 16 |
| Binocular diplopia | 4 |
| Tubular vision | 2 |
| Hallucinations | 2 |
| Visual illusions | 1 |
| Monocular diplopia | 1 |
| Hemianopsia | 1 |
| Syncopal and presyncopal | 24 (55.8%) |
| Syncope | 20 |
| Presyncope | 4 |
| Sensation symptoms (numbness and paresthesia) | 16 (37.2%) |
| Bifacial | 4 |
| Both hands | 4 |
| Tongue | 2 |
| Perioral (bilateral) | 2 |
| Perioral, hands and legs | 1 |
| Both hemibodies | 1 |
| Left hemibody | 1 |
| Left hand | 1 |
| Vertigo | 15 (34.9%) |
| Motor symptoms | 10 (23.2%) |
| Ataxia | 5 |
| Generalized subjective weakness | 2 |
| Right hemiparesis | 2 |
| Left hemiparesis | 1 |
| Dysarthria | 9 (20.9%) |
| Low level of consciousness | 6 (14.0%) |
| With response | 4 |
| Coma | 2 |
| Amnesia | 3 (7.0%) |
| Confusional state | 2 (4.7%) |
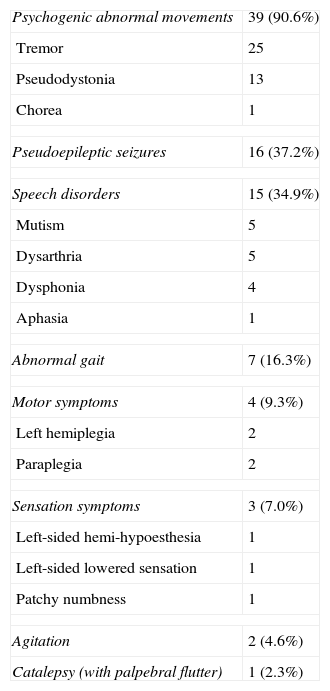
Table 4 summarises the conversion symptoms. The complex hysterical symptoms have been arranged on the basis of similarity to the “organic” symptoms they resemble. Most patients exhibited several of the symptoms set out in this table either serially or combined (for instance, progressive shaking, aphonia and pseudodystonic spasms with subsequent collapse onto the floor mimicking an epileptic fit).
Conversion symptoms (n=43).
| Psychogenic abnormal movements | 39 (90.6%) |
| Tremor | 25 |
| Pseudodystonia | 13 |
| Chorea | 1 |
| Pseudoepileptic seizures | 16 (37.2%) |
| Speech disorders | 15 (34.9%) |
| Mutism | 5 |
| Dysarthria | 5 |
| Dysphonia | 4 |
| Aphasia | 1 |
| Abnormal gait | 7 (16.3%) |
| Motor symptoms | 4 (9.3%) |
| Left hemiplegia | 2 |
| Paraplegia | 2 |
| Sensation symptoms | 3 (7.0%) |
| Left-sided hemi-hypoesthesia | 1 |
| Left-sided lowered sensation | 1 |
| Patchy numbness | 1 |
| Agitation | 2 (4.6%) |
| Catalepsy (with palpebral flutter) | 1 (2.3%) |
Shaking was the most common symptom (58.1% of patients) and was ordinarily associated with other symptoms. Shaking was usually paroxysmal, with sudden onset and variable and bizarre morphology (e.g., shaking of the head or trunk in some cases). It had a fluctuating rhythm (generally less than 8Hz) and oscillating amplitude, sometimes in the form of great, violent shudders. Tremor was often preceded by small, isolated myoclonic-like contractions that increased in amplitude and frequency, gradually becoming rhythmic or pseudorhythmic and ultimately convulsion-like in appearance. Patients exhibited resting, intention and postural tremor that on occasion tended to diminish when the observer was not paying attention to the symptom or when the patient's attention was shifted to other targets.
Pseudodystonia took the form of repeated spasms (similar to tremor or periodic myoclonus) and abnormal postures. Most were also paroxysmal, fluctuating and bizarre, not at all comparable to more stereotypical dystonic spasms such as torticollis or oromandibular dystonia. The spasms often developed into abnormal postures or violent shaking wrongly interpreted as epileptic fits. Spasms could start in 1 limb and propagate to other regions, including the spinal and abdominal muscles. Episodes tended to be transitory and reversible, lasting 30–60min. In 6 cases the body took on the typical posture of opisthotonos (arc hystérique) during the episode.
Conversion chorea was present in 1 case with continuous and irregular movements during the headache episode. These movements could be induced or aborted by suggestion.
Sixteen patients were diagnosed as having pseudoepileptic fits. Six had initially been diagnosed and treated as suffering from epileptic fits. Fainting, common in these patients, was not included in this rather indefinite category, although we did include many of the psychogenic abnormal movements – tremor, pseudodystonia – mentioned above. With variations, most of the patients fit in part the classic descriptions like Charcot's grand mal hystérique,14 but the different stages of the fit were not well defined in most cases. Fit sequence, duration and content were highly variable but constant in each patient. Greater or lesser episode intensity was all that varied in each patient, with the manifestations being much milder (tremor, isolated convulsions) and shorter in duration in some episodes and longer lasting, ending in violent shaking, in others. Despite the bizarre, violent nature of the episodes, recovery was rapid and complete in most cases.
The speech disorders comprised inability to speak in 5 patients, with normal comprehension and vocalisation during coughing and normal mouth, tongue and face movements and proper gesturing. Five patients also exhibited dysarthria with non-systematic stuttering. On the whole, this speech impediment was readily distinguishable from the more systematic disorder attributable to brainstem dysfunction. Dysphonia or aphonia ceased when the coughing stopped and, in 1 case, during sleep-talking at night.
One case was associated with semantic paraphasias and nonsense responses as in Ganser syndrome.
Abnormal gait was the most striking manifestation in 7 patients. This was attributed to hemiplegia (Todd's paresis) in 2 cases and to irregular, hysterical or unclassifiable ataxia in the rest.
Two patients had left-sided hemiplegia for 2–3 weeks after the headache and 2 patients had recurrent paraplegia. All these cases were influenced by suggestion and the paralysis disappeared or was significantly reduced during sleep movements, when the patient's attention was shifted to other targets, or during automatic activities like dressing.
One patient had painful, lowered sensitivity to tactile stimuli and another, “total” hemibody numbness. In both cases the exact boundary at the midline was indicative that it was conversive in nature. One patient complained of patchily distributed regions of numbness.
In 2 cases, the attacks ended in shouting, crying and severe agitation.
After headache 1 patient manifested a recurring cataleptic state but with normal examination findings, palpebral flutter and recovery in 24–48h.
Two women with a long history of neurological and extraneurological somatisation disorders were diagnosed as having Briquet syndrome.
Temporal profileAround half (23 patients) suffered from different types of headache. The most frequent was migraine without aura (MWA), another type was probable or definite BM, and the least frequent was basilar-type migraine with associated conversion symptoms (BMCS), the focus of this study. Ten patients complained of occasional (6 patients) or frequent (4 patients) tension-type headache in the intervals between migraine episodes.
Ten patients had MWA and much less frequent BMCS. In 5 patients the conversion episodes occurred with basilar-type migraine but also without headache.
The sequence of symptoms (for instance, headache, basilar symptoms like vertigo and hysterical manifestations like “grand mal hystérique,” to cite an example) was variable among the patients but constant in any one individual patient. In 21 cases the basilar symptoms preceded onset of the hysterical manifestations but then both occurred concurrently during the course of the headache. In 7 cases the basilar symptoms preceded headache and hysterical manifestations occurred during the headache. In 6 cases (all with tremor and pseudodystonia) hysterical and basilar symptoms were simultaneous, preceding the headache. The sequence could not be definitely established in 4 cases. Thus, headache was an ictal, pre-ictal or post-ictal symptom.
Duration of symptoms was also variable, even within individual patients. BMCS headache duration was mostly 6–24h (20 patients), but the headache lasted for 48h in 8 cases, for 72h in 6 cases and for 7 days in 1 case. Duration was variable in the remaining cases (8 patients). Basilar symptoms lasted 15–30min, although vertigo sometimes continued for 12–24h. Conversion symptoms lasted 15–60min, but 24–48h in 4 cases and up to 15 days in another 4 cases. Clinical manifestations of hysteria became chronic in 5 cases. In 2 cases the symptom (dysarthria in 1, paraplegia in the other) continued for months. In 2 patients with hysterical hemiplegia and 1 patient with tremor, the symptom manifested for 3, 6 and 7 years, respectively, while BM persisted.
Episode frequency was highly variable. However, it tended to be low and to occur in clusters or to be directly related to emotional stimuli or periods of stress.
Stress (or post-stress) or emotional impact was clear triggering factors for MWA, BM and BMCS in 30 patients. However, no psychogenic factor was identifiable in 7 patients and episodes took place both with and without any recognisable stress factors in 6 patients. In 2 patients BMCS episodes were sometimes brought on by menstruation.
Family historiesCorrect family histories could be compiled for only 30 patients. Of these, 16 cases had more than 1 first-degree relative with histories of headache (MWA, BM). Family histories of BMCS were found for only 2 patients with BMCS.
SuggestionSuggestion was used to try to set off a hysterical episode in 32 patients for diagnostic purposes or possible influence on clinical symptoms. Symptoms similar to the clinical symptoms were reproduced in 22 patients. Conversion symptoms were triggered in 14 patients who underwent video-EEG monitoring without alterations in the EEG.
Psychiatric comorbidityPsychiatric comorbidity took the form principally of anxiety of greater or lesser severity in 20 patients and anxiety-depression disorder in 11 patients. Psychiatric status could not be determined in 5 patients. Seven patients appeared to be emotionally and psychiatrically normal.
Histrionic personality disorder, with its emotional excesses, theatrics and somatisation disorders, could be confirmed in only 8 patients. “Migraine personality” (i.e., inflexible, perfectionist, ambitious and obsessive) was observable in only 2 cases.
The notion of “gain from illness” is held by certain schools to be at the core of hysteria, but it is agreed to be hard to study, and there is no comparative model that can be employed. Even so, an attempt was made to examine this aspect in 20 patients, with a clear gain observable in only 5. This proportion was deemed comparable to the incidence of attempted gain by patients with non-hysterical illnesses.
For similar reasons, the results regarding la belle indifference in our patients could not be assessed. Subjectively, this attitude towards their own symptoms on the part of the patients was held not to be more frequent than in patients with multiple sclerosis.
Outside the attacks, the neurological examinations were normal or inconsequential in all the patients except for the 3 cases of hemibody motor or sensory deficits. Twenty patients (17 women, 3 men) exhibited slight hypotonia with hyperpassivity and joint hyperextensibility with slight hyperkinesia (“womanly” muscle tone), but they fell within the normal range. In the patients with chronic conversion symptoms, special attention was paid to positive signs of hysteria, which were observable in all these patients.
Ancillary examinationsThe imaging (CT) test results were normal or exhibited inconsequential findings that did not account for the clinical symptoms (for instance, 2 cases of stable arachnoid cyst in the right temporal pole). The MRI findings were normal or likewise inconsequential in the 18 patients in whom this scan was performed. In addition to MRI scans, SPECT scans were also performed in the 5 cases in which the disorder had become chronic, and PET scans were performed in the 2 cases with hemiplegia; the results were normal in all cases. The EEG results were consistently normal in all the patients and inconclusive in 5, including those in which readings were taken during hypnosis (14 cases), in the 12 patients who underwent 2 EEGs and in the other 12 patients who underwent 3 EEGs. Rapid traces were recorded in only 6 patients and were attributable to their courses of medication. In particular, neither spontaneous occipital seizures nor photically induced or epileptic discharges were recorded in any patients.
TreatmentThe first step was to carefully withdraw the medication patients were taking when they first came to the Headache Unit, mostly overmedication with antiepileptics. Treatment was basically designed to prevent migraine attacks where advisable because of the high frequency or severity of episodes and to address the psychiatric comorbidity when it was a prominent symptom. Twenty-five patients were treated with propranolol (9 patients with propranolol alone, 14 patients with propranolol, amitriptyline, and medazepam, 1 young patient with propranolol and sodium valproate, and 1 patient with propranolol and oxcarbamazepine). Propranolol was taken 2–3 times a day, for a total dose of 40–120mg/d, depending on the response. The dose of amitriptyline ranged from 12.5 to 25mg/d, and medazepam dosage was 5mg/night. The patient on sodium valproate took 1000mg/d split into 2 doses, while the patient on oxcarbamazepine took 300mg/d, also split into 2 doses. Response was very good (cessation of conversion episodes, BMCS) in 10 patients and good (appreciable reduction in episodes) in 13 patients, while there was no response in 2 patients on propranolol alone. Substantial, although less marked, improvement was also achieved in MWA and BM. Flunarizine (5mg/night) stopped all symptoms in 1 patient with BMCS. Sodium valproate (1500mg/d) alone was used in 1 patient, who failed to improve. Topiramate alone (maximum dosage: 200mg/d) was ineffective in 1 patient. This patient also showed no response to amitriptyline alone (maximum dosage: 50mg/d) or fluoxetine (20mg/d). Anxiolytics (diazepam 10mg/d and alprazolam at a maximum dosage of 0.50mg/d) were effective in 3 patients with a high anxiety component.
Suggestion was attempted in all patients with chronic symptoms. It resulted in cessation of dysarthria in 1 patient who had been suffering from this disorder for months, although it came back a few months later; in partial improvement of hemiplegia in 2 patients (only during the hypnotic trance); and worsening of tremor in 1 tremor patient.
Illustrative casesCase 2This 34-year-old woman had a history of headache since adolescence during times of emotional stress. Headache was frontal and biparietal, extremely severe, with loss of visual acuity in both hemifields, diplopia, general malaise, overall weakness and frequent losses of consciousness lasting around 5min. She reported that, on regaining consciousness, she was disoriented and weak with heightened sensitivity in the left half of her body for 1–2 weeks. Full episodes recurred every 1–2 months. The left-sided deficit became permanent at age 30. The left-sided hemiparesis did not include the face and left the upper limb hanging limp. The patient was unable to make any sort of movement, but if she held both arms outstretched in front of her (Barré test), the paralysed limb remained extended for a few seconds before dropping. If the examination was carried out with the patient reclining on the examination table, this tonic persistence was more pronounced. The limp condition of the arm and forearm decreased appreciably during spontaneous movement (turning over on the table, dressing) and then came back. Some distal hand movement was recovered under suggestion. The dissociation between the subjective and the objective was more evident in the lower limb, with Todd's paresis that was positive for Hoover's sign. Deep tendon reflexes were normal and the plantar reflex response was flexor in both feet. Repeat EEG, cranial CT, cranial and spinal MRI, central motor conduction time and PET and SPECT scans were normal. Psychiatric evaluation yielded a diagnosis of anxiety and histrionic personality. Treatment with anxiolytics and propranolol relieved the headaches but achieved only partial improvement of the hemiplegia.
Case 11This 55-year-old man was sent to the Meco penitentiary and was referred to our hospital to adjust the medication dosage for “uncontrolled epilepsy”. His mother suffered from convulsive episodes of undetermined origin. His son suffered from headache and pseudoepileptic fits (Case 1). The patient had suffered similar headaches since childhood. They began with a confused mental state and unsteady gait, nausea, vomiting, phonophobia, photophobia and holocranial headache. Headache was sometimes more severe, which the patient associated with feelings of frustration; on these occasions, the symptoms described were supplemented with anxiety and collapse, with pronation of the left arm, flexion of the third finger and extension of the remaining fingers, hyperextension of the knee, and plantar flexion of the foot while on the floor. These symptoms were also accompanied by non-rhythmic shaking of the entire limb and flexion/extension of the neck. After a minute, the shaking would cease and patient would begin to sob. Headache persisted for the rest of the day. The episodes could also be brought on by suggestion or triggered by “thinking about unpleasant situations for a long while.” The neurological examination was normal. Two EEGs (1 immediately after an attack) were normal. Cranial CT was normal. Episodes decreased with anxiolytics and propranolol (120mg/d).
Case 17This 52-year-old woman's mother suffered from headache, but there was no history of headache in other close relatives. Since she had turned 40, she suffered from recurring headaches, which at their most intense included “lights in her eyes” and “bright flashes” in both hemifields, unsteady gait, a sensation that her surroundings were spinning, transitory memory loss, disorientation and, on one occasion, diplopia. At this point the symptoms either tended to recede or else they continued with a sensation of “increased shaking inside,” apparent myoclonic arm contractions and collapse with loss of consciousness for several minutes or hours. On 6 occasions, right-sided hemiplegia and numbness persisted for variable lengths of time (12h–7 days), resulting in multiple admissions. Neurological examination during an episode revealed unidirectional nystagmus with broad movements not described on other admissions and a right-sided hemiplegia that did not include the face, with Todd's paresis and Hoover's sign. Suggestion elicited myoclonic jerks and weakness consistent with the symptoms described above. The episodes were not brought on by stress, but the patient lived in highly charged emotional circumstances because of serious family problems. The findings of multiple EEGs, cranial CT, cranial MRI, MR angiography and conventional angiography were normal. Treatment with flunarizine (5mg at night) and aspirin (300mg/d) stopped the motor symptoms and sensation deficits, but the headaches persisted.
Case 33This 32-year-old woman had suffered from headache since her menarche at 12 years of age. She had no first-degree relatives with headache. Headache was intense and hemicranial radiating to the back of the neck; the pain course was associated with nausea, phosphenes in the whole visual field, and some mental confusion with no recall of what had taken place. When the headache was especially severe (often during menstruation), she felt increasingly anxious and both her hands and her left leg, or both lower limbs, gradually began to shake, after which she would collapse onto the floor; this was followed by violent spasms in the trunk alternating between emprosthotonos and opisthotonos for about 15–20min. Elevation of the trunk during hysterical arching was so severe that family members had to sit on top of her to stop the contractions. The EEGs were normal when episodes were elicited by suggestion. Psychiatric evaluation concluded that patient exhibited histrionic personality disorder and severe anxiety. Imaging (cranial CT and MRI) results were normal. Treatment with anxiolytics, amitriptyline and propranolol succeeded in reducing the frequency of the episodes.
CommentsDespite the highly diverse series of symptoms exhibited by our cases, which have been set out in full detail in the tables and mentioned in the exemplary cases discussed here, there was an underlying thread running through them that warrants their being regarded as a separate entity in its own right. Our patients suffered from migraine, mostly basilar-type migraine, with associated hysterical symptoms. Even so, to be able to consider this association to be singular in itself, our cases still need to be more clearly differentiated from related entities. Firstly, they must be differentiated from “migraine-induced epilepsy” (migralepsy). The association between migraine and epilepsy is a complicated one and has recently been revised.15,16 Epileptic seizures have been observed to coexist with basilar migraine.17 The stereotypical hysterical features and the normal complementary findings (EEG, video EEG, susceptibility to suggestion) rule out an epileptic origin in those of our cases that had pseudoepileptic seizures. The visual symptoms in our patients also differed from those in patients with occipital epilepsy and post-ictal headache, which can sometimes be mistaken for basilar-type migraine with visual auras.13 Likewise, our patients did not display the spike-wave EEG changes or the photoconvulsive response present in some cases of basilar-type migraine.16 This is not to say that there might not be some as yet unidentified common pathogenic mechanism that causes the hyperexcitable brain state giving rise to epilepsy, headache or hysteria. At the same time, Bickerstaff's “migraine-epilepsy syndrome” is still speculative and involves altered consciousness during basilar-type migraine or headache attacks and associated epileptic seizures and disorders in a small number of patients.17 In any case, no patients were diagnosed with migraine-triggered seizures or occipital epilepsy with post-ictal migraine at our Headache Unit.
Including hysteria makes differentiating this clinical association more complicated. DSM-IV is not specific enough to provide a precise definition of conversion disorder, and seemingly any non-organic manifestation suggestive of neurological or medical illness may come under the definition. Similarly, following the crisis of psychoanalysis, psychogenic features (common as a co-morbid condition in many “psychiatric” or neurological diseases) are not defining elements of disorders involving hysteria. Out of practical concerns, the International Headache Society has banished unclear concepts like “psychogenic headache.” Migraine itself, despite the many gaps in our understanding of its causes, should not be considered to be a hysterical illness, as it formerly was. There is an underlying genetic, clinical and biochemical basis that makes up an actual entity. Certain cases in which the psychogenic components cause basilar artery migraine to be considered “conversion hysteria” or “conversion headache” are not readily acceptable.18–20 Therefore, the term “psychogenic basilar migraine” has been avoided in favour of “migraine associated with conversion symptoms.”21 Similarly, the World Health Organization's definition of hysteria, with its emphasis on “motives” (“…motives, of which the patient seems unaware….”) or on “psychological advantage or symbolic value” has been deemed outmoded.22 In practical terms, the patients at our hospital suffered conversion symptoms in keeping with classical descriptions (such as pseudoepileptic fits, grand mal hystérique or “psychogenic abnormal movements”) and an emotional trigger or a contributing psychiatric co-morbidity was identifiable in most, but not all, of our patients. These facts suggest that psychogenic disorder is a condition that contributes to but does not cause the appearance of the conversion symptoms.
The association between migraine attacks and conversion symptoms was surprisingly high in the population area served by our hospital, compared with the very few cases reported in more densely populated areas. The relatively high prevalence in our district cannot be completely explained by the population at risk of hysteria (e.g., immigrants, Romani and prison inmates with low educational levels). In my view, not enough attention has been paid to this combination of symptoms since Babinski and its incidence is higher than suggested by the low number of reports.
Nevertheless, the existence of epileptic or, more likely, pseudoepileptic convulsions in migraine or headache in cases of hysteria has been described, if only in passing, from the earliest reports given in antiquity. A brief historical review will help us identify these patients in earlier times. In the first description of migraine (hemicrania), Aretaeus the Cappadocian (second century CE) said:
“This is … an illness by no means mild, even although it intermits, and although it appears to be slight. For if at any time it sets in acutely, it occasions unseemly and dreadful symptoms; spasms and distortion of the countenance take place; the eyes either fixed intently like horns or, rolled inwardly, move convulsively from this side to that; vertigo …”23 In the chapter dealing with hysterical (uterine) illnesses, he also observed cases with “voluntary and involuntary trembling … vertigo, and the limbs sink under her; headache, heaviness of the head, and the woman is pained in the veins on each side of the nose.”24 This description is suggestive of BM, although this is necessarily a speculative conclusion.
In his long experience, Charles Lepois (Carolus Piso, 1563–1633), one of the leading medical reformers of the Renaissance, described a hospice for hysterical patients suffering from paroxysmal loss of feeling, deafness, aphonia, tremor and paralysis associated with headache.25
Robert Whytt (1714–1776), who developed the concept of “nervous disorder,” also referred to headache, dizziness, visual disorders, double vision and mental confusion, in addition to hysterical convulsions, as frequent symptoms of this type of fit.25
In the first major modern treatise on hysteria, Traité clinique et therapeutique de l’hystérie, Pierre Briquet (1796–1881) set down 430 clinical case histories of hysterical patients. He wrote: “headache is one of the distortions of sensations most frequently found in hysterical women ….” The second case (Emile Laroche) suffered headache, dizziness, visual disorders, lowered consciousness and hysterical loss of feeling on one side of the body. Of 356 patients surveyed, 300 suffered from constant headache. Headache was throbbing headache in half the cases and it was associated in one third of the cases with dizziness, stammering, mental confusion (etourdissement) and memory lapse.26
Mrs Emmy von N., one of the foundational cases in psychoanalysis (1895), is another interesting case. In a lengthy clinical case history, Freud portrays a patient having a full range of symptoms, including dysarthria, mental confusion, tics, migraine, severe anxiety and a susceptibility to hypnotic suggestion. Freud did not overlook his patient's severe nuchal headaches, with “a sensation of icy pressure on the neck, rigidity and painful coldness in all the extremities, inability to talk and complete prostration. They usually lasted from 6 to 12h.”27 In a marginal note, he presciently wrote: “On subsequent reflection, I had to admit that what the patient called ‘neck cramp’ might have been organically determined, analogous to the states of migraine. In practice one sees many of these states, which have not been described, and which have such striking resemblance to classic attacks of hemicrania that one would wish to broaden the latter concept. It is well known that many neurotic women combine many hysterical attacks, such as twitching and deliria, with their migraine attacks. Whenever Mrs. Emmy von N. had neck pain, she also had an attack of delirium.”27
It was Babinski who, in an original contribution in 1890 that has been unfairly overlooked, described 4 cases of “migraine ophthalmique hystérique” at the Salpêtrière sanatorium, setting out this combination of symptoms with precision. Charcot also examined several of these patients, a young man and 3 young women (21, 16, 22 and 20 years of age). They suffered recurring episodes of headache preceded or accompanied by visual aura, associated symptoms suggestive of brainstem involvement (71 years before Bickerstaff's description of basilar artery migraine)28 and hysterical disorders.3 The first patient reported a bright, spreading scotoma with a jagged border that was initially in half the visual field, followed by bilateral blurring and shrinkage of the visual field upon visual field testing. These symptoms were sometimes accompanied by convulsions and depressive dysarthria (tristesse) to the point of losing the ability to speak. Furthermore, the patient exhibited numbness in the right half of his body, soft palate and pharynx, and occasionally diplopia in 1 eye. The attacks improved with bromides.
The second case was a young woman with right-sided sensory numbness (not only loss of feeling but also visual hemifield, taste and olfactory deficits, all located on the right side) associated with violent hemicranial headache, ragged scotoma and palpebral flutter. Symptoms were susceptible to suggestion and ceased in response to the sedative action of bromides.
The third case was another young woman who suffered from bright bilateral scotoma, mental confusion (obnubilation de l’intelligence), nausea and vomiting, occasional loss of consciousness, convulsions, dysarthria and loss of feeling on the right side following emotional distress. Symptoms were readily triggered and aborted by suggestion. Just as in one of our patients, simply thinking about her illness was enough to bring on an attack. In general, this patient responded well to bromides.
The last case was a 20-year-old woman with recurring episodes of bright bilateral scotoma with a jagged border that grew until she was left blinded, loss of feeling in the pharynx and right half of the body, bilateral shrinking of the visual field, monocular polyopia and temporal headache. These symptoms were associated with fits of hysteria in which she suffered contractions and grands mouvements, with or without loss of consciousness, which could be brought on by suggestion.
Babinski sought an organic cause for hysteria in this association of symptoms. Hysteria was an entity in its own right, and ophthalmic migraine was “directly dependent on hysteria and a manifestation of this neurosis.”3
Surprisingly, notwithstanding Babinski's detailed description, nearly no new cases with this association have been reported since that time. According to Pierre Janet, “After Charcot's death, hysteria seemed to disappear from the La Salpêtrière sanatorium.”29 In my opinion, towards the end of the nineteenth century, theoretical exhaustion set in as a consequence of the many controversies surrounding hysteria, and mainstream neurology lost interest in the subject. Babinski's observations fell victim to this chain of events and it seems only fitting to rehabilitate this association between hysteria and migraine as Babinski's migraine. Hysteria subsequently became the speculative core of psychoanalysis until the crisis of this therapy.30,31
Little was published about this association in the first half of the twentieth century and the few reports tended to neglect the details, without ever citing the French neurologist's own observations. In Spain the vast experience and excellent powers of observation of the neurologist Barraquer Ferré (1948) enabled him to identify “several histories of individuals who displayed hysterical or emotionally pathological manifestations and so on as a part of the cycle of migraine attacks. When this state persists, patients may now and then exhibit signs of hysterical dystonia, in all cases transitory.”32
Following a certain loss of interest in hysteria by psychiatry, a controversial paper by Slater33 revived the topic and, starting afresh, British doctors took the lead in the field of conversion disorder.34 Slater reviewed the subsequent status of patients diagnosed as suffering from hysteria (1 with BM) and found that a large majority later evinced an organic disorder. He recommended taking hysteria (“a disguise for ignorance”) out of pathology textbooks as an entity. Later series35–37 failed to bear out Slater's assertions and, although the term hysteria was removed from the DSM-IV, hysteria itself refuses to disappear.38 Despite the nosological distance separating us, this brief historical overview suggests that the association described by Babinski was formerly quite common.
The association between migraine and conversion symptoms did not reappear in the literature until 1995. Sánchez-Villaseñor et al published 4 cases of “psychogenic basilar migraine” that matched Babinski's observations, although he was not cited. The patients were 3 women aged 24, 30 and 38, respectively, and a 31-year-old man. Three had “ophthalmic” symptoms and all 4 had “basilar” symptoms. The most common symptom was altered consciousness. The hysterical symptoms were verbal unresponsiveness (although 2 were in a coma), hemiparesis, hemibody loss of feeling (in the 4 patients) and jerking limb movements (in 2 patients). Symptoms (including the basilar symptoms) were elicited in all 4 patients by suggestion with saline injection. None of the patients improved with antimigraine or antiepileptic medication. The authors offered no explanation for the association and placed questionable causal emphasis on the power of psychogenic factors.21
Certain cases of hysterical pseudoepileptic seizures have been associated with headache in large series.39,40 However, the association has not been examined in detail de novo.
Finally, the experience and historical references reported here suggest that BMCS is not a rare entity. These cases invite speculation as to the obscure nature of hysteria. Unlike Babinski, we do not suggest here that hysteria is an entity, but do accept hysteria as a symptom. Conversion symptoms are positive symptoms in the Jacksonian sense (excitatory or inhibitory effects on the body) manifested by atavistic responses (many common in early infancy, such as extension of the trunk in response to frustration) that come into being when a series of circumstances converge. In my opinion altered consciousness, basically lowered or narrowed consciousness, is the primary circumstance and may be caused by migraine-produced dysfunction of the brainstem, or by emotion or hypnosis. In these conditions (genetically determined or acquired), primitive hysterical symptoms may arise in susceptible individuals with poor control (or synthesis) of body schema (sometimes linked to hyperkinesia). The “psychiatric normality” and apparent absence of psychogenesis shown by 7 of our patients points to psychogenesis being only a co-factor in many cases but not the necessary causal element. The greater frequency of migraine, emotional states and “hyperkinesia” in women helps to account for the traditional differences in hysteria between the sexes. The pain (headache) itself, by restricting the extent of consciousness, may act as an additional factor helping to cross a threshold and setting off hysteria. Our cases do not suggest that conversive symptoms are a manifestation of focal dysfunction (a “hysterical nucleus”) caused by headache, like hemianopsia or oculomotor paralysis.
ConclusionsIn view of the paucity of published reports since Babinski's overlooked report, it seemed to be time for a comprehensive description of the clinical elements of these patients, who exhibit a combination of symptoms from 2 such richly symptomatic entities as headache and hysteria.
To conclude, Babinski, a highly perceptive observer, is due renewed consideration and BMCS also merits reconsideration as an entity that may be quite common and may respond to antimigraine medication, which could assist in partially deciphering the cryptic, long-standing condition known as hysteria.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: García-Albea E. Jaqueca asociada a trastorno de conversión (jaqueca de Babinski). Análisis de una serie de 43 casos. Neurología. 2012;27:125–35.