Hemispatial neglect is characterised by systematic omission of stimuli in the contralesional hemifield. This disorder affects such daily activities as getting dressed, eating, reading, or writing. Patients display a decreased ability to attend to, explore, and respond to novel or significant stimuli on the side opposite to the injury. This impairment cannot be attributed to presence of homonymous hemianopsia, which sometimes coexists with hemispatial neglect.1 This frequent complication of right-sided vascular lesions2 has also been described in patients with multiple sclerosis,3 neurodegenerative diseases,4 or head trauma.5,6 We present a case of hemispatial neglect after severe head trauma.
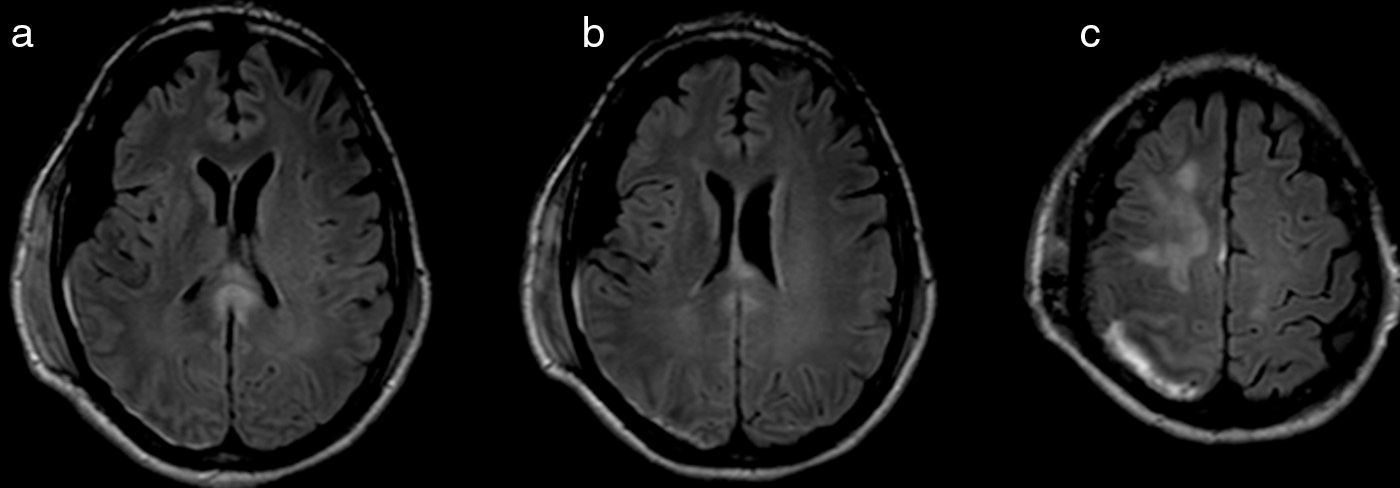
Our patient is a 52-year-old right-handed man with no relevant medical history who experienced severe head trauma after falling in a suicide attempt. When the emergency medical services arrived on the scene, the patient had a Glasgow Coma Scale score of 6, a bleeding scalp wound, and numerous associated contusions. Brain CT performed when he was admitted to the emergency department displayed a comminuted fracture of the right parietal bone; the largest fragment was depressed. Subdural haematoma was identified in the right hemisphere, with a subarachnoid haemorrhage and the haemorrhagic contusion site in the parietal lobe. We found no midline shift, and the ventricular system was symmetrical and of normal size. Bone fragments were excised and the parenchyma of the right cerebral convexity was resected. A subsequent brain MRI (Fig. 1) displays a right frontal parenchymal lesion; a right subdural supratentorial haematoma with a discrete mass effect on the right hemisphere and right lateral ventricle and no midline shift; multiple microbleeds in the cortical and subcortical areas of both hemispheres, and around the lateral ventricles; and signal changes in the body and splenium of the corpus callosum.
Axial T2-weighted FLAIR MRI sequences. (a) and (b) Resection of the parenchyma of the right convexity and signal changes in the splenium of the corpus callosum. (c) Hyperintensities on the right superior area of the parietal cortex may indicate presence of blood and tissue damage associated with subdural haematoma.
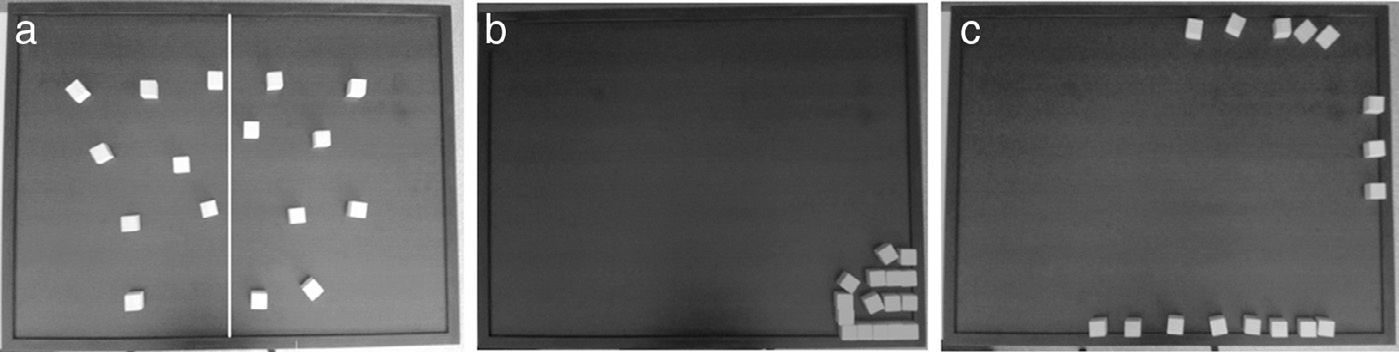
One month after the traumatic injury, the patient was transferred to our hospital to undergo neurorehabilitation. Upon admission, he was disoriented and showed bradypsychia and psychomotor restlessness. Four months after head trauma, it was possible to conduct a formal neuropsychological examination, according to which the patient was oriented in time, space, and person and displayed preserved language skills. He showed verbal memory alterations (Rey Auditory Verbal Learning Test: short-term memory 35/75, long-term memory 2/15, and recognition 4/15) and executive dysfunction (Letter-Number Sequencing Test: 4/21; Wisconsin Card Sorting Test: number of categories 2/6, number of perseverative errors 32; Phonemic Verbal Fluency Test [3min]: total number of words 19). During the examination, the patient was observed not paying attention to stimuli in the contralesional hemifield; homonymous hemianopsia had not been observed in the neurological examination. He was subsequently administered a specific neuropsychological testing protocol for assessing visuospatial attention (Bells Test, Ogden Figure Copying Task, Line Bisection Test, Baking Tray Task, and Reading Task); results confirmed presence of left hemispatial neglect. Ten days later, visuospatial tests were administered again; the patient showed slight improvements in task performance (Fig. 2).
Performance on one of the tests included in the protocol for assessing visuospatial attention (Baking Tray Task).13 (a) Healthy subject: cubes are evenly distributed over the board. The dividing line shown in the picture was added intentionally to this figure; it is not visible during the test. (b) Our patient's performance 127 days after head trauma. The image shows a marked tendency to place the cubes on the right side of the board. (c) Performance 10 days after the previous testing session.
Although hemispatial neglect commonly presents in patients with lesions in the right hemisphere, recurrence after head trauma is infrequent. Left hemispatial neglect has traditionally been associated with vascular lesions in the right parietal lobe.7 At present, this condition is linked to right-hemisphere lesions, more specifically in the superior temporal gyrus, temporoparietal junction, and inferior parietal region.8 Likewise, several authors have suggested that structural changes in certain areas of the right frontal lobe may cause hemispatial neglect.9 Danckert and Ferber8 support the idea that left hemispatial neglect is caused by extensive lesions affecting the functional system formed by those brain regions. According to these authors, a focal lesion in the inferior parietal or right superior region is not very likely to cause this condition by itself. Mesulam proposes that contralateral neglect is caused by dysfunctions in the neurocognitive network whose cortical epicentres are located in the frontal cortex (involved in the intentional component of neglect) and parietal cortex (involved in the attentional component).10 In our patient, hemispatial neglect was probably due to presence of multiple lesions affecting function of Mesulam's proposed neurocognitive network, which plays a critical role in processing extrapersonal space. Those lesions include structural changes in the splenium of the corpus callosum (Fig. 1). Current hypotheses postulate that hemispatial neglect may be explained by a disconnection mechanism between the 2 parietal cortices resulting from damage to the posterior corpus callosum.11,12
Please cite this article as: García-Molina A, García-Férnandez J, Aparicio-López C, Roig-Rovira T. Heminegligencia espacial secundaria a traumatismo craneoencefálico. Neurología. 2016;31:64–66.