Anisocorias are a relatively frequent reason for consultation in neuro-ophthalmology units. They remain a diagnostic challenge for specialists as they may be due to several aetiological factors. In the absence of other accompanying symptoms, anisocorias are usually due to benign processes. Benign episodic mydriasis (BEM) is an isolated cause of intermittent pupil asymmetry in which the pathophysiology is still not fully understood; it is predominant in young women with migraine.
Subjects, material, and methodsWe describe the epidemiological and clinical characteristics of patients with BEM, assessed in a neuro-ophthalmology unit in a tertiary hospital.
ResultsA total of 7 patients were diagnosed with BEM, all of them females, with a mean age of 33±10 years. The patients presented with pupil asymmetry (n=5) and blurred vision (n=2), and 6 of the 7 patients had unilateral involvement. The duration of impairment varied from a few minutes to 48hours. Four patients (57%) had a clinical history of migraine without aura. The episodes in these 4 patients were recurrent (75%), often lasted for a few minutes (75%), and had associated blurred vision (50%). The neuroimaging studies were normal.
DiscussionBEM appears predominantly in young women. It is frequently related to a previous history of migraine, and the specialist must consider if it is a concomitant symptom of common migraine, migraine with aura, or ophthalmoplegic migraine. Although BEM has unilateral predominance, there may be alternation of the affected eye or even bilateral impairment during the same episode, which makes us question the adequacy of the term to describe the process. Imaging tests are not recommended in the absence of other accompanying symptoms, or in short-term episodes.
Las anisocorias son un motivo de consulta relativamente frecuente en unidades de neuro-oftalmología (UNO). Suponen un reto diagnóstico por la variedad de procesos que pueden ocasionarla. En ausencia de síntomas acompañantes, suelen estar ocasionadas por procesos benignos. La midriasis benigna episódica (MBE) es una causa aislada de asimetría pupilar intermitente, de fisiopatología no esclarecida y predominio en mujeres jóvenes migrañosas.
Sujetos, material y métodosDescribimos las características epidemiológicas y clínicas de los pacientes con MBE valorados en una UNO de un hospital terciario.
ResultadosUn total de 7 pacientes fueron diagnosticadas de MBE. Todas eran mujeres, con edad media de 33±10 años. Los motivos de consulta fueron asimetría pupilar (n=5) y visión borrosa (n=2) de presentación fundamentalmente unilateral (n=6). La duración fue variable, desde minutos hasta 48h. Cuatro pacientes (57%) presentaban como antecedente migraña sin aura. En estas, los episodios eran recidivantes (75%), de minutos de duración (75%) y asociaban visión borrosa (50%). Los estudios de neuroimagen (resonancia magnética cerebral) fueron normales.
DiscusiónLa midriasis benigna episódica se presenta predominantemente en mujeres jóvenes. Se asocia al antecedente de migraña y hace plantear si se trata de un síntoma acompañante de la migraña, un aura migrañosa o de migraña oftalmopléjica. De predominio unilateral, puede sin embargo existir alternancia del ojo afectado o ser bilateral de forma simultánea, lo que nos hace cuestionarnos la idoneidad del término. En ausencia de síntomas acompañantes y en episodios de corta duración, no consideramos necesaria la realización de pruebas de imagen.
Pupil asymmetry is a relatively frequent reason for consultation in both emergency and neurology departments. It poses a considerable diagnostic challenge since it may have a wide range of possible causes, many of which are related to potentially severe conditions. However, in the absence of other symptoms, anisocoria can be associated with benign conditions.
Benign episodic mydriasis (BEM) is an isolated cause of intermittent pupil asymmetry. The underlying pathophysiological mechanism is not well understood, although 2 possible explanations have been proposed: hypoactivity of the parasympathetic nervous system and hyperactivity of the sympathetic nervous system.1 Most patients have a history of migraine, although episodes can present without headache.2,3 The role of BEM in migraine patients is not completely understood and the question of whether transient pupil changes in migraine patients are migraine-like auras or an associated symptom is a source of debate.
The purpose of this study is to describe the epidemiological and clinical characteristics of a series of patients with BEM evaluated in a neuro-ophthalmology unit at a tertiary hospital. We also describe the characteristics of BEM associated with a history of migraine and review the potential connection between the 2 entities.
Subjects, material, and methodsWe prospectively selected all patients attending the neuro-ophthalmology unit at Hospital Universitario de Gran Canaria Dr. Negrín (Canary Islands) between 1 January 2008 and 31 May 2012. This is a tertiary care hospital covering a healthcare area of approximately 450000 inhabitants, corresponding to the northern part of the island of Gran Canaria. It also serves as the reference centre for Lanzarote island. Patients are referred to our unit from 4 main areas: neurology departments, ophthalmology departments, hospital emergency services, and primary care centres. Before the first consultation, doctors responsible for the neuro-ophthalmology unit screen all potential referrals. Patients who were subsequently evaluated at this unit were included in a Microsoft Excel® database. Reasons for consultation and final diagnoses are coded to avoid heterogeneity. The 2 head doctors at the unit are equally responsible for entering data in the database.
We included those patients whose reason for consultation was transient pupil asymmetry and those with a definitive diagnosis of BEM. Patients were diagnosed with BEM if they had a consistent history of transient pupil dilation whether or not it was associated with headache, and no other neurological symptoms or warning signs.
Once patients were selected, we reviewed their medical histories and gathered the necessary variables: (a) sex; (b) age; (c) reason for consultation; (d) referring department; (e) personal history, including migraine, arterial hypertension, diabetes mellitus, and tobacco use; (f) psychoactive drug use; (g) number of previous episodes; (h) duration of current and previous episodes; (i) affected eye in each episode; (j) associated symptoms; and (k) neuroimaging results.
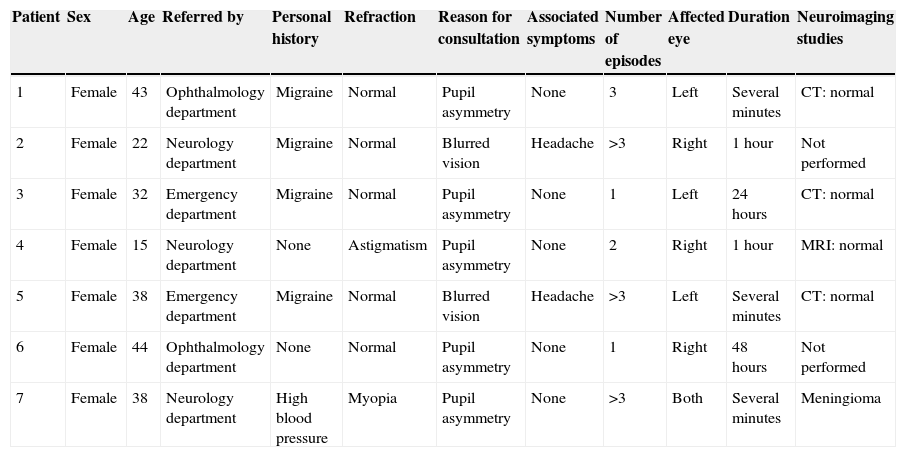
ResultsA total of 780 patients were evaluated in our unit during the study period. Of the 7 patients with BEM, all were female (Table 1). Mean (SD) age was 33 (10) years (range, 15–44 years). A considerable percentage of these patients (44%) had been referred by the neurology department; other referring departments included the ophthalmology and emergency departments. None of these patients reported tobacco use or diabetes, one was hypertensive, and 4 (57%) had migraine without aura. None of the patients was taking psychoactive drugs when symptoms appeared.
Description of the study population.
| Patient | Sex | Age | Referred by | Personal history | Refraction | Reason for consultation | Associated symptoms | Number of episodes | Affected eye | Duration | Neuroimaging studies |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 43 | Ophthalmology department | Migraine | Normal | Pupil asymmetry | None | 3 | Left | Several minutes | CT: normal |
| 2 | Female | 22 | Neurology department | Migraine | Normal | Blurred vision | Headache | >3 | Right | 1hour | Not performed |
| 3 | Female | 32 | Emergency department | Migraine | Normal | Pupil asymmetry | None | 1 | Left | 24hours | CT: normal |
| 4 | Female | 15 | Neurology department | None | Astigmatism | Pupil asymmetry | None | 2 | Right | 1hour | MRI: normal |
| 5 | Female | 38 | Emergency department | Migraine | Normal | Blurred vision | Headache | >3 | Left | Several minutes | CT: normal |
| 6 | Female | 44 | Ophthalmology department | None | Normal | Pupil asymmetry | None | 1 | Right | 48hours | Not performed |
| 7 | Female | 38 | Neurology department | High blood pressure | Myopia | Pupil asymmetry | None | >3 | Both | Several minutes | Meningioma |
MRI: magnetic resonance imaging; CT: computed tomography.
Reasons for consultation were pupil asymmetry (detected by the patient or more frequently by a family member), in 5 cases (72%), and blurred vision associated with headache, in 2 cases (28%).
Episode duration ranged from < 5min in 3 cases (42.8%), approximately 1hour in 2 cases (28.6%), and 24hours in one case (14.3%), to 48hours in another (14.3%). The number of episodes was 3 in 4 patients (57.1%), 2 in 1 patient (14.3%), and 1 in 2 patients (28.6%). In 4 patients (57.1%), the affected eye was always the same, while in 1 patient (14.3%) episodes alternated between the 2 eyes. None of the patients was able to identify any triggering factors for anisocoria episodes.
Since episode duration was very short in most cases, we were only able to evaluate symptoms in one patient (the one with an episode lasting 48hours). In all other patients, diagnoses were based on a consistent history of transient pupil dilation or results from examinations performed in the acute phase by other doctors. Two patients provided a video recorded during symptom activity showing pupil asymmetry, and they explained that their symptoms were temporary. At the time of consultation, both pupils were symmetrical and responded normally to light, so an eye drop test was not necessary. As our unit does not have a pupillometer, we cannot provide data on pupil size.
Four patients (57.1%) had a history of migraine without aura. In the same group, 3 patients (75%) had experienced at least 3 episodes of benign mydriasis; in 2 of them (50%) the motive for consultation was blurred vision associated with headaches resembling previous migraine attacks in terms of characteristics and intensity.
Physical and neurological examinations revealed no pathological findings. An ophthalmological examination showed astigmatism in one patient and myopia in another; results were normal for the rest of the patients.
All patients underwent a brain MRI scan which showed no pathological findings.
DiscussionAnisocoria is a frequent motive for consultation in emergency, neurology, and neuro-ophthalmology departments. Many different aetiologies for this entity have been described. Although anisocoria has traditionally been considered a neurological sign of poor prognosis, many of its causes are benign. Furthermore, many cases of anisocoria in patients evaluated in neurology or neuro-ophthalmology departments are due to benign causes, whereas anisocoria evaluated in emergency departments is caused by potentially severe processes in a higher percentage of patients.4 This highlights the need for an appropriate medical history and physical examination to detect warning signs associated with pupil asymmetry in order to rule out underlying structural lesions. In the absence of other findings, unilateral changes in pupil size are usually caused by benign processes, including episodic pupil asymmetry.
Pupil size depends on the balance between the sympathetic nervous system, which dilates the pupils, and the parasympathetic nervous system, which constricts them. Episodic pupil asymmetry, also known as BEM, is a condition whose pathophysiology is not yet completely understood. Several studies have suggested that episodic anisocoria in this entity is caused by changes in any of the 2 systems responsible for pupil size balance, that is, either parasympathetic nervous system hypoactivity or sympathetic nervous system hyperactivity.1
In 1970, Hallett and Cogan5 reported a case of episodic unilateral mydriasis in a young woman and described it as a benign condition of unknown origin. Since that first description, BEM has been found to be more common among young women,6 although it has also been described in children.3 Patients in our series were predominantly female: we identified 7 patients with BEM, all of whom were females aged 15 to 44 years.
In most of the cases and series reported in the literature, BEM is linked to a personal and/or family history of migraine,7 although some cases unrelated to migraine have also been described.2,3 In our series, 4 out of the 7 patients had a documented history of migraine. We were surprised to find that a migraine history was common among the patients with more numerous episodes (3 out of the 4 patients with 3 or more episodes) and those with shorter episodes (2 out of the 3 patients with shorter episodes). The connection between BEM and migraine is not precisely known. Some authors consider BEM to be a migraine aura,8 while most previous studies have regarded it as a non-aura symptom that accompanies migraine.7 It has even been described as a form of ophthalmoplegic migraine without impaired external motility involving the third cranial nerve.9 As mentioned above, episodes linked to migraine were more frequent in our series, and they lasted from several minutes to an hour. Furthermore, in 2 cases, episodic mydriasis preceded headache, which suggests that it may resemble an aura in some migraine patients. In addition, episodic pupil asymmetries are probably more frequent in migraine patients than previously thought and may therefore be regarded as one of the functional changes in migraine. These asymmetries may also be one of the causes of the frequently non-specific complaints of blurred vision made by migraine patients. However, since these phenomena are usually episodic, they may be overlooked or underdiagnosed.
Several studies have stated that the autonomic nervous system is involved in migraine pathophysiology, although as stated in the review by Zarruk et al., 10 roles have not been clearly explained for either nervous system. While results remain contradictory, there seems to be greater involvement of the parasympathetic nervous system (hypoactivity). However, sympathetic nervous system hyperactivity cannot be ruled out. A history of migraine in patients with higher rates of episode recurrence, short duration of mydriasis, and headache onset after episodes are 3 factors that suggest a connection between BEM episodes and the autonomic nervous system dysfunction typical of migraine auras.
Mydriasis episodes may be accompanied by blurred vision, orbital pain, eye redness, photophobia,11 and sometimes by poor near response and trouble focusing.6 The only visual complaints in our series were blurred vision and trouble focusing. We also note that orbital pain and eye redness are not characteristic of BEM episodes; when these symptoms are present, differential diagnosis must consider other causes for anisocoria.
Episode duration ranges from a few minutes to days or even weeks.12 In our series, episodes lasted <1hour in 5 of the patients (71.4%), and 48hours in only 1 patient (14.3%). The patients with longer episodes may be the ones with ophthalmoplegic migraine; in these cases, mydriasis has been linked to functional impairment of the parasympathetic fibres that follow the third cranial nerve, without impaired external motility involving that nerve. Inflammation has been proposed as the cause of anisocoria in ophthalmoplegic migraine,13 which may result in longer duration of mydriasis in these cases. Arunagiri and Santhi12 state that in ophthalmoplegic migraine, only one of the oculomotor nerves is affected (more frequently the common oculomotor nerve). Paresis may not be evident in these cases, but pupils are always involved.
Although this disease is predominantly unilateral, affectation may alternate between eyes in different episodes.12 In some cases, the disorder may even be bilateral and simultaneous. This causes us to question the suitability of the term ‘benign episodic unilateral mydriasis’; ‘benign episodic mydriasis’ may be a more appropriate denomination.
BEM, whether or not it is related to migraine, is a benign process with no associated structural lesions. No structural lesions were found in any of the patients in our series. We therefore believe that neuroimaging studies are not necessary for patients with BEM and no symptoms between episodes, nor are they needed in patients with a normal neurological examination. Brain MRI may be indicated in cases of long duration: the literature reports third cranial nerve hyperintensities in T2-weighted and FLAIR sequences and gadolinium contrast enhancement in patients with ophthalmoplegic migraine.13 The patient whose symptoms lasted 48hours did not show hyperintensities. However, the MRI scan was performed after symptoms had already resolved, which would reduce MRI sensitivity for these lesions.
Our study is limited in that we were unable to perform eye drop tests in any of our patients due to short symptom duration. As a result, we could not determine if primary alterations were caused by sympathetic or parasympathetic nervous system dysfunction. Furthermore, migraine and non-migraine groups could not be compared due to the small sample size (7 patients). However, we do believe that the description of these 7 cases provides a general perspective on BEM, showing its benign nature, its higher prevalence among women, and its connection with migraine.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martín-Santana I, González-Hernández A, Tandón-Cárdenes L, López-Méndez P. Midriasis benigna episódica. Experiencia en una consulta monográfica de neuro-oftalmología de un hospital terciario. Neurología. 2015;30:290–294.