Thyroid pain usually corresponds to subacute thyroiditis (SAT), characterized by markedly elevated inflammatory markers, moderate thyrotoxicosis, no isotopic uptake, and occasional systemic involvement. This possibly viral disorder usually responds quickly and completely to oral corticosteroids.1 Other less common causes of thyroid pain include intranodular hemorrhage, infectious thyroiditis, Riedel thyroiditis, and rapidly growing malignancies such as lymphomas and anaplastic carcinomas.2
Hashimoto's thyroiditis is characterized by intraglandular lymphocytic infiltration resulting in hypothyroidism, and is sometimes preceded by a hyperfunctional phase. Serologically, patients with Hashimoto's thyroiditis present positive anti-thyroid peroxidase (TPO) and anti-thyroglobulin antibodies, with negativity for TSH receptor stimulants that characterize Graves’ disease, though the disorder may sometimes be associated with eye and skin alterations like those seen in Graves’ disease. Hyperesthesia of the thyroid gland in response to palpation is common in the early inflammatory stages of the disease, and in isolated cases is associated with limiting pain. This condition is referred to as painful Hashimoto's thyroiditis (PHT). Such presentations are usually self-limiting and respond to oral corticosteroids. In some cases affected patients also respond to the start of thyroxine therapy. A relapse on corticosteroid treatment being reduced or a lack of response to therapy sometimes leads to the indication of surgery to solve the problem.3,4
We present two patients with PTH who, after failed oral therapy, received intrathyroidal triamcinolone injections, with an excellent response. Both patients gave their explicit consent to the publication of the present communication.
Case 1: A 36-year-old woman with contact dermatitis to nickel and PABA was referred in January 2015 due to pain in the region of the thyroid gland. Her sister and father had autoimmune hypothyroidism. The patient had experienced a tenderness of variable intensity in the region during the previous 9 months and provided an ultrasound report indicating thyroiditis of right-side predominance, with patchy hypoechogenic zones in the gland parenchyma. Firm and sensitive asymmetrical grade I goiter was palpated. The TSH concentration was 3.66μIU/ml (normal: <4.2), and the blood count indicated lymphocytosis – monocytosis, with an erythrocyte sedimentation rate (ESR) of 6mm in the first hour. After two months of oral prednisone dosing tapered from 30mg/day, with no improvement, treatment was started with l-thyroxine up to 88μg/day, with TSH 6.57μIU/ml, anti-TPO antibodies >600IU/ml (n<34) and C-reactive protein 0.10mg/dl. The patient showed progressive improvement, with long intervals between only minimum symptoms, until discomfort returned after 2 years despite adequate TSH levels (1.23μIU/l), and no relevant ultrasonographic changes. Treatment with intraglandular corticosteroids was proposed and accepted, and in April 2017 we infiltrated 40mg of triamcinolone acetonide (Trigon Depot®, Bristol-Myers-Squibb) diluted in 2ml of physiological saline solution, with a 21G intramuscular needle, distributing the solution in both thyroid lobes, in the ultrasonographic thyroiditis areas. The symptoms improved one week after the injection, with no side effects, and after 6months the patient was virtually asymptomatic, with normal TSH levels, the same replacement therapy dose, and diminished thyroid gland volume upon palpation.
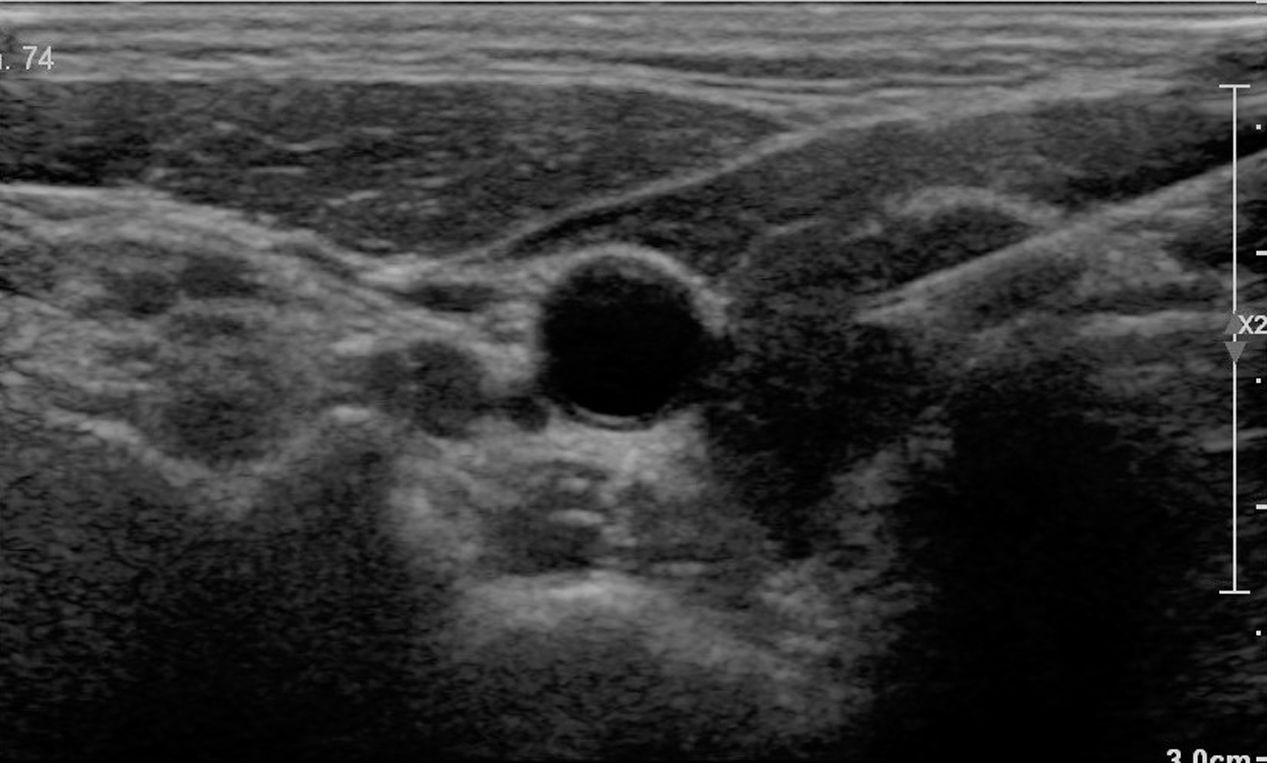
Case 2: A 47-year-old woman consulted in December 2016 coming from another center, due to increasing thyroid pain during the previous 6 months, with occasional ear pain and exacerbation when speaking. She worked as a teacher. The patient had been diagnosed with primary autoimmune hypothyroidism 8 years earlier, and was receiving replacement therapy with l-thyroxine, with adequate control (TSH: 0.84). Her daughter had eosinophilic esophagitis. The condition had been interpreted at her reference center as corresponding to SAT, despite ESR 3mm in the first hour and a fine needle aspiration biopsy revealing lymphocyte infiltration. She had been treated with nonsteroidal antiinflammatory drugs and subsequently with prednisone tapered from 45mg daily, with no improvement. The patient had also received high-dose omeprazole due to the possibility of peptic reflux. She presented an ultrasound report reflecting marked hypoechogenicity and profuse panlobular vascularization. Treatment with intrathyroidal corticosteroids was proposed. We administered 40mg of triamcinolone acetonide under ultrasound guidance and using the same technique as with the previous patient (Fig. 1). The pain subsided markedly within a week, with residual discomfort whenever she forced her voice. At the patient's request, a second infiltration was performed after three months using the same technique, and another two injections were made 6 and 12 months after the first. All the injections were well tolerated. Following the third injection the patient reported complete relief. However, after 5 months the discomfort returned, though with milder intensity and affecting only the left lobe. A fourth infiltration was therefore decided upon. After 5 months the patient remained asymptomatic and had returned to work. An atrophic thyroid gland was revealed at ultrasound.
The first reports of intraglandular corticosteroid administration date from 1974,5 and more than 30 years later its use in reducing the volume of goiters of different origins was described.6,7 In thyroid autoimmune disease, corticosteroids are used both systemically and locally to treat Graves’ ophthalmopathy, and either topically or in the form of local injections to treat pretibial thyroid dermopathy.8 The injection of 14 doses of dexamethasone in each gland lobe over a period of three months has shown a significant decrease in the Graves’ disease relapse rate,9 though its use has not become widespread, perhaps because of the aggressive nature of the treatment protocol. The treatment of PHT is important because of its impact upon patient quality of life, since speech exacerbates the symptoms by displacing the gland. In some cases, as in our second patient (a teacher), this may cause problems at work. Thyroidectomy is the standard option when drug therapy with thyroxine and/or oral corticosteroids fails.10 The intrathyroidal infiltration of triamcinolone was seen to be effective in both of our cases, with a progressive response to four doses in the most severe case. To the best of our knowledge, this has not been previously published. Of note in the first patient was the strong association of autoimmune disease, suggesting potent immune activation. Likewise of note in the second patient was the onset of pain after 8 years of hypothyroidism, which caused the condition to be initially mistaken for SAT.
In conclusion, we provide a new therapeutic alternative for painful Hashimoto's thyroiditis, where to date surgery has been the only alternative when other management options fail.
Please cite this article as: Paja M, del Cura JL. Tratamiento con glucocorticoides intratiroideos en la tiroiditis de Hashimoto dolorosa. Resultado en 2 pacientes. Endocrinol Diabetes Nutr. 2018;65:546–547.