Plasmablastic lymphoma is a rare and a relatively new entity that was first described in the jaws and the oral cavity of HIV-AIDS patients. We report a case of plasmablastic lymphoma involving the liver in an AIDS patient. Plasmablastic lymphoma is considered a diffuse large B-cell lymphoma with a unique phenotype and predilection for the oral cavity. The case presented had a unique hepatic lesion, localized in the left lobe of the liver. Diagnosis was confirmed by hepatic biopsy guided by Computerized Tomography scan and histopathology. The smears showed a dense infiltrate composed by atypical lymphocytes with numerous plasmocytes expressing the plasma cell markers MUM-1 and CD138 and negative for the B-cell markers CD3, CD20 and CD45. Immunohistochemical and in situ hibridization revealed the Epstein-Barr virus genome in the atypical cells. Polymerase chain reaction was negative for HHV-8 RNA.
Since 1985, lymphoma is an AIDS-defining illness and non-Hodgkin lymphoma (NHL) is the second most common neoplasm behind Kaposi’s sarcoma in these patients. Individuals with AIDS have a 100 to 300 times higher risk to develop a NHL in comparison with the general population. As well, intravenous drugs users have an additional risk among the patients with HIV infection.1
Plasmablastic lymphoma (PBL) is an aggressive and distinct sub-type of AIDS-related NHL. It is a frequent tumor in the oral cavity but is infrequent in other locations.2
Here we present the first case of plasmablastic NHL of the liver reported in an AIDS patient.
Case ReportA 47-year old heterosexual man, infected by HIV was admitted with a 20 days history of nauseas, vomit, abdominal pain and weight loss. Physical examination revealed a worsening condition, fever, epigastric and upper right quadrant abdominal pain and liver enlargement.
Significant laboratory findings included: hemoglobin 9.5 g/dL; hematocrit 28%; white cells count 3,300/mm3; platelets 215,000/mm3; alkaline phosphatase 157 U/L (N = 90 to 240 U/L) and lactate dehydrogenase 409 U/L (N = 230 to 460 U/L). Transaminase and alpha-fetoprotein levels were normal. Serological tests to detect specific antibodies against hepatitis B and C virus were negatives. The CD4 T-cell count was 37 cells/μL (8%) and the plasma viral load was over to 500,000 copies/mL.
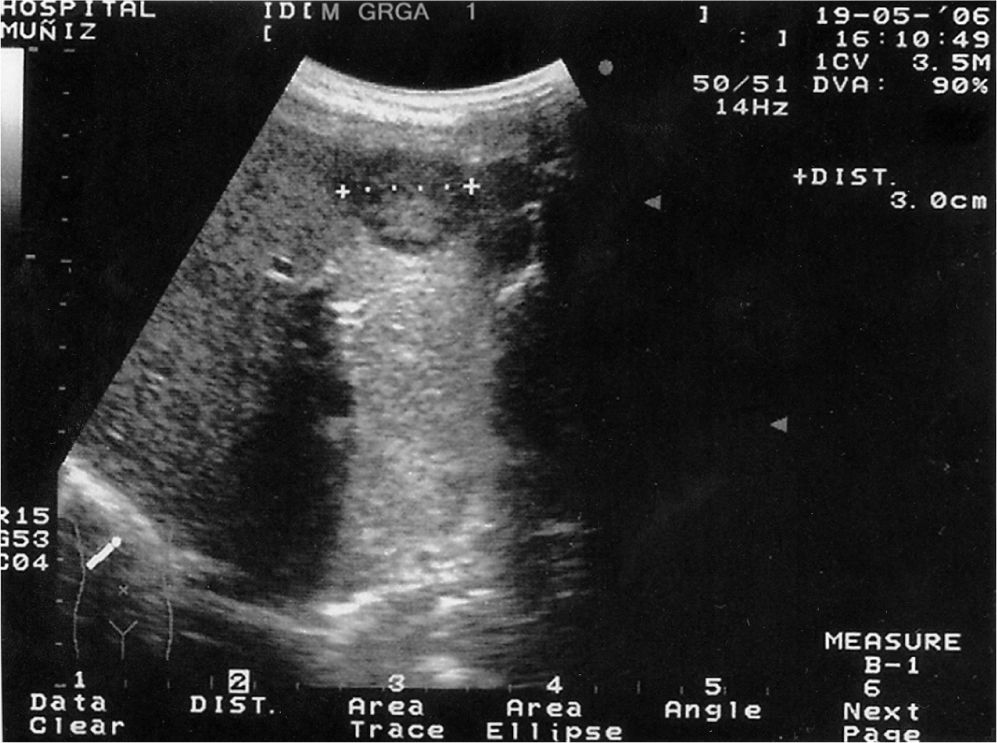
Abdominal ultrasound scan showed a heterogeneous large mass of 3 cm diameter, located in the left hepatic lobe (Figure 1) with contrast enhancement.
Bone marrow biopsy was negative to detect atypical cells infiltration. A computerized tomography (CT) scan of thorax, abdomen and pelvis showed hepatomegaly with the same lesion present in ultrasonographic examination.
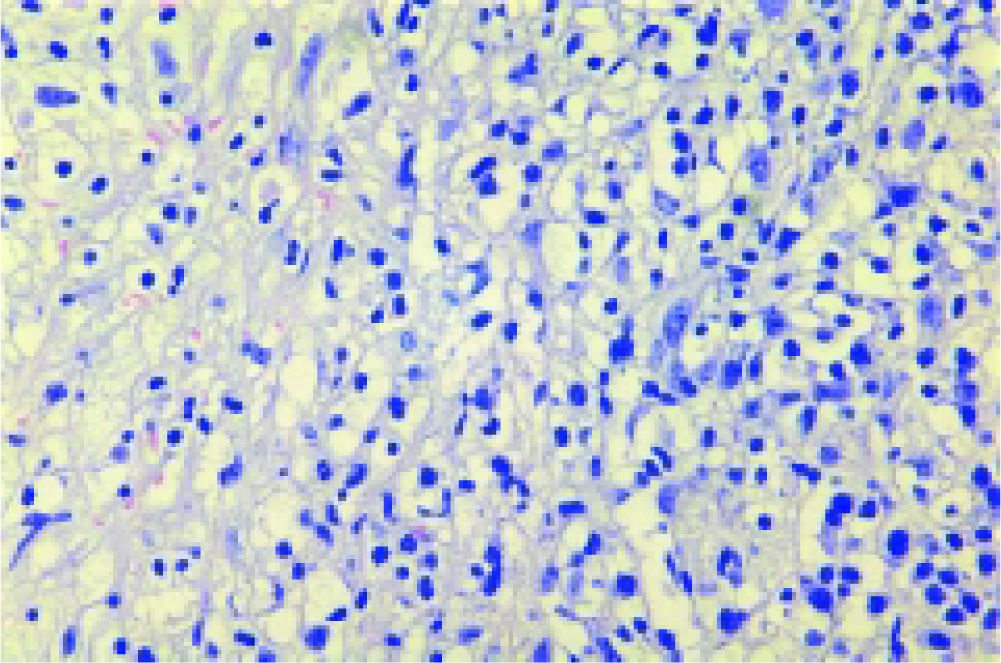
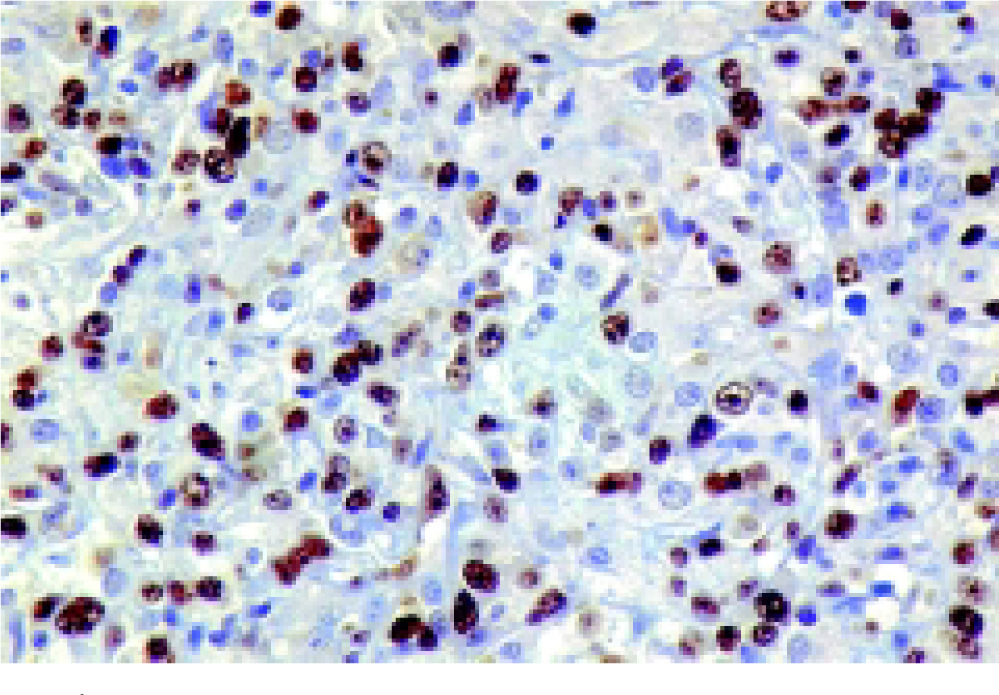
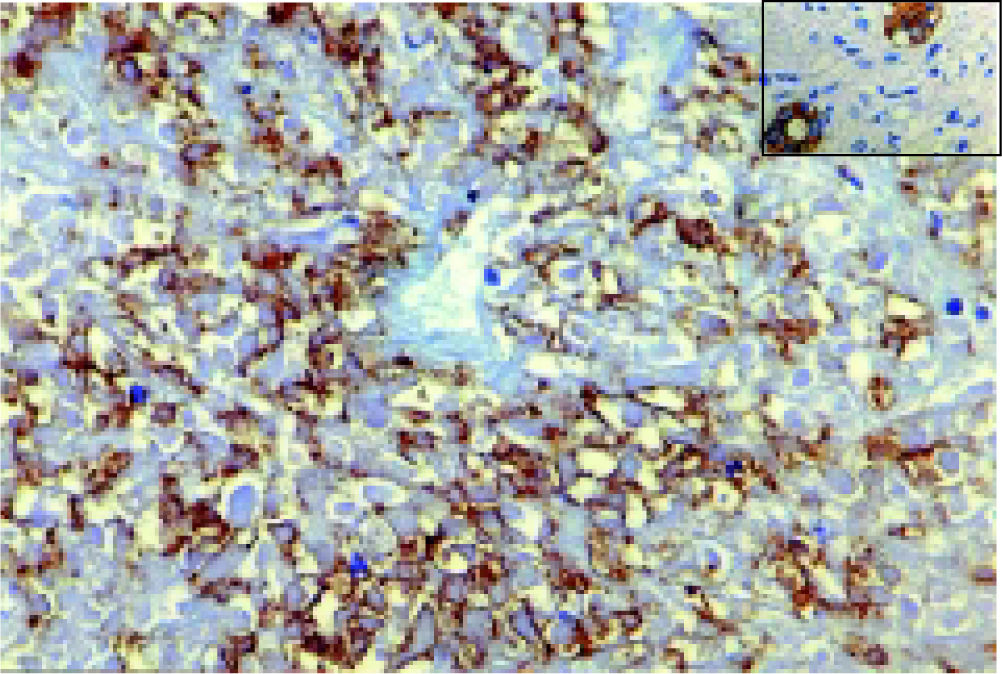
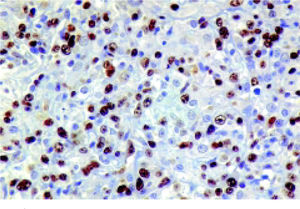
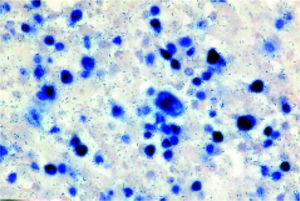
CT percutaneous-guided fine needle liver biopsy was performed. Histopathological examination of biopsy smears showed a dense infiltrate composed of a diffuse proliferation of large immunoblast cells with the typical morphological appearances of a high-grade NHL. Numerous cells had a plasmablast appearance (Figure 2). Immunostaining with monoclonal antibodies (DAKO - Glostrup, Denmark) showed atypical cells, negative for standard B-cell markers CD3, CD20 but expressing CD45, MUM-1 (Figure 3), CD138 and other markers of plasma cell differentiation. Bcl-6 was negative and the Ki-67 (proliferative) index was high (> 95% of the tumor cells) (Figure 4). Definitive histopathological diagnosis was high grade plasmablastic NHL.
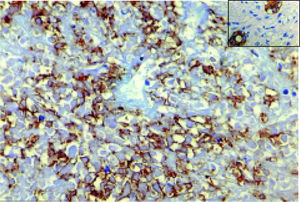
Epstein-Barr virus (EBV) associated latent membrane protein-1 (LMP-1) was detected in tumor cells by immunohistochemichal (IHQ) while EBV-encoded mRNAs was revealed by in situ hybridization (ISH) (Figure 5). Real-time polymerase chain reaction (RT-PCR) was negative to detect the HHV-8 RNA in the neoplastic cells.
Patient died three months after the diagnosis, despite one cycle of standard CHOP chemotherapy was carried on. The patient’s physical condition did not allow him to receive other cycles of chemotherapy.
DiscussionThe plasmablastic variant of diffuse large B cell lymphoma (DLBCL) is now considered to be a heterogeneous group of rare tumors, occurring especially in the context of HIV infection (PBL of the oral cavity).3,4
PBL was originally described in 1997 as a unique lesion in the oral cavity of an HIV seropositive male patient.5 Subsequently, it has been described in other sites as the skin, the stomach, the lung and the rectum, including HIV seronegative patients. In HIV-infected subjects this neoplasm occurs in up to 3% of the patients.6-9
PBL is a CD20 negative and a MUM-1, CD38 and/ or CD138 and VS38c positive large B cell lymphoma and the clinical course was aggressive and rapidly fatal without treatment.10 The World Health Organization (WHO) classification of lymphomas of the 2000 year includes PBL as a variant of DLBCL.11
Liver involvement is common in disseminated NHL, but less than 1% of extranodal lymphomas compromise the liver.12 Hepatic involvement in NHL, either primary or secondary, includes diffuse parenchymal infiltration or single/ multiple liver masses.13
Patients with AIDS related primary liver NHL generally present “B” symptoms (fever, night sweats and weight loss), abdominal pain and hepatomegaly, with or without jaundice at the time of diagnosis.
High grade, unfavorable histology and bulky tumor volume are associated with poor prognosis, as in our patient. Several series estimated a median survival time of only six months, including those patients who received chemotherapy.14
Ultrasonographic and computerized tomography scans might be helpful for the diagnosis of focal hepatic lesions in AIDS patients, but no imaging findings are specific for hepatic lymphoma.15 Our patient presented a single large and hypoechoic lesion with contrast enhancement in the sonographic images (Figure 1).
Image-guided needle fine biopsy of the liver is the best method for the definitive diagnosis of hepatic lymphoma, as we could observe in our patient.16
Several studies suggested that HCV plays a role on the pathogenesis of hepatic lymphoma and hepatocarcinoma. EBV is also strongly associated to the pathogenesis of NHL in AIDS patients.17 EBV genome is present in 35% to 50% of AIDS related NHL.
We could demonstrate the presence of EBV genome in the atypical cells by two techniques, IHQ and ISH (Figure 5).18,19
The Medline, Embase and Cochrane databases were searched to identify articles of PBL of the liver associated with AIDS. The search was performed using the following key words: plasmablastic lymphoma, liver, HIV, AIDS. To the best of our knowledge, PBL of the liver in a patient with AIDS has not been previously reported in the medical literature.
Liver lymphoma should be included in the differential diagnosis of single hypoechoic lesions in the ultrasonographic images in AIDS patients. PBL may occur in extra-oral sites in HIV seropositive patients, involving other organs as the liver, and should be considerer a poor prognosis malignancy.