Gender differences in attendance rates for appointments in delusional disorder have been poorly studied. Furthermore, delusional disorder is traditionally considered a treatment-resistant disorder.
Material and methodsWe conducted a longitudinal retrospective study with a one-year follow-up, including 78 delusional disorder patients (DSM-IV-TR), consecutively admitted over a period of 10 years. We performed a follow-up for one year in order to describe demographic and clinical variables, and to compare the therapeutic effectiveness. In this study, due to the non-interventional nature of this study, indirect measures were used to measure treatment effectiveness. The sample was divided into three groups according to the antipsychotic received at the first admission.
ResultsTwenty-three patients received Risperidone Long-Acting Injection (RILD), 30 oral risperidone, and 25 patients received other oral atypical antipsychotics. Delusional disorder women had a later age at onset and needed a longer duration of hospitalisation. No statistically significant differences were found between the three treatment groups as regards demographic data, social and personal functioning, and psychopathology at admission. The RILD group showed higher maintenance rates at the end of the follow-up period. Furthermore, the RILD group required treatment with antidepressants and benzodiazepines less often.
ConclusionsWe concluded that treatment with RLAI may increase maintenance rates at follow-up in DD patients when compared with other oral atypical antipsychotics.
Las diferencias de género en la asistencia a consultas por trastorno delirante han sido escasamente estudiadas. Además, el trastorno delirante es tradicionalmente considerado como un trastorno resistente al tratamiento.
Material y métodosSe llevó a cabo un estudio retrospectivo longitudinal que incluyó 78 pacientes con trastorno delirante (DSM-IV-TR) que ingresaron consecutivamente en nuestro centro en un período de 10 años. Se realizó un seguimiento de los pacientes durante un año con el objetivo de describir variables demográficas y clínicas y comparar la efectividad terapéutica. En este estudio, debido a su naturaleza no intervencionista, se realizó un análisis de las medidas de efectividad indirecta. La muestra se dividió en 3 grupos según el tratamiento antipsicótico recibido en el primer ingreso.
ResultadosVeintitrés pacientes recibieron risperidona inyectable de acción prolongada (RILD), 30 risperidona oral y 25 otros antipsicóticos atípicos orales. Las mujeres con trastorno delirante presentaron un inicio más tardío del trastorno y requirieron un mayor tiempo de hospitalización. No se encontraron diferencias estadísticamente significativas entre los 3 grupos de tratamiento con respecto a los datos demográficos, al funcionamiento social y personal, así como a la psicopatología en el ingreso. En el seguimiento durante un año el grupo RILD mostró un mayor porcentaje de permanencia al final del período evaluado. Además, el grupo RILD requirió con menor frecuencia un tratamiento con antidepresivos y benzodiazepinas.
ConclusionesConcluimos que el tratamiento con RILD podría disminuir las pérdidas en el seguimiento del trastorno delirante en comparación con otros antipsicóticos atípicos.
Delusional disorder (DD) is characterised by the presence of 1 or more delusions, insidious commencement and the resolution, and the course of the disease is chronic.1,2 It generally appears in the middle aged (between 35 and 55 years old).3–5
Epidemiological studies on delusional disorder have shown that it is more frequent in women than in men.6–8 However, classic authors such as Bleuler indicated that it occurred predominately (70%) in men.1
The most common type of delusion is the persecutory type. Its frequency varies slightly depending on the author (Someya et al., 64%; Portugal et al., 58%). The next in turn are jealous or mixed delusions,9–11 with rates again depending on the sources. In 33.1% and 64.8% of the patients other comorbid psychiatric disorders were observed12,13; affective disorder14 was the most prevalent (53.1%).
There is wide support in the literature for gender differences in delusional disorder.5,15 The disorder appears later in women than in men and most of the women present worse social functioning at the moment of admission; their hospitalisation is also longer.15–17 The Wusstman et al. study6 is based on the HADES (Halle Delusional Syndromes) study and found no gender differences in the type of DD or the frequency of depressive symptoms. However, women had greater compliance, received more antipsychotic drugs and presented higher rates for healthcare service usage than men.
Compliance with treatment is low in patients with delusional order, so it is traditionally considered treatment resistant.18 This is probably related to the former observation. Antipsychotics are considered the treatment of choice, given that they reduce agitation, anxiety and behavioural disturbances and, on the other hand, the fact that prognosis improves if patients comply adequately with treatment is well established.18,19
One common cause of treatment failure is deficient compliance with the treatment and the low percentage of attendance to the psychiatric consultations.18,20 In these cases, 1 option could be the use of a long-acting atypical antipsychotic, as greater treatment compliance and higher attendance rates have been observed in clinical practice with this type of drugs. In spite of this, there is a total lack of information about treatment with long-acting atypical antipsychotics except for report of cases of patients with DD.
It is a well-established fact that lack of attendance to outpatient consultations is a clinical problem in psychiatry. Patients who do not show up for their outpatient psychiatric appointments are found socially in a poorer situation that those keeping their appointments.21 This is important because only 42% of the first appointments set after being discharged from psychiatric hospital are kept and 25–50% of patients not showing up at their mental health consultation stop drug treatment.22
There was a study15 that covered the data available on treatment compliance and percentages of attendance to consultation for DD. It was observed that 17% of the patients with DD had a low treatment compliance rate, 42% present average rates and compliance was high in 38.6% of the patients. It is possible to find further information about the study design and the variable assessed in this study in the literature.
Considering the foregoing, our study had 2 main objectives:
- (1)
Investigate gender differences with respect to clinical and demographic characteristics and to the behaviour during follow-up on a sample of hospitalised patients with DD.
- (2)
Carry out an indirect analysis of the effectiveness of administrating risperidone long-acting injection (RLAI) in comparison to oral risperidone and other atypical antipsychotics by means of a registry of the percentages of attendance to the consultations between the treatment groups and any other psychoactive drug different from the antipsychotics clinically needed to improve the symptoms.
Using a retrospective design, we included all consecutive cases of patients hospitalised for DD admitted to the Psychiatric Service (Hospital Clínic, Barcelona, Spain) between 2000 and 2011.
This was the first admission to our Psychiatric Hospitalisation Service for all of the patients. They were assessed using a semi-structured interview. A psychiatrist recorded socio-demographic, clinical and treatment data during the first admission and in the ambulatory appoints after discharge. Data gathering was reviewed by a consultant. A systematic review of all the computerised medical records was used to establish the criteria of diagnosis according to the DSM-IV-TR23 during the first admission, as well as in the follow-up.
We defined the index episode as the first hospital admission following a diagnosis of DD. All of the patients received post-discharge follow-up for a year.
During the follow-up, we systematically recorded the clinical and socio-demographic characteristics, psychiatric comorbidity, attendance to the medical and nursing appointments and the long-term or oral antipsychotic use, as well as the antidepressants and benzodiazepines prescribed.
Due to the observational and retrospective design of the study, the patients were not assigned to a treatment group randomly. The psychiatrists chose the antipsychotic during the first admission of each patient taking into consideration the aspects listed below. Clinical characteristics such as the type DD, comorbid conditions of anxiety or depression and other clinical characteristics were not considered in making the choice.
- (1)
Patient case history. Clozapine was not prescribed for patients at risk for agranulocytosis or leukopenia.
- (2)
Patient age. Antipsychotics were prescribed for elderly patients only if their use was authorised for this collective.
- (3)
Patient weight. Sedating antipsychotics that increased weight significantly were avoided for overweight or obese patients.
With respect to the socio-demographic data, having fewer than 8 years of schooling was considered a very low educational level, a low level was established for 8–9 years of schooling, average was considered as 10–11 years and a high level was 12 years or more of state-regulated schooling. We also recorded the number of cohabitants and children, marital status and work situation of the patients as main psychosocial factors.
The clinical variables recorded were patient age at the time of admission, age of DD onset, length of hospital stay in days, delusional subtype, non-prominent associated hallucinations and affective or anxious symptoms, even when they did not reach the threshold of a specific disorder. General functioning was assessed using the Global Assessment of Functioning (GAF) scale. Also registered were the route of admission, motives for the consultation and rate of suicidal behaviour.
At the time of admission, the motives that led to the consultation were recorded using a classification based on the following 5 terms: pure delusions, depressive symptoms, anxiety symptoms, behavioural disorders and suicidal behaviour.
Indirect variables of effectiveness were registered during follow-up according to routine clinical practice. These variables included antidepressant and benzodiazepine use and the percentages of attendance to the psychiatric consultations during the first year following hospital discharge.
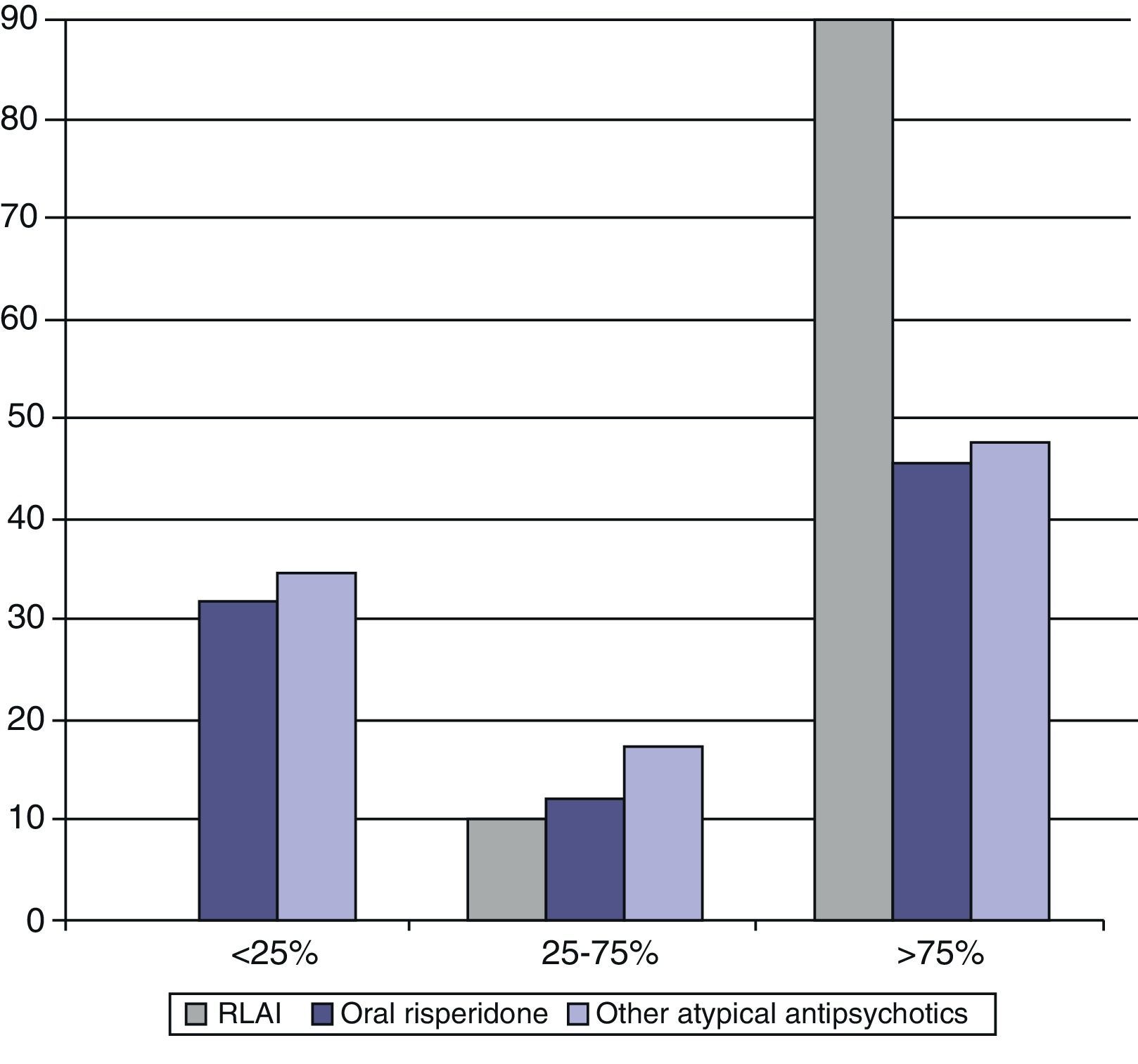
Operational definitions were established to assess the percentages of attendance to the psychiatric appoints during the first year of follow-up. The patients were classified as the ones that stopped attending appointments before 6 months, those that did so between 6 and 12 months from hospital stay and those that continued attending appointments at 12 months. Compliance with appointment attendance was defined according to the classification criteria used by Grover et al.15 The authors of that study divided patients into 2 groups: those that went to <50% or >50% of the follow-up appointments set up. However, the majority of the patients included in our study came to around 50% of the programmed appointments, while other patients did so in approximately 10%. For this reason, the patients were divided into 3 groups: the ones that came to <25% of the programmed appointments during the period of contact, those that came to between 25% and 75% of the appointments, and those that came to >75% of the appointments.
We analysed all data with the statistical programme SPSS for Windows (version 19). Descriptive statistics were used for the categorical variables, such as the clinical and socio-demographical characteristics, while the mean (±standard deviation [SD]) was calculated for the continuous variables. Univariate differences on clinical and demographic characteristics between men and women and between the treatment groups were calculated using Mann–Whitney's U and χ2 tests. The level of significance was set at P<.05.
We established multivariate differences with respect to appointment interruption and percentages of consultation attendance through multinomial logistic regression. The dependent variables were the cases lost during follow-up (<6 months, between 6 and 12 months and >12 months) and percentages of attendance to consultations (<25%, 25–75%, >75%); treatment groups (RLAI or other antipsychotics) were included as factors. To investigate whether the differences between the treatment groups as to the dependent variables showed bias from the presence of confounding variables, we included the variables gender, age at first admission and accumulated years of delusional disorder as covariables in the model.
ResultsSocio-demographic characteristics and risk factorsThe sample was composed of 78 patients that fulfilled the DSM-IV-TR criteria for DD. There were 20 men (25.6%) and 58 women (74.4%). The most frequent marital status was being single (46.2%), followed by married (25.6%) and divorced or separated (21.8%). The mean number of cohabitants (SD) was 0.88 (1.08) and the number of children, 0.74 (1.11). With respect to education, 17 subjects fell into the group of very low level, 24 of low level, 16 presented an average level and 21, a high level. As for work situation, 30 were employed, 24 presented an acceptable economic level due to their legal incapacity and 2 patients were in prison at the moment of hospitalisation.
Around 29.5% of the patients had a family history of psychiatric illness. The most frequent disorder in the first-degree relatives was schizophrenia in 12 cases (15.4%), followed by DD (n=4, 5.1%), major depression (n=4, 5.1%), anxiety disorder (n=2, 2.6%) and bipolar disorder in 1 case (1.3%). As for comorbid presence of sensory deficit, 4 patients (5.1%) presented conductive hearing loss and 2 subjects, (2.6%) neurosensory deafness.
Clinical characteristicsThe mean age at DD onset DD (SD) was 49.13 (12.04) years and the mean age of index episode was 55.38 (12.57) years. The most common path leading to hospitalisation was the emergency department (61.5%), followed by court order (16.7%) and voluntary admission (10.3%). Other reasons were less frequent. Overall functioning upon admission, assessed using the GAF scale, was lower than expected; the mean GAF score was 39.08 (6.14). The mean length of hospital stay (SD) was 25 days (14.84).
As the cause of admission, 52 patients (66.7%) presented behavioural disorders, 11 (14.1%) had isolated delusions, 6 (7.7%) presented anxiety symptoms and 6 (7.7%) were admitted due to suicidal behaviour. In the hospital assessment, suicidal tendencies were identified in 9 patients: 1 presented suicidal ideation, 5 had taken drugs to commit suicide, 1 tried self-defenestration, 1 swallowed a caustic liquid and 1 attempted to overdose with insulin.
The most common delusion was persecution (n=58; 74.4%), followed by erotomanic type (n=6; 7.7%), delusions of grandeur (n=2; 2.6%), the somatic type (n=5, 6.4%), jealous (n=4; 5.1%) and mixed delusions (n=3; 3.8%). As associated phenomena, non-prominent auditory hallucinations were observed in 6 cases (7.7%), non-prominent visual hallucinations in 1 case (1.3%), tactile phenomena in 6 subjects (7.7%) and olfactory hallucinations in 4 patients (5.1%).
All the patients were treated with antipsychotics, while a third received a combination of antipsychotics and antidepressants. Selective serotonin reuptake inhibitors (SSRIs) were used frequently (26.9%).
Furthermore, 56% of the patients also received benzodiazepines as an anxiolytic treatment: 22 subjects (28.2%) were treated with lorazepam, 13 (16.7%) received lormetazepam, 2 (2.6%) diazepam, 5 (6.4%) clonazepam and 2 cases (2.6%) received bromazepam. Only 4 patients received mood stabilisers (n=3, carbamazepine; n=1, valproate), while 9 patients received biperiden due to extrapyramidal side effects.
ComorbidityNo comorbid psychiatric disorders were shown in 47 patients (60.3%), as compared with the 39.7% that presented other comorbid conditions. Depressive disorders were the comorbidity observed most frequently (23.1%), followed by anxiety disorders (16.7%). Tobacco habit was presented by 23.1% of the patients. Out of the total sample, 2 subjects (3.8%) smoked fewer than 10 cigarettes/day, 9 patients (11.5%) smoked between 10 and 20 and 6 smoked more than 20 cigarettes a day. Eleven patients fulfilled criteria for alcohol abuse in the past and another 4 subjects presented a history of cocaine consumption, but they were free from toxic habits on hospital admission.
Gender differencesThe most common delusion in both women and men was persecution, followed by erotomanic and somatic in the women and jealous type in the men. No statistically significant differences were seen between men and women for marital status, educational level, number of cohabitants, number of children and work situation (Table 1). Women were admitted more often due to isolated delirious ideation, while the most frequent cause for the men was depressive symptoms (P=.011). In addition, the women became ill later than the men (50.05 against 46.45 years old); the age at first admission was also higher in the women (56.71 compared with 51.55 years), although without statistical significance (Table 2). Length of hospital stay was longer for the women than for the men (P=.045) and the women received more antidepressants (P=.029) and presented lower percentages of attendance to consultations during the first 6 months (Fig. 1). We found no gender differences with respect to the mean period between the first and second admissions.
Socio-demographic data at time of admission by sex.
| Women(n=58) | Men(n=20) | Value of P | |
| Marital status at time of admission (%) | 0.190a | ||
| Single | 41.4 | 60 | |
| Married/with common-law partner | 24.1 | 30 | |
| Divorced/separated | 25.9 | 10 | |
| Widow/widower | 8.6 | 0 | |
| Level of education (%) | 0.131a | ||
| Very low | 24.1 | 15 | |
| Low | 36.2 | 15 | |
| Medium | 17.2 | 30 | |
| High | 22.4 | 40 | |
| No. of cohabitants, mean (SD) | 0.83 (1.05) | 1.05 (1.19) | 0.343b |
| No. of children, mean (SD) | 0.84 (1.15) | 0.45 (0.5) | 0.090b |
P<.05.
Clinical characteristics at time of admission by sex.
| Women(n=58) | Men(n=20) | Value of P | |
| Age at onset in years, mean (SD) | 50.05 (11.9) | 46.45 (12.34) | 0.272b |
| Age in admission rate, mean (SD) | 56.71 (13.08) | 51.55 (10.33) | 0.200b |
| Length of hospitalisation in days, mean (SD) | 26.69 (15.44) | 20.05 (11.94) | 0.045b |
| GAF on admission, mean (SD) | 38.93 (6.51) | 39.50 (5.05) | 0.499b |
| No. of medical problems, mean (SD) | 1.40 (1.39) | 1.30 (1.46) | 0.691b |
| Motives for admission (%) | 0.011a | ||
| Pure thought disorder | 19 | 0 | |
| Behavioural disruption | 65.5 | 70 | |
| Anxiety | 8.6 | 5 | |
| Depressive symptoms | 0 | 15 | |
| Suicidal behaviour | 6.9 | 10 | |
P<.05.
Twenty-three (29.5%) patients received RLAI, 30 (38.5%) received risperidone oral and 25 (32.1%), other atypical antipsychotics. The sample was divided into 3 groups for the comparison by antipsychotic received: SSRI, oral risperidone or other oral atypical antipsychotics. No statistically significant differences were found between the 3 treatment groups with respect to the clinical and socio-demographic data, motives for hospitalisation and psychopathology on admission.
During follow-up no differences were observed between the 3 treatment groups in percentage of attendance at 6 months. However, the group receiving SSRIs showed higher percentages of consultation attendance after discharge (14/23 patients with appointment attendance above 75%) and higher percentages of maintenance at the end of the follow-up period as well (Figs. 2 and 3). In addition, the SSRI group required the use of antidepressants and benzodiazepines with a significantly lower frequency than the patients treated with other antipsychotics (Table 3).
Antidepressant and benzodiazepine use by antipsychotic treatment group (%).
| No ADs | AD | Total | No BZD | BZD | Total | |
| RLAI | 18 (78.3%) | 5 (21.7%) | 23 (100%) | 10 (43.5%) | 13 (56.5%) | 23 (100%) |
| Oral risperidone | 20 (66.7%) | 10 (33%) | 30 (100%) | 15 (50%) | 15 (50%) | 30 (100%) |
| Other atypical antipsychotics | 14 (56%) | 11 (44%) | 25 (100%) | 9 (36%) | 16 (64%) | 25 (100%) |
| Total | 52 (66.7%) | 26 (33.3%) | 78 (100%) | 34 (43.6%) | 44 (56.4%) | 78 (100%) |
ADs: antidepressant drugs; BZD: benzodiazepine; RLAI: risperidone long-acting injection.
The multivariate differences with respect to stopping appointment attendance were investigated by applying a multinomial logistic regression. For the cases of abandonment before 6 months with respect to those that stopped attending the consultations between 6 and 12 months, the chi-square value for gender prediction was 3.085 (P=.079). This indicates that gender is not statistically different from 0, given that age at first admission, accumulated years of illness and treatment were included in the mode. Wald's chi-square statistic for the predictive variable age at first admission was 0.806 (P=.061); for accumulated years of illness, it was 0.341 (P=.097); and for the treatment group, it was 1.428 with an associated P-value of 0.041.
The multivariate differences in the percentages of consultation attendance were also established using a multinomial logistic regression. For consultation attendances <25% with respect to 25–75%, no statistically significant factors or covariables of 0 were obtained. This indicates that the differences in the percentages of attendance cannot be explained by gender, age at first admission, accumulated years of illness or treatment group.
DiscussionUsing a retrospective design, we performed comparisons through transversal analysis at the time of admission and at a year's follow-up on the inclusion of all the patients that were admitted with DD in our Department of Psychiatry (Hospital Clínic, Barcelona) between 2000 and 2011. Our study objective was to investigate gender differences with respect to clinical and demographic characteristics, suicide attempts and percentages of attendance to consultations in a sample of 78 patients with DD. In addition, our objective was to carry out an indirect analysis of the effectiveness of the treatment received by patients with DD.
Our results confirm that DD is more frequent in women than in men. The women became ill at a later age and received psychiatric attention later than the men. These results are consistent with recent studies6,8 that observed a younger symptom onset age in men than in women and an older age for women's first psychiatric consultation than that of men. However, as has already been indicated, some classic and contemporary authors, such as Winokur, have found men to be over-represented.1,15
Our socio-demographic data indicated that the majority of the patients hospitalised with DD were single, divorced or separated; this contrasts with previous studies in which the marital status of married was the most frequent in this population.5 In our study, the mean age of disorder onset is 49 years, which is similar to that published in recent studies in our population area.7,9
The most frequent delusional idea was persecution, followed by erotomanic thoughts. These findings partially coincide with those of Portugal et al.,9 who found persecutory, jealous-type and mixed to be the most frequent delusion types. Furthermore, many recent studies have reported a preponderance of persecutory cases.10,16
Nevertheless, the validity and the usefulness of the current classification of DD into types are controversial. In a transversal study carried out by Portugal et al.,24 4 psychopathological factors (paranoid, cognitive, affective and schizoid dimensions) were identified using factorial analysis of PANSS (Positive and Negative Syndrome Scale) scores. These factors were related with cognitive functioning, substance abuse, over-all functioning and other clinical variables, which could provide help in forming a better concept of the types of DD.
The elevated psychiatric comorbidity prevalent in our study (39.8%), even though lower than in others, indicates that depressive and anxious symptoms can be considered part of the initial symptomatology and could be a cause of hospital admission.15,16 Our results showed that the women presented more hospitalisations and needed more drug treatment and that their percentages of consultation attendance during follow-up were lower than those of the men. These results coincide with those of Wustmann et al.,6 who observed that women required other drug treatments, such as the benzodiazepines, with greater frequency than men.
The second most common type of delusion in the women was the erotomanic, while in the men the most common types were the persecutory and the jealous. However, there were no statistically significant gender differences in type of DD. This is also compatible with the findings of Wustmann et al.,6 who did not obtain any gender differences with respect to DD types.
All of the patients admitted to our psychiatric department received atypical antipsychotics and other drug treatments when necessary. There is no information on treatments in DD that has sufficient statistical power and is based on randomised and masked controlled studies. Due to this lack of information, one of our objectives was to describe a profile of effectiveness for the antipsychotics routinely used in clinical practice. Our findings partially coincide with those of Grover et al.,15 who observed (in India) that response to treatment with risperidone was better than that of other antipsychotics but indicated the need for new studies to examine the effectiveness of the treatments in the types of DD. There was a systematic review of antipsychotic treatment in DD that did not reveal any significant differences between the various types of treatment with respect to outcome.25 However, as far as we know, this is the first study on DD to attempt to specifically describe percentages of appointment attendance related to the antipsychotic drugs administered.
In this study we found that patients treated with RLAI presented higher percentages of appointment attendance during follow-up than those treated with other antipsychotics or with oral risperidone. The differences in the appointment attendance percentages could be explained by treatment group in the multinomial logistic regression, even when gender, age at first admission and accumulated years of disorder were included in the model as covariables. Another point is that the patients treated with RLAI presented higher percentages of attendance to out-patient consultation appointments after discharge and higher percentages of appointment maintenance at the end of follow-up. However, when multinomial logistic regression was carried out including gender, age at first admission and accumulated years of disorder, treatment group did not predict the percentages of appointment attendance. In addition to this fact observed, we saw that the patients treated with RLAI needed antidepressants or benzodiazepines less frequently; this would be counted as a good finding of effectiveness.
Strengths/limitationsIn contrast to other studies, the strong points of our study was the investigation of the gender differences in depressive comorbidity, ideation and suicidal behaviour and the percentage of appointment attendance during follow-up in a sample of 78 patients with DD. Despite analysing indirect variables of the effectiveness, we compared the antipsychotic treatments most often used in DD in clinical practice. A study limitation is our reduced sample size, as well as the lack of assessment tools to evaluate the psychopathological symptoms (for example, the PANSS or the Brief Psychiatric Rating Scale for assessment) due to the retrospective and naturalist design of the study. For these reasons, we feel that lengthier and larger studies are needed to explain the absence of gender differences in the follow-up and the effectiveness of the recent atypical antipsychotics.
ConclusionsIt can be concluded that there are gender differences in DD in the ages of disorder onset, first admission and first use of psychiatric services, as well as in the length of the first hospital stay. Women need more drug treatments and how lower percentages of consultation attendance than men, which could indicate that DD is more severe in women than in men. Treatment with RLAI in DD could increase the rates of appointment maintenance during follow-up, but it cannot be concluded that the percentage of consultation attendance would be better. Patients treated with SSRIs seem to require the prescription of other psychoactive agents such as antidepressants and benzodiazepines less frequently. However, further studies are needed to confirm these preliminary results.
Ethical disclosuresProtection of people and animalsThe authors declare that no experiments were performed on human beings or animals in this research.
Data confidentialityThe authors declare that they followed their work centre protocols on patient data publication and that all of the patients included in the study received sufficient information and gave their written informed consent to participate in this study.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects mentioned in this article. This document is in the possession of the corresponding author.
Conflict of interestThe physicians González-Rodríguez, Molina-Andreu, Imaz Gurrutxaga and Rosa Catalán have no conflicts of interest to declare. Dr. Bernardo received fees as a consulter for Bristol-Meyer-Squibb and Wyeth, and fees from Janssen-Cilag, Eli Lilly, Pfizer, Synthelab, Glaxo Smith Kline and Astra-Zeneca; however, these personal relationships were not related to the content of our article.
We would like to thank the government of Catalonia, the Secretaria d’Universitats i Recerca at the Departament d’Economia i Coneixement (2009SGR1295), the Carlos III Health Institute, the Biomedical Research Centre in the Catalonia Mental Health Network (Red de Salud Mental de Cataluña) (CIBERSAM) and all the staff for their collaboration in carrying out the gathering of the clinical and demographic data in the medical registry systems. The work was carried out (in part) at the Centro Esther Koplowitz in Barcelona.
Please cite this article as: González-Rodríguez A, Molina-Andreu O, Imaz Gurrutxaga ML, Catalán Campos R, Bernardo Arroyo M. Estudio retrospectivo del tratamiento y uso de consultas en un grupo clínico de pacientes con trastorno delirante. Rev Psiquiatr Salud Ment (Barc.). 2014;7:64–71.