To describe the echographic characteristics of optic disk melanocytoma using a high resolution 10–20MHz ophthalmic ultrasound.
MethodsWe conducted a 10-year retrospective review finding 9 cases with optic disk melanocytoma. The echographic studies were performed by the same experienced ophthalmologist. The form and density of the tumors were evaluated with B-scan ultrasound. Internal reflectivity and vascularity of the tumors were assessed with a standardized A-scan. Base (vertical and horizontal) and height of the tumor were obtained by using both ultrasounds AB modes.
ResultsThe mean age at diagnosis was 43.88 years. There was no evidence of abnormal tumor vascularization in any of the cases. Mean (SD) vertical measurement of the base was 2.53mm (±1.47). Mean (SD) horizontal measurement of the base was 2.49mm (±1.03). Mean height (SD) was 1.52mm (±0.88). Of the assessable cases, 78% had high internal reflectivity, the remaining 22% had medium-high internal reflectivity. All tumors’ internal structure was characteristically homogeneous. Mean follow-up was 33.6 months.
ConclusionMelanocytomas are small, benign tumors that are highly assessable by ocular ultrasound when their elevation surpasses 0.5mm. In our study, the internal reflectivity ranged from high to very high, unlike other malignancies such as choroidal melanoma which tend to present with low internal reflectivity. The avascularity of the tumor is a common finding. Ultrasound is a remarkable tool that helps detect benign characteristics in a pigmented optic disk tumor and helps establish a more reliable diagnosis.
Describir las características ecográficas del melanocitoma de nervio óptico utilizando un ultrasonido oftálmico de alta resolución (10-20Mhz).
MétodosSerie de casos retrospectiva de 10 años. Se presentan 9 casos de melanocitoma de nervio óptico. El análisis ecográfico fue realizado por el mismo oftalmólogo experimentado. La morfología y la densidad de los tumores fueron evaluadas con ultrasonido modo B. La reflectividad interna y la vascularidad de los tumores se evaluaron con ultrasonido modo A. La base (en sus dimensiones vertical y horizontal) y la altura de los tumores se midieron utilizando ambos ultrasonidos modo AB.
ResultadosEl promedio de edad al diagnóstico fue de 43.88 años. No hubo evidencia de vascularidad anormal en ningún caso. El promedio (DE) de la medición vertical de la base fue 2.53mm (±1.47), la medición horizontal de la base fue 2.49mm (±1.03), y la media de la altura tumoral fue 1.52mm (±0.88). Del total de los casos, el 78% tuvo reflectividad interna alta y el 22% restante tuvo reflectividad interna media-alta. El 100% de los tumores tuvieron una estructura interna de características homogéneas. El promedio de seguimiento fue de 33.6 meses.
ConclusiónLos melanocitomas son tumores pequeños, benignos, que fácilmente pueden ser estudiados por ultrasonido ocular cuando su elevación sobrepasa los 0.5mm. En nuestro estudio la reflectividad interna varió de alta a media-alta, a diferencia de otras afecciones malignas como el melanocitoma coroideo, que se presentan con una reflectividad interna baja. La avascularidad del melanocitoma es un hallazgo común. El ultrasonido es una gran herramienta que nos ayuda a detectar características benignas en un tumor pigmentado del nervio óptico, ayudándonos a establecer un diagnóstico más fiable.
Melanocytoma is a benign and highly pigmented tumor that can emerge almost anywhere in the eye,1 such as the orbit,2–5 iris,6–10 ciliary body,11–18 choroid,19–21 sclera,22,23 conjunctiva,24 and the optic disk.25–32 The origin of these pigmented lesions is the migration of ectopic melanocytes from the lamina cribosa of the optic nerve head.33 The average age of diagnosis is 50 years, with a slight female predominance, and affecting both eyes in a similar proportion.32 This usually unilateral tumor has an equal incidence in all races, whereas uveal melanoma is more common in a white population.34 Referred to by different names in the literature such as magnocellular nevus or benign melanoma of the papilla.35
In the early twentieth century this type of tumor, then known as juxta-papillary melanoma, was considered malignant. Enucleation used to be the treatment of choice, but after observing that the majority of histopathological studies showed benign cells, this eventually lead to a modification in the treatment of this pathology, that remains valid to date.30,31
Most cases are asymptomatic (76%) which makes it difficult to estimate the actual prevalence in the general population.29 The leading causes of patient's complaints are low visual acuity (16%), scotoma (4%) and metamorphopsia (4%). An afferent pupillary defect may be present in 30% of cases despite excellent visual acuity.31,33
The typical papillary lesion is a dark brown or black pigmented tumor usually located eccentric and on the temporal side. It can spread to adjacent tissues such as the retina or choroid. The lesion can be flat or protrude with a mean elevation and diameter of 4mm and 10mm respectively. Association with choroidal nevus has been reported in up to 50% of cases.34,35
Usually, the diagnosis is established after an incidental finding during a routine ophthalmologic examination. Further studies like fluorescein angiography, perimetry, standardized A-scan and B-scan ultrasound, and fundus photography should be ordered to confirm the diagnosis and rule out the differential diagnosis such as melanoma.35–38
Melanocytomas are extremely slow-growing tumors. Shields et al. have noted growth in 11% of melanocytomas at 5 years and 32% at 10 years. Such invasion always involves the intraretinal part of the tumor and never its choroidal components. Three risk factors for growth have been identified: increased tumor thickness, the presence of intrinsic vascularization, and dome shape.34 Malignant transformation of a melanocytoma of the optic disk is a highly rare possibility, being found in only 1–2% of all reported cases. It has been observed primarily in white patients and can occur after many years of initial identification, emphasizing the need for long-term surveillance of this tumor.33
Limited data is available on the ocular ultrasounds findings in melanocytoma. This information is important as this data can be used to learn how these tumors can present and be correctly identified by ultrasound. As such, the purpose of this study was to evaluate the ultrasounds findings of optic disk melanocytoma.
MethodsWe conducted a 10-year retrospective review of 9 cases with optic disk melanocytoma. This study was approved by the hospital's ethics Committee and conducted in accordance with the Declaration of Helsinki. All patients had a comprehensive ophthalmological examination and fluorescein angiography before the study. Two angiographic studies were not available for analysis. All echographic studies were performed by the same experienced ophthalmologist, using Equipment Cinescan “S” from Quantel, with 10MHz “B” scan probe and 8MHz standardized “A” scan probe. The form and density of the lesions were evaluated with B-scan ultrasound. Internal reflectivity and vascularity of the lesions were assessed with a standardized A-scan. Dimensions of the tumor were obtained using both ultrasound AB modes by base (vertical and horizontal) and height. Ultrasound measurements for one patient could not be obtained given the small dimensions of the tumor.
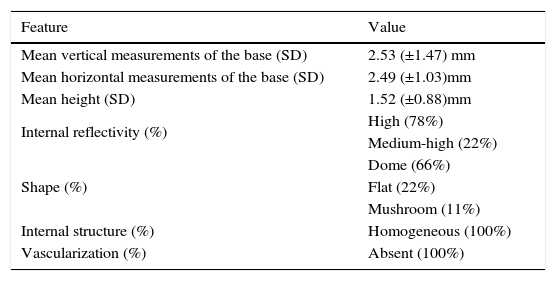
ResultsThe mean (SD) age at diagnosis was 43.88 (±14.44) years with a marked female predominance. Mean (SD) best-corrected visual acuity (BCVA) in affected eyes was 0.4267 (±0.5191) LogMAR. Melanocytomas were found predominantly in the left eye in 77% of the cases. The inferior temporal quadrant was the most involved (66%) in this case series. The retina adjacent to the optic nerve had tumor involvement in 38% of the cases. Angiography fluorescein findings revealed hypofluorescence in 71% of the cases, the remaining 29% were isofluorescent (angiographies of two patients were not available). Accurate ultrasound measurements were obtained in 8 of the 9 cases (88%). The remaining case could not be measured due to an elevation of less than 0.5mm. Echographic features are reported in Table 1. Mean follow-up was 33.6 months.
Ecographic features.
| Feature | Value |
|---|---|
| Mean vertical measurements of the base (SD) | 2.53 (±1.47) mm |
| Mean horizontal measurements of the base (SD) | 2.49 (±1.03)mm |
| Mean height (SD) | 1.52 (±0.88)mm |
| Internal reflectivity (%) | High (78%) |
| Medium-high (22%) | |
| Shape (%) | Dome (66%) |
| Flat (22%) | |
| Mushroom (11%) | |
| Internal structure (%) | Homogeneous (100%) |
| Vascularization (%) | Absent (100%) |
The following case exemplifies the utility of ultrasound accuracy for the detection of lesion dimensions, vascularization, and shape; allowing accurate monitoring of benign characteristics.
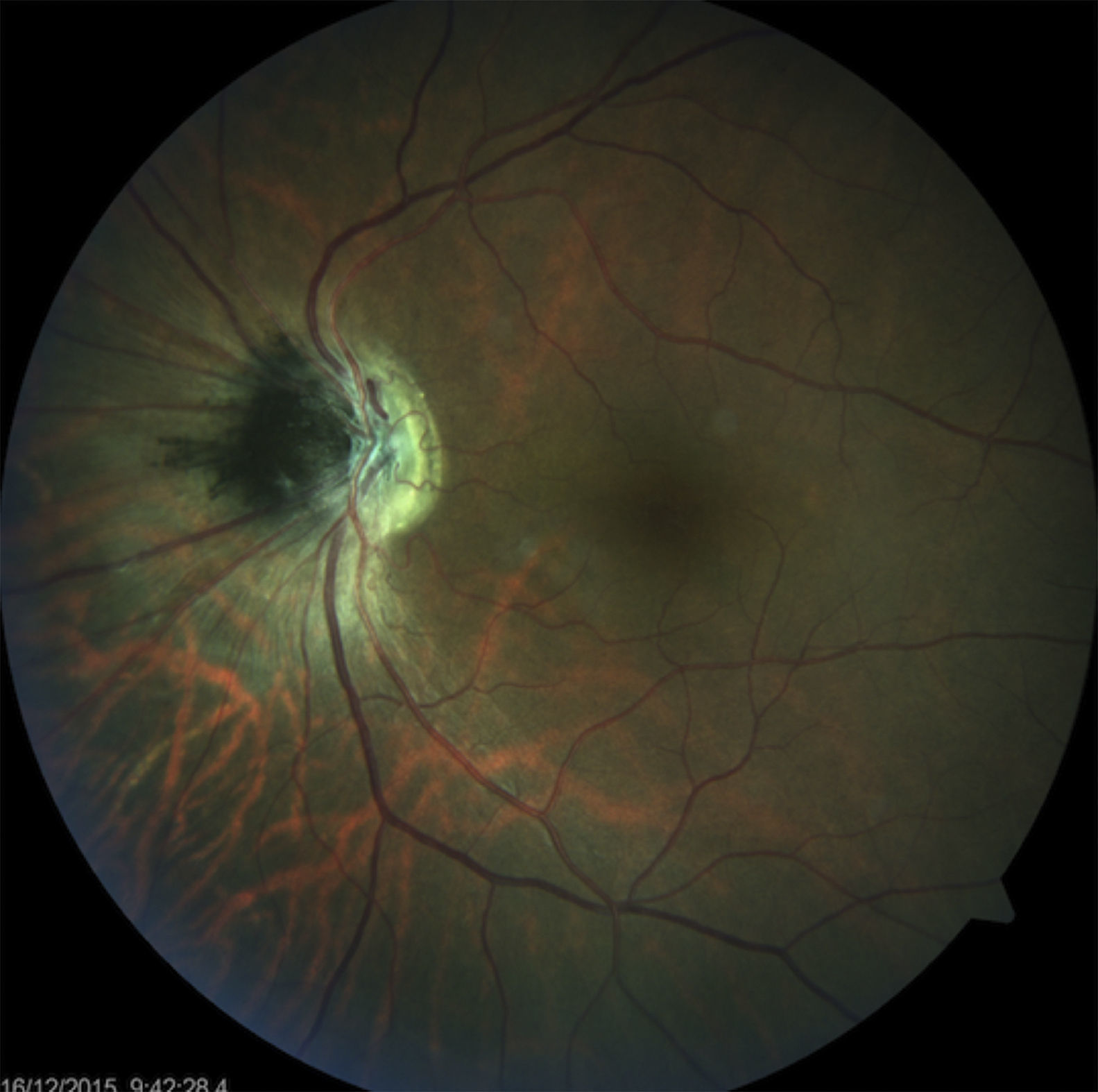
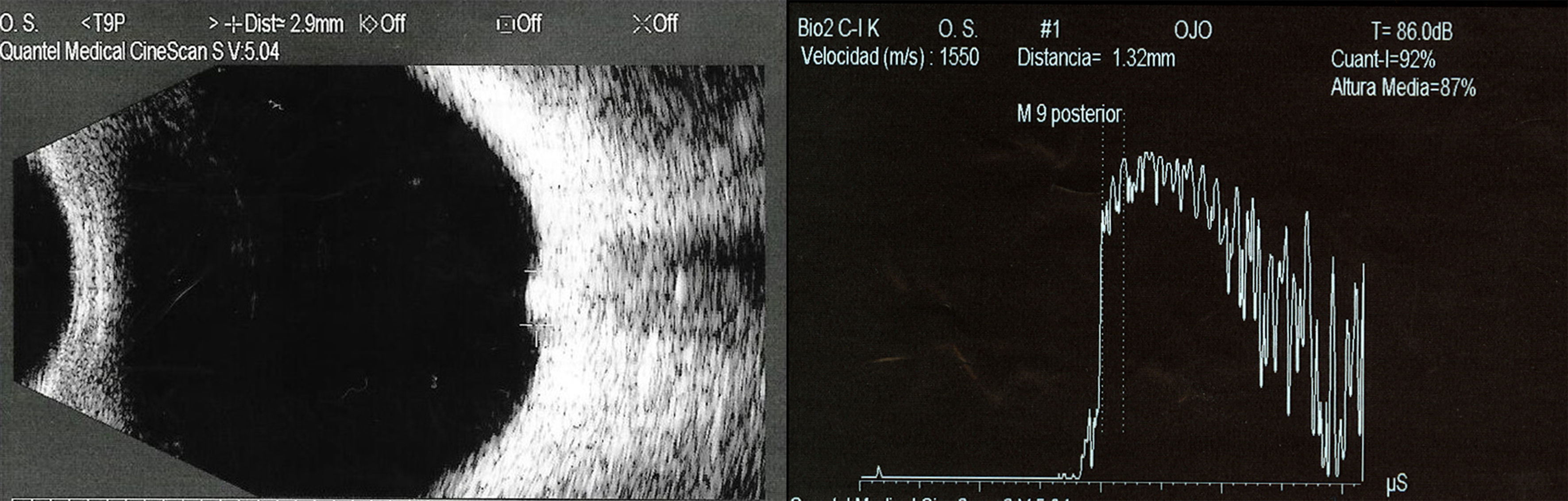
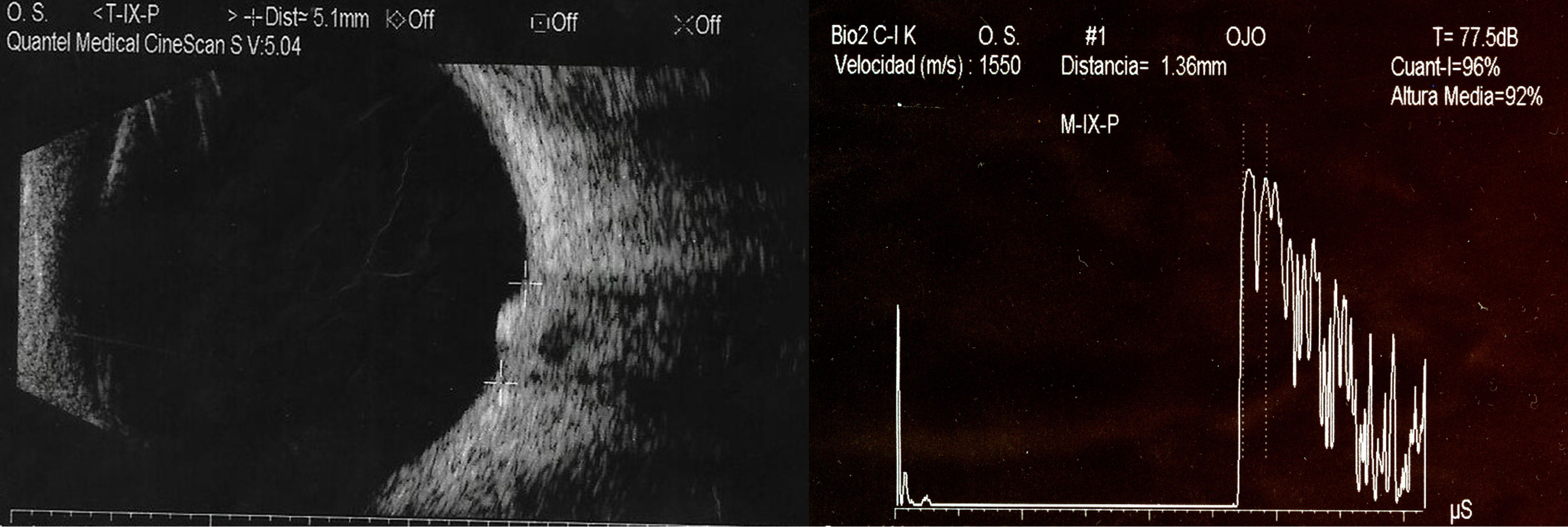
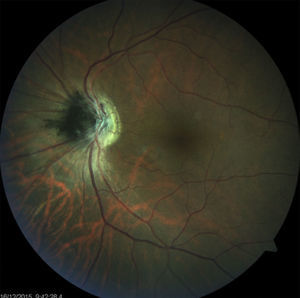
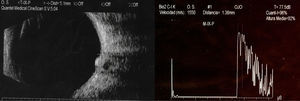
Case 1A 25-year-old male came to our hospital referring blunt ocular trauma 3 days before admission with decreased visual acuity in the left eye. Past medical history was not relevant. Visual capacity was 20/60 in both eyes with an IOP of 15mmHg. Exploration of the right eye was normal. The left eye had mild inflammation in the anterior chamber. Retina was completely attached, and no predisposing lesions were found. Optic disk showed an elevated, hyperpigmented lesion with invasion to the nasal retina, slightly smaller than 1 disk in diameter (Fig. 1). Standard ultrasound showed the dimensions of the highly reflective lesion to be 2.9×3.1×1.32mm (basal dimensions×height) with no vascularity (Fig. 2). Follow-up examination was continued every 6 months. Seven years later the ocular ultrasound was repeated; revealing increased dimensions 5.1×2.7×1.36mm (basal dimensions×height). The lesion was observed to be round, homogenous, avascular, and persisted with high internal reflectivity (Fig. 3). Since it remained asymptomatic and no signs of malignant transformation had yet appeared, we decided to continue follow-up with observation and ancillary testing.
DiscussionMelanocytomas are small benign tumors that are highly assessable by ocular ultrasound when, as documented by Shields et al., their elevation surpasses 0.5mm. Our series demonstrated that the age range at diagnosis was wide (18–67 years), very similar to the one reported by Gologorsky et al. (17–79 years). In our study, the internal reflectivity was high in 78% of the cases, compared with the same article as above which reports 73% with high and 12% with medium-high reflectivity; unlike other malignancies like choroidal melanoma that tends to present with low internal reflectivity. The invasion of adjacent tissues was a confounding finding discovered in more than a quarter of the cases. Shields et al. reports that about 85% of the cases, melanocytomas extend over the margin of the optic disk to involve the adjacent choroid or retina.29
The avascularity of the tumor is a common finding opposed to melanomas that are highly vascularized, absence of vascularization was found in all of our patients. Regarding tumor dimensions, although similar height, we observed that melanocytomas tend to have smaller base diameters compared to their malignant counterpart. The highest elevation reported was 3.1mm and the largest base diameter was 5.1mm, whereas according to Shields et al., mean height was 3.5mm and mean basal dimension of choroidal melanomas was greater than 11mm.31
Our study must be considered in the setting of its limitations. It is a retrospective case series with a limited number of patients. Despite these disadvantages, our study adds to the understanding of the ultrasound findings of optic disk melanocytoma in our population. This information is important for the clinician as it supports the idea that ultrasound is a remarkable tool that helps detect benign characteristics in a pigmented optic disk tumor and helps establish a more reliable diagnosis.
ConclusionUltrasound is a remarkable tool that helps detect benign characteristics in a pigmented optic disk tumor and helps establish a more reliable diagnosis. Although clinical follow-up is paramount, concomitant use of ultrasound helps us corroborate changes in previously benign characteristics, and allows us to accurately monitor tumor growth rate.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo endorsement of any kind received to conduct this study/article.
Conflict of interestThe authors declare no conflict of interest.