Blood transfusion is a valuable therapeutic tool for massive bleeding in spite of inherent risks and makes the difference between life and death. Rational use of blood components and particularly of red blood cells concentrates (RBC) request for surgery could minimize the transfusional reactions and financial burden for blood banks.
ObjectiveTo know the transfusion practice and the relationship between the request and use of RBC in programmed surgeries at the General Hospital of Mexico.
Materials and methodsA retrospective study was conducted and data analysis based in the number of RBC units required from the blood bank were compared with the number of RBC units transfused. Medical records, surgical notes, anesthesia worksheets, nursing and laboratory reports from a 6 months period, were reviewed.
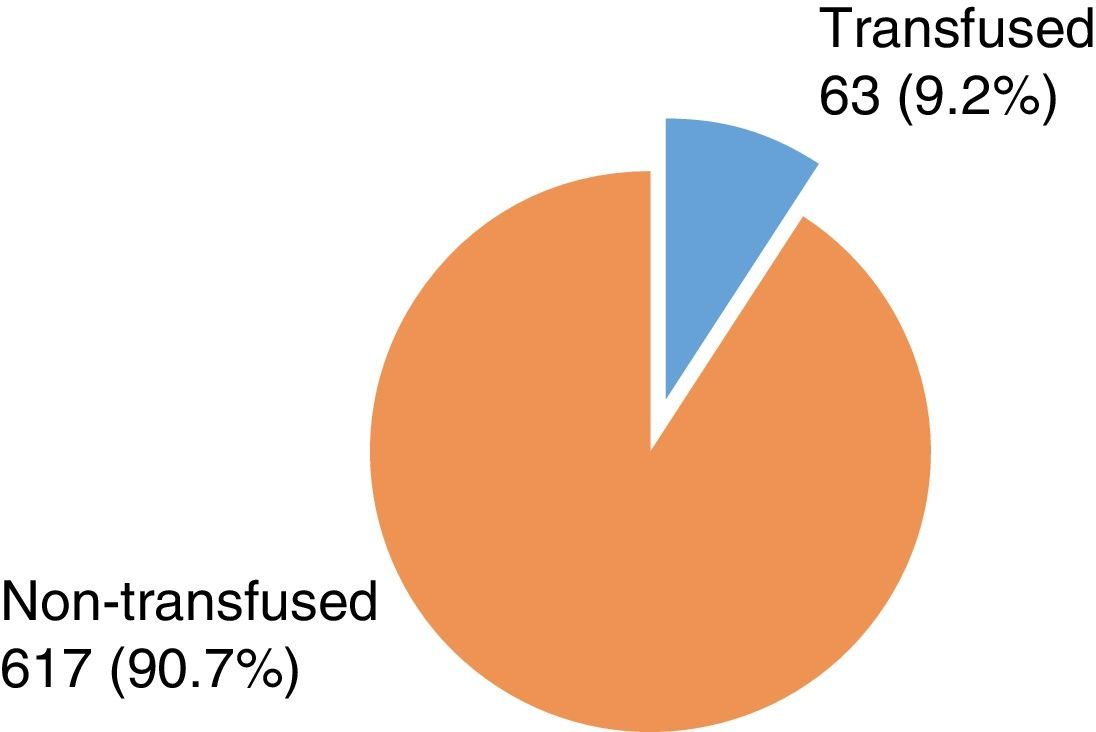
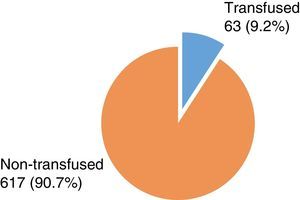
ResultsDuring the studied period, 354 RBC were requested from the blood bank from different surgical specialties; with a total of 680 units. From these only 63 (9.2%) were transfused vs 617 (90.7%) that were not used and were returned to the blood bank.
ConclusionsRBC requests were excessive compared to the real demand; this represents inadequate blood requests and elevated costs for the blood bank and the health system. There is a need to promote strategies through the institutional Transfusion Medicine Committee.
La transfusión sanguínea es una herramienta terapéutica valiosa para la hemorragia masiva; a pesar de sus riesgos, marca la diferencia entre la vida y la muerte. La solicitud racional de los concentrados eritrocitarios en cirugía, podría reducir al mínimo las reacciones transfusionales y el gasto financiero para los bancos de sangre.
ObjetivoConocer la práctica transfusional y la relación entre la solicitud y el uso de sangre en cirugías programadas del Hospital General de México.
Material y métodosSe realizó un estudio retrospectivo y análisis de datos basado en el número de unidades de sangre requeridas al banco de sangre comparándolas con el número de unidades transfundidas. Se revisaron notas médicas y quirúrgicas, hojas de anestesia y reportes de enfermería y laboratorio, en un periodo de 6 meses.
ResultadosSe analizaron 354 solicitudes de concentrado eritrocitario al banco de sangre; lo que equivale a un total de 680 unidades. De esta cifra, sólo 63 (9.2%) unidades se transfundieron y 617 (90.8%) que no se utilizaron y fueron devueltas al banco de sangre.
ConclusionesLa solicitud de concentrados eritrocitarios fue excesiva en relación a la demanda real requerida; esto representa una inadecuada solicitud de sangre y costos elevados tanto para el banco de sangre como para el sistema de salud. Es necesario promover estrategias a través del Comité de Medicina Transfusional institucional.
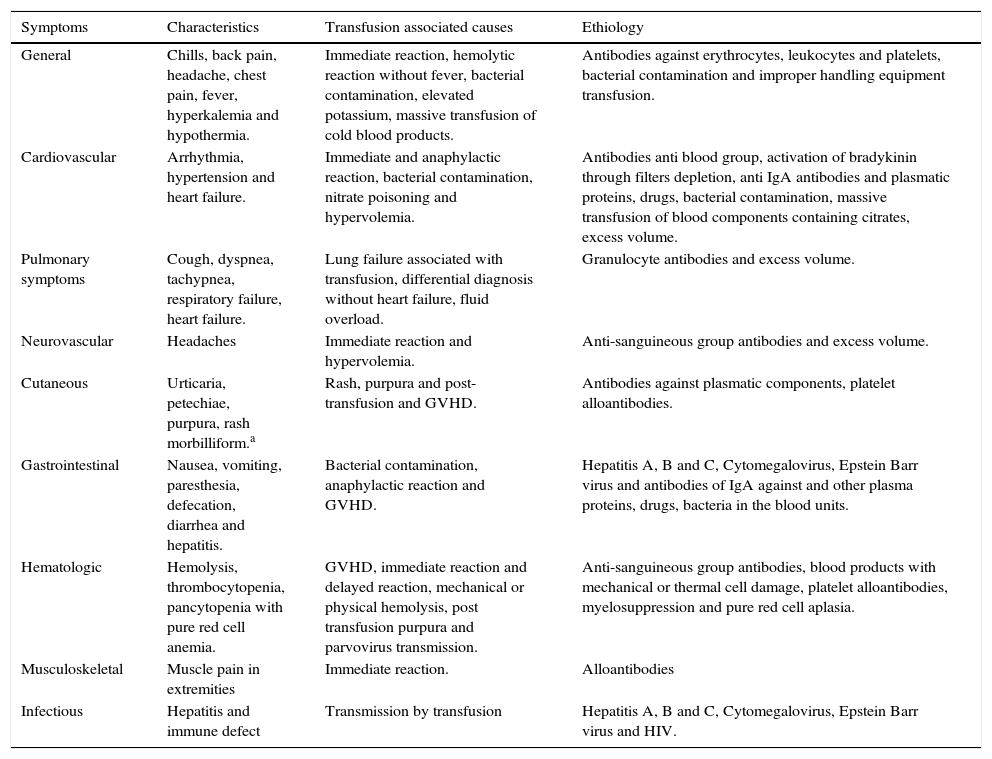
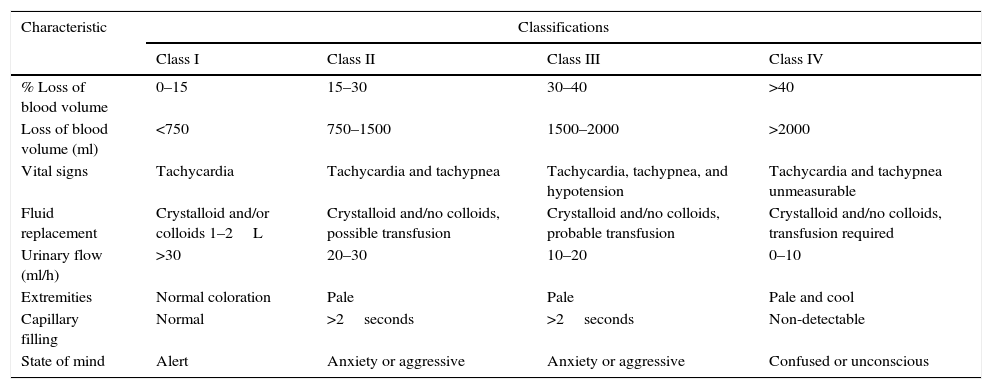
Blood transfusion is a therapeutic method that started on the sixteenth century, initially based on magic and mysticism until the appearance of the rigorous application of the scientific method.1 In the specific case of a surgical patient, the RBC is probably the blood component more frequently transfused during the perioperative event.2 Bleeding is one of the risks present during the surgical procedure. It can occur during any type of surgery, scheduled or emergency, and no surgical specialty is exempt from this risk. It is important to emphasize the risk-benefit evaluation when transfusing blood, it is alarming that up to 74% of unnecessary red cell transfusions concentrates are reported.3 Bleeding may constitute by itself the cause for a patient to enter the operating room. This complication can cause serious repercussions on the health of patients, even death. The rational request of RBC to the blood bank is extremely important, they should not be requested to only comply a bureaucratic process, it cannot follow a simple protocol without proper fundament, RBC are used to replace blood losses and for palliative treatment of certain anemias.4 Every day blood that was routinely requested is returned to the blood bank. It is still graver the fact that blood requested for “just in case” use and that is not transfused must be thrown out since it may not have been in optimal temperature conditions. Routinely in the operating room, RBC should be stored at room temperature for up to 4h; if they are required for a longer period of time, they must be kept between 2 and 6°C.4,5 The purpose of knowing whether or not the blood was properly conserved is a problem not regarding improper management but the identification of needs to build or develop strategies in order to improve the correct use of blood. It is very important to emphasize the risk-benefit assessment for blood transfusion and its components and properly select the patient to be transfused with precise indications and number of units to be transfused.6 A transfusion reaction refers to the adverse effects or an abnormal response that a patient develops with the administration of blood components; it can be acute if it occurs within 24h, or delayed if it occurs after 24h. Transfusion reactions are classified into two major categories: immunological and non-immunological, both can be immediate or delayed7,8 (Table 1). In the specific case of surgical patients, transfusion risks include: increase in the frequency of postoperative infections, respiratory distress syndrome due to volume overload and graft versus host disease (GVDH), this impacts the patients morbidity and mortality without doubt.9 The use of the ratio “10:30” for hemoglobin and hematocrit, respectively as indicative of the need for transfusion must be avoided.10 This was referred in various publications as a trigger for hemoglobin values between 7 and 9g/dl, for transfusion of RBC which is no more current11–14; even in young patients without concomitant diseases, the trigger value can be considered up to 6g/dl, and in cases of advanced age (over 70 years) cardiovascular disorders (myocardial ischemia, heart failure, cerebral vascular disease), and in patients with diseases that cause high consumption of oxygen, hemoglobin values of 8–10g/dl are justified.13–15 The indication to transfuse erythrocyte concentrates is responsibility of the physician, and obviously clinical parameters are critical in the decision to perform a transfusion.4,16 (Table 2). It is important to consider that storage time will have important repercussions in the blood; mainly in the intracellular concentration of 2–3 diphosphoglycerate (2,3-DPG) that contributes to the proper function of transfused red blood cells. The 2,3-DPG facilitates the release of oxygen to interact with hemoglobin, the above is observed by diverting the dissociation of the oxygen curve to the right. The decrease in the concentration of 2,3-DPG, decreases the release of oxygen from red blood cells and 2,3-DPG values reach normal levels 24h after transfusion.17 The aim of this study was to determine the number of requests of red cell concentrates and their destination by the different medical specialties of the operating rooms of the General Hospital of Mexico.
Clinical symptoms of post-transfusion reactions.
| Symptoms | Characteristics | Transfusion associated causes | Ethiology |
|---|---|---|---|
| General | Chills, back pain, headache, chest pain, fever, hyperkalemia and hypothermia. | Immediate reaction, hemolytic reaction without fever, bacterial contamination, elevated potassium, massive transfusion of cold blood products. | Antibodies against erythrocytes, leukocytes and platelets, bacterial contamination and improper handling equipment transfusion. |
| Cardiovascular | Arrhythmia, hypertension and heart failure. | Immediate and anaphylactic reaction, bacterial contamination, nitrate poisoning and hypervolemia. | Antibodies anti blood group, activation of bradykinin through filters depletion, anti IgA antibodies and plasmatic proteins, drugs, bacterial contamination, massive transfusion of blood components containing citrates, excess volume. |
| Pulmonary symptoms | Cough, dyspnea, tachypnea, respiratory failure, heart failure. | Lung failure associated with transfusion, differential diagnosis without heart failure, fluid overload. | Granulocyte antibodies and excess volume. |
| Neurovascular | Headaches | Immediate reaction and hypervolemia. | Anti-sanguineous group antibodies and excess volume. |
| Cutaneous | Urticaria, petechiae, purpura, rash morbilliform.a | Rash, purpura and post-transfusion and GVHD. | Antibodies against plasmatic components, platelet alloantibodies. |
| Gastrointestinal | Nausea, vomiting, paresthesia, defecation, diarrhea and hepatitis. | Bacterial contamination, anaphylactic reaction and GVHD. | Hepatitis A, B and C, Cytomegalovirus, Epstein Barr virus and antibodies of IgA against and other plasma proteins, drugs, bacteria in the blood units. |
| Hematologic | Hemolysis, thrombocytopenia, pancytopenia with pure red cell anemia. | GVHD, immediate reaction and delayed reaction, mechanical or physical hemolysis, post transfusion purpura and parvovirus transmission. | Anti-sanguineous group antibodies, blood products with mechanical or thermal cell damage, platelet alloantibodies, myelosuppression and pure red cell aplasia. |
| Musculoskeletal | Muscle pain in extremities | Immediate reaction. | Alloantibodies |
| Infectious | Hepatitis and immune defect | Transmission by transfusion | Hepatitis A, B and C, Cytomegalovirus, Epstein Barr virus and HIV. |
Classification of acute bleeding and recommendations for transfusion of red cell concentrates in adults.
| Characteristic | Classifications | |||
|---|---|---|---|---|
| Class I | Class II | Class III | Class IV | |
| % Loss of blood volume | 0–15 | 15–30 | 30–40 | >40 |
| Loss of blood volume (ml) | <750 | 750–1500 | 1500–2000 | >2000 |
| Vital signs | Tachycardia | Tachycardia and tachypnea | Tachycardia, tachypnea, and hypotension | Tachycardia and tachypnea unmeasurable |
| Fluid replacement | Crystalloid and/or colloids 1–2L | Crystalloid and/no colloids, possible transfusion | Crystalloid and/no colloids, probable transfusion | Crystalloid and/no colloids, transfusion required |
| Urinary flow (ml/h) | >30 | 20–30 | 10–20 | 0–10 |
| Extremities | Normal coloration | Pale | Pale | Pale and cool |
| Capillary filling | Normal | >2seconds | >2seconds | Non-detectable |
| State of mind | Alert | Anxiety or aggressive | Anxiety or aggressive | Confused or unconscious |
A retrospective study of medical and surgical notes, anesthesia, nursing sheets and laboratory results of surgical patients for which units were requested from the Blood Bank was performed. Also requests cases of programmed surgery and urgency of each specialty of the General Hospital of Mexico were analyzed over a period of 6 months. The number of red cell concentrates requested and transfused and non-transfused was determined. Data was collected in order to integrate a database in Microsoft Office Excel 2007.
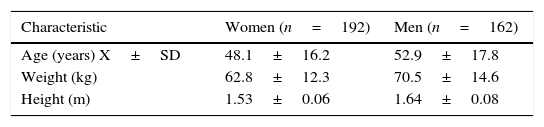
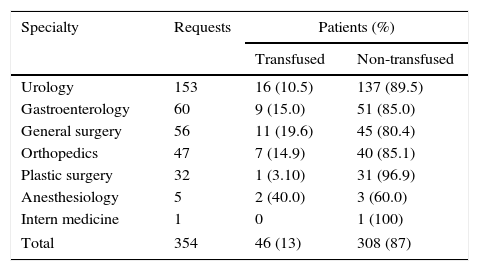
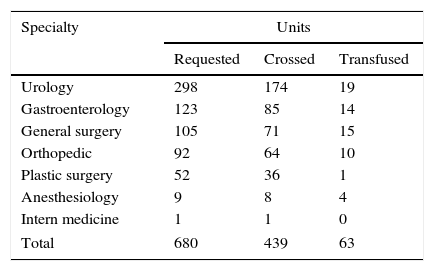
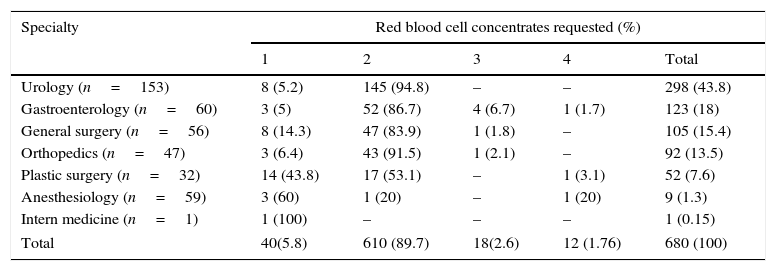
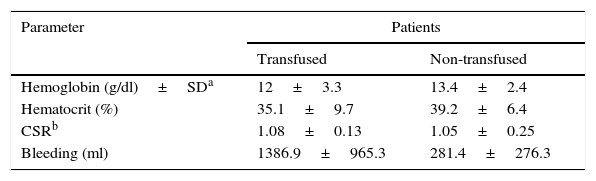
Results354 red cell concentrates requests were analyzed, form these 192 (54.2%) were women and 162 men (45.8%). The demographic characteristics (age, weight and height) are shown in Table 3. From the 354 total requests, 339 (95.8%) were for programmed surgery and 15 (4.2%) for emergency surgery. 184 (54.3%) women and 155 (45.7%) men of programmed surgery were identified. Transfusion of at least one blood unit was performed in 46 (13%) cases and 308 (87%) cases were not transfused (Fig. 1). An average of between one and four blood units were requested, with a total of 680 from which only 439 were crossmatched and of these only 63 were transfused. Table 4 shows the total number of crossmatched and transfused units by medical specialty. In 305 (86.2%) two units were requested, one unit in 40 (11.3%) cases, in 6 (1.7%) three units, and 3 (0.8%) with four units. The number of units requested by specialty and request by unit are shown in Tables 5 and 6. Of the 308 requests canceled, 38 (12.3%) cases were due to the surgical procedure and in 270 (87.7%) cases were not required during surgery. In 38 cases the surgical procedure was not performed and 76 units were requested from which 46 were crossmatched. Hemoglobin, hematocrit, Coagulation Standardized Ratio (CSR) and bleeding data of transfused and not transfused patients are presented in Table 7. From the 308 requested not transfused units, bleeding was only referred in 261 and in 7 cases was reported as “minimal bleeding” and in 2 was not reported. From the 46 transfused cases, 21 (45.7%) were women and 25 (54.3%) men. In 37 (80.4%) cases was an ordinary procedure performed, and in 9 (19.6%) of urgency. From these 46 cases, 40 were transfused during the surgery and 4 after surgery. From the two transfused cases, one of orthopedics the surgery was canceled but the patient was transfused anyway with a unit of blood and other corresponding to General Surgery was also canceled, an endoscopy was realized and was transfused with one blood unit. In 30 (65.2%) cases one blood unit was transfused; in 15 (32.6%) cases 2 units and in one case (2.2%) 3.
Transfused and non-transfused patients by medical specialty.
| Specialty | Requests | Patients (%) | |
|---|---|---|---|
| Transfused | Non-transfused | ||
| Urology | 153 | 16 (10.5) | 137 (89.5) |
| Gastroenterology | 60 | 9 (15.0) | 51 (85.0) |
| General surgery | 56 | 11 (19.6) | 45 (80.4) |
| Orthopedics | 47 | 7 (14.9) | 40 (85.1) |
| Plastic surgery | 32 | 1 (3.10) | 31 (96.9) |
| Anesthesiology | 5 | 2 (40.0) | 3 (60.0) |
| Intern medicine | 1 | 0 | 1 (100) |
| Total | 354 | 46 (13) | 308 (87) |
Units of red blood cell concentrates, requested and transfused crossed by medical specialty.
| Specialty | Units | ||
|---|---|---|---|
| Requested | Crossed | Transfused | |
| Urology | 298 | 174 | 19 |
| Gastroenterology | 123 | 85 | 14 |
| General surgery | 105 | 71 | 15 |
| Orthopedic | 92 | 64 | 10 |
| Plastic surgery | 52 | 36 | 1 |
| Anesthesiology | 9 | 8 | 4 |
| Intern medicine | 1 | 1 | 0 |
| Total | 680 | 439 | 63 |
Total units of red blood cell concentrates requested by specialty.
| Specialty | Red blood cell concentrates requested (%) | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | |
| Urology (n=153) | 8 (5.2) | 145 (94.8) | – | – | 298 (43.8) |
| Gastroenterology (n=60) | 3 (5) | 52 (86.7) | 4 (6.7) | 1 (1.7) | 123 (18) |
| General surgery (n=56) | 8 (14.3) | 47 (83.9) | 1 (1.8) | – | 105 (15.4) |
| Orthopedics (n=47) | 3 (6.4) | 43 (91.5) | 1 (2.1) | – | 92 (13.5) |
| Plastic surgery (n=32) | 14 (43.8) | 17 (53.1) | – | 1 (3.1) | 52 (7.6) |
| Anesthesiology (n=59) | 3 (60) | 1 (20) | – | 1 (20) | 9 (1.3) |
| Intern medicine (n=1) | 1 (100) | – | – | – | 1 (0.15) |
| Total | 40(5.8) | 610 (89.7) | 18(2.6) | 12 (1.76) | 680 (100) |
Hemoglobin, hematocrit, standardized international coagulation index, bleeding in patients transfused and non-transfused.
This study shows that most of the RBC units requested were not transfused (90.73%), the number of transfusions was low (9.26%), indicating that requests are not entirely justified, since the resource was not used. Of the 46 cases transfused, (63) 95.8% were for programmed and 4.2% for emergency surgery. Routinely, most requests include two units of blood, of which the blood bank performs mainly one crossmatch unit. Of the 680 units requested, 439 were crossed (64.6%), from these 14.3% (63) were transfused, while 376 (85.6%) were not used. It is important to note that blood units are transferred from the blood bank to the operating room and are not under proper storage conditions (temperatures 2–6°C), it is necessary to give them final destination due to the hemolysis process.5 The mean hemoglobin observed in the transfused cases was 12g/dl, trans-surgical bleeding was probably a decisive element to perform transfusion. The trans-surgical bleeding of >600ml in the transfused cases, justifies the use of transfusion. In cases where the bleeding was less than 600ml, the mean hemoglobin was 9.5±1.7sg/dl. The CSR values in the transfused cases were between 0.9 and 1.1 (normal range), the alteration of this parameter does not justify the transfusion. This study of the blood use during surgical procedures showed that the request for blood units does not have well-founded indications since blood units requested were not needed. Probably other health institutions have this same problem when requesting blood components.
ConclusionThe number of requests of non-transfused blood units is high, resulting in unwarranted expense, this situation was observed more frequently in programmed surgery of the specialties of Urology, Gastroenterology, General Surgery, Plastic Surgery and Orthopedics. All patients transfused were justified because of bleeding and/or anemia prior to the surgical event. According to the results, a specific document for the request of blood and blood components could be developed, where indication of the blood component, transfusion and postransfusional practices, clinical information and laboratory results should be included and preserved in the clinical history, so that transfusion practices can be followed. The medical staff should be sensitized on the rational use of this valuable resource. This work contributes to the situational analysis and knowledge of blood needs for surgical events by specialty, and also represents an opportunity field for the assessment of risks and benefits as well as costs considerations in the use of blood, in order to generate intern policies in health institutions through the Transfusion Medicine Committees for the rational use of blood.18,19
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.