Sentinel lymph node biopsy (SLNB) usefulness in breast carcinoma N+ converted to N0 after neoadjuvant chemotherapy (NC).
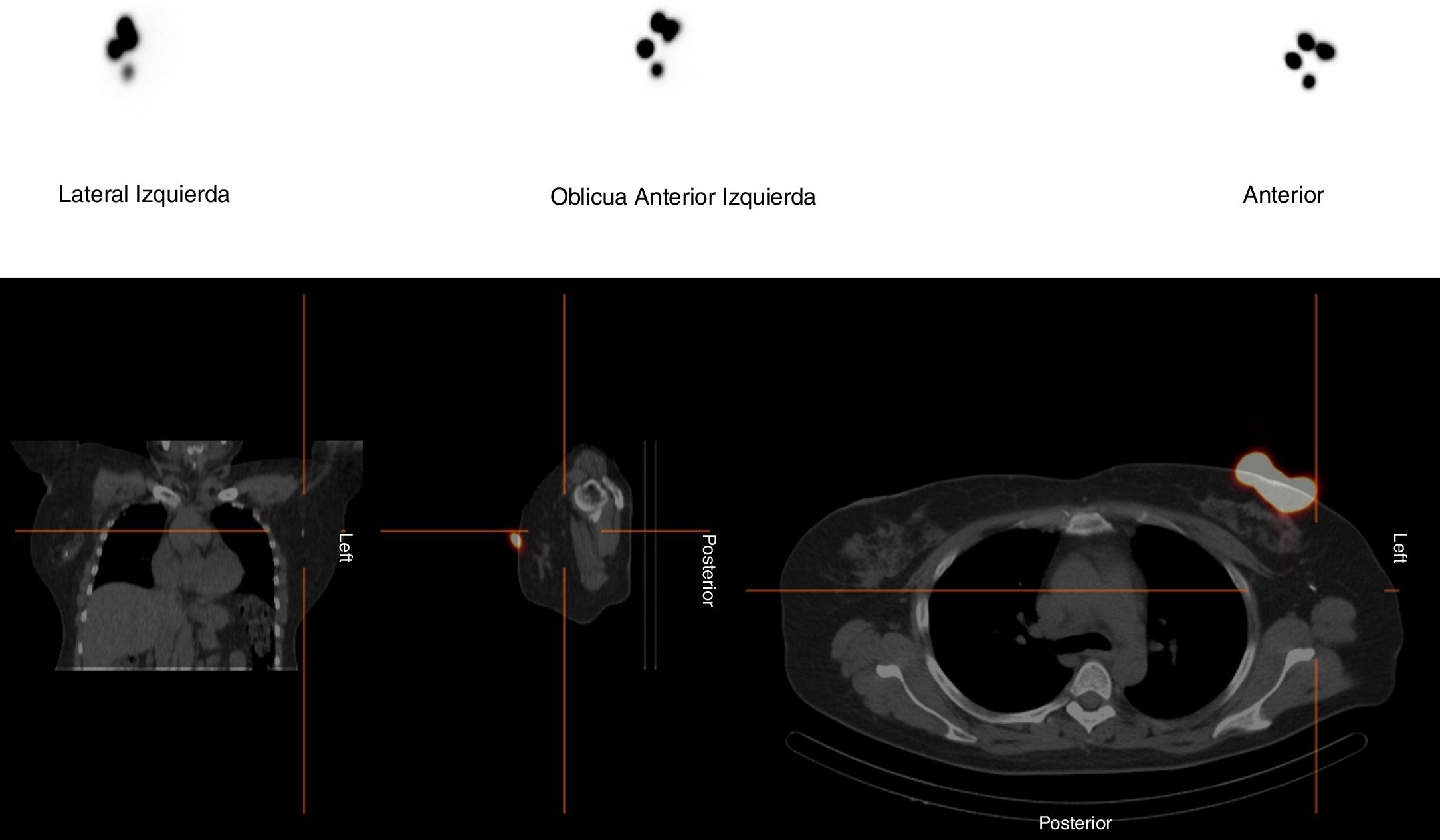
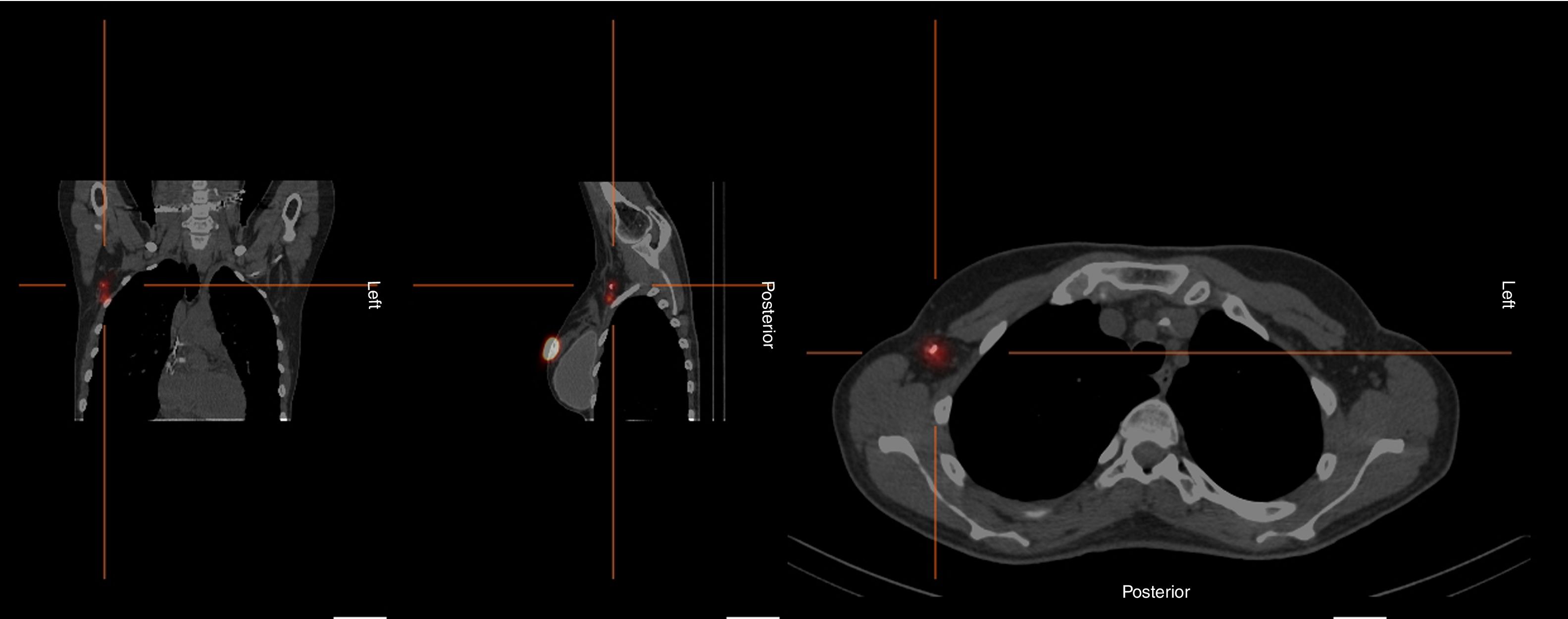
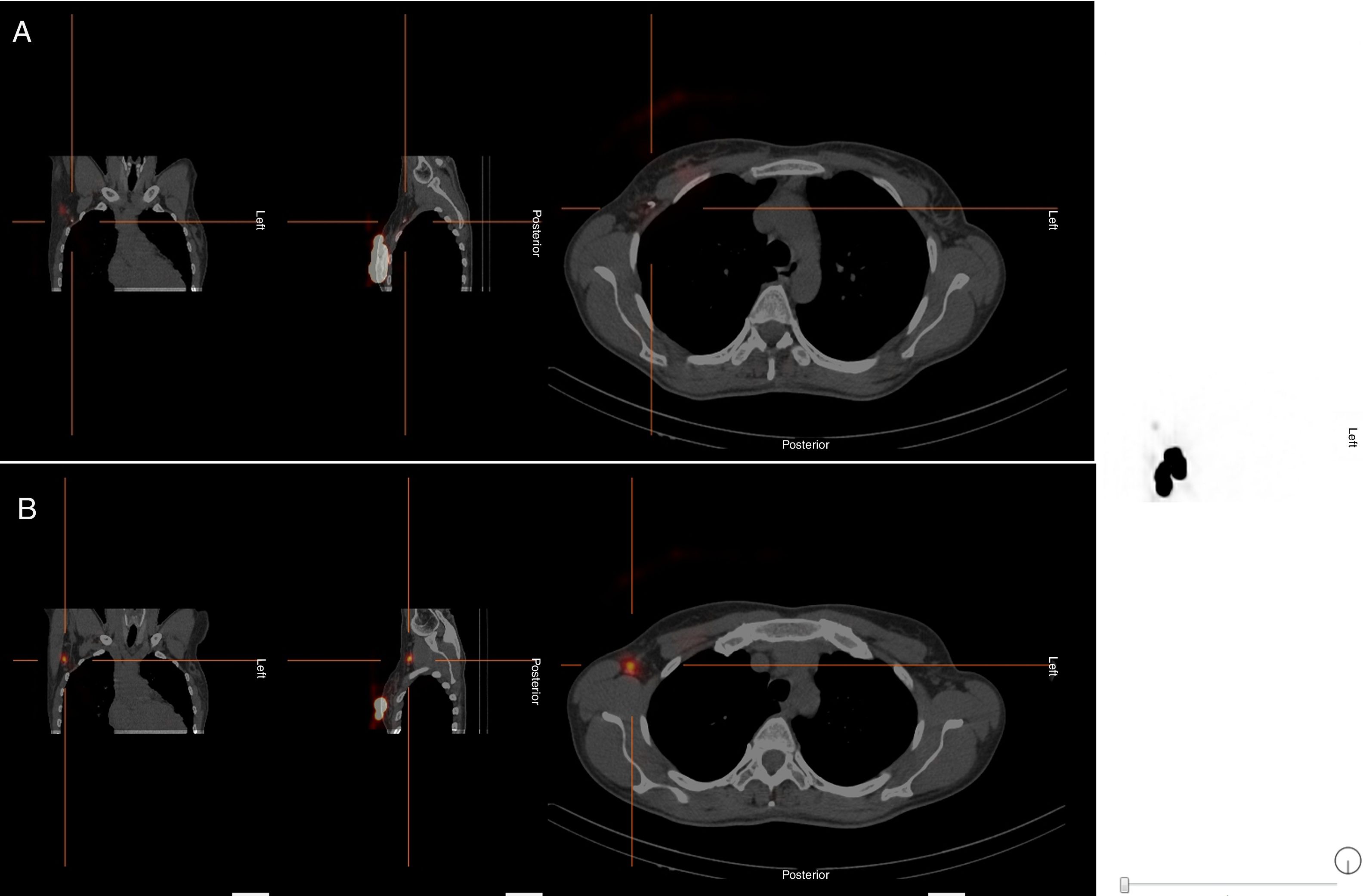
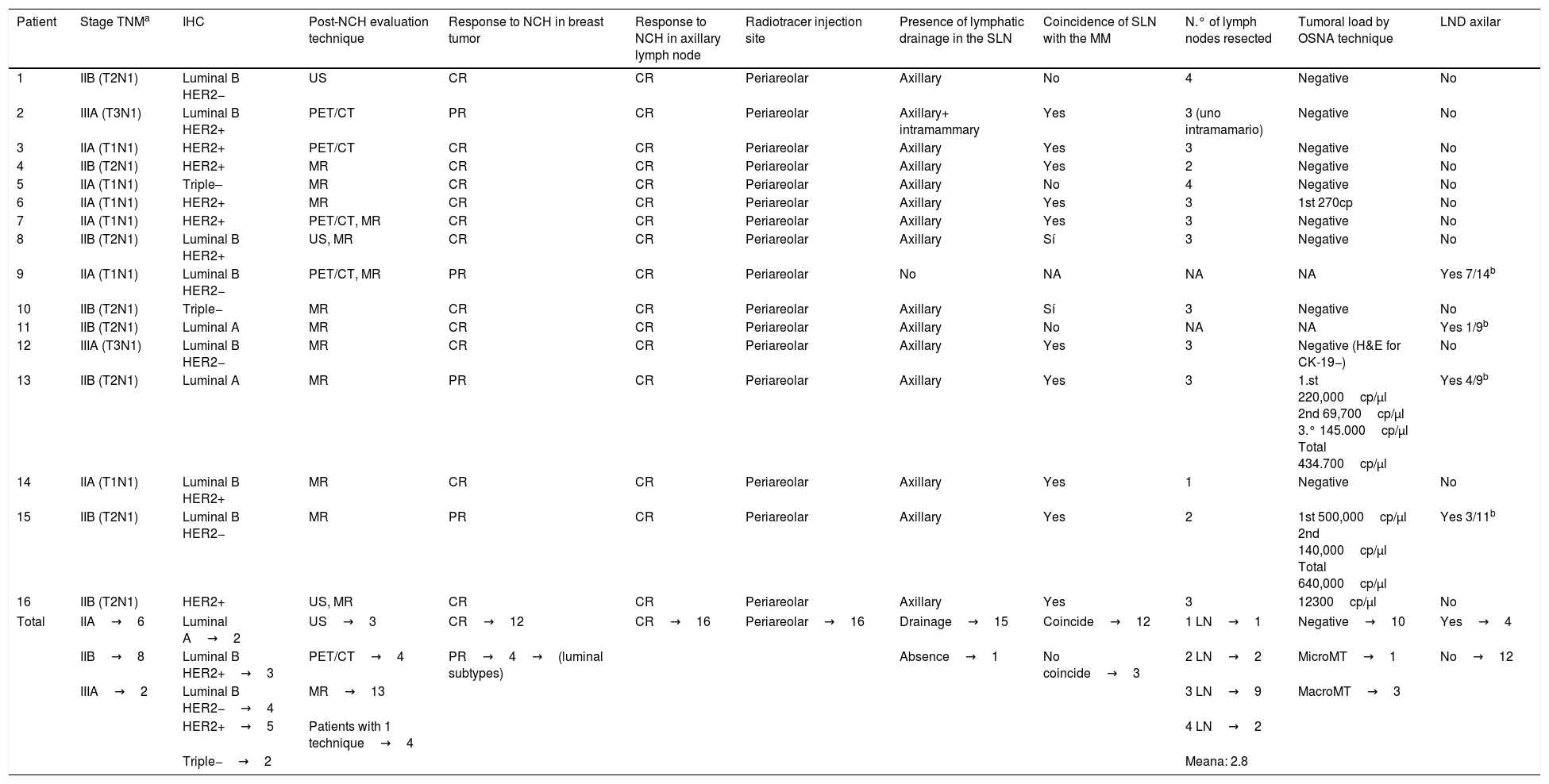
Material and methodsDescriptive study including 16 females with infiltrating carcinoma with lymphatic metastasis confirmed by biopsy, leaving a metallic marker (MM) in pathological lymph nodes (LN). All patients underwent NC reaching a complete radiological response in LN. Lymphoscintigraphy was performed after 99mTc nanocoloid injection, obtaining planar images and SPECT/CT. Lymphatic drainage and concordance of sentinel node (SN) with MM was analyzed.
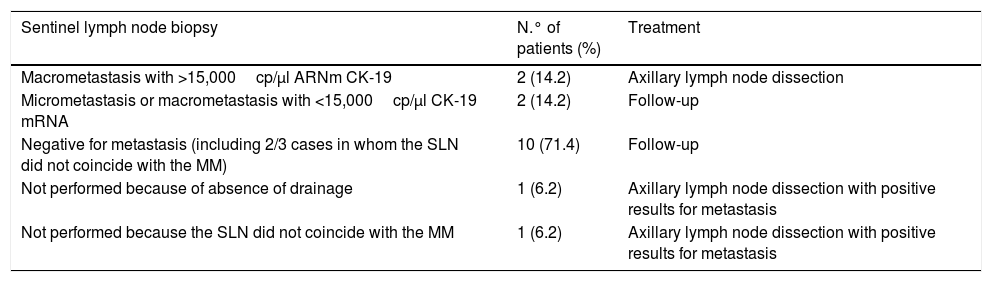
ResultsSN was visualized in lymphoscintigraphy in 93.7% of cases. The SN coincided with the MM in 12/15 cases on SPECT/CT. The SLNB technique was completed on 14/16 patients, intraoperatively locating the GC in all of them. The SN was negative in 10 cases, 3 cases presented macrometastases and 1 micrometastases. Axillary lymphadenectomy (AL) was performed in a case of macrometastasis with >15,000cp/μARNm CK-19, absence of drainage and in one case that showed no coincidence with the MM due different Berg's level location. These last two cases presented lymph node metastasis. In the other two cases with not coincidence between the SN and the MM, a total of 4 lymph nodes were removed, showing no evidence of metastasis. Patients without AL were followed up for an average of 10 months (range 6–17), with no evidence of lymph node involvement.
ConclusionSLNB in breast cancer with conversion into N0 after neoadjuvant treatment is a technique with good results and a low false negative rate.
Valorar la utilidad de la biopsia selectiva del ganglio centinela (BSGC) en pacientes con carcinoma de mama N+ convertidas a N0 tras recibir quimioterapia neoadyuvante.
Material y métodosAnálisis descriptivo incluyendo 16 mujeres diagnosticadas de carcinoma infiltrante de mama con metástasis linfáticas confirmadas por biopsia y portadoras de marcador metálico (MM) en el ganglio patológico. Recibieron quimioterapia neoadyuvante con respuesta radiológica completa ganglionar. Se realizó linfogammagrafía tras inyección de 99mTc-nanocoloides, obteniéndose imágenes planares y SPECT/TC, analizando el drenaje linfático y la concordancia del ganglio centinela (GC) con el MM.
ResultadosEl GC se visualizó en la linfogammagrafía en el 93,7% de los casos. El GC coincidió con el MM en 12/15 en la SPECT/TC. Se completó la técnica de BSGC en 14/16, localizando intraoperatoriamente el GC en todas ellas. El GC fue negativo en 10 pacientes, 3 presentaron macrometástasis y una micrometástasis, realizándose linfadenectomía axilar a los casos con macrometástasis>15.000cp/μARNm CK-19, ausencia de drenaje y uno de los no coincidentes con el MM por encontrarse en diferentes niveles de Berg. Estos 2 últimos con resultado positivo para metástasis. En los otros casos de no coincidencia con el MM se extirparon en total 4 ganglios linfáticos, sin evidencia de metástasis. A las pacientes que no se les practicó linfadenectomía axilar se les hizo seguimiento medio de 10 meses (rango 6-17), sin evidencia de afectación ganglionar.
ConclusionesLa BSGC en el cáncer de mama con conversión a N0 post-neoadyuvancia presenta buenos resultados y una baja tasa de falsos negativos.
Article
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)