Spinopelvic dissociation is an uncommon injury, but, at the same time, very serious, since it can associate important complications with high morbidity and mortality. Its low frequency means that the experience of the specialists who have to deal with it is often very limited.
ObjectiveTo analyze the treatment indications based in classifications and surgery techniques.
MethodA search for scientific articles from high-impact journals was performed through international databases, such as Pubmed, Cochrane Library, Scopus, Science Direct and OVID.
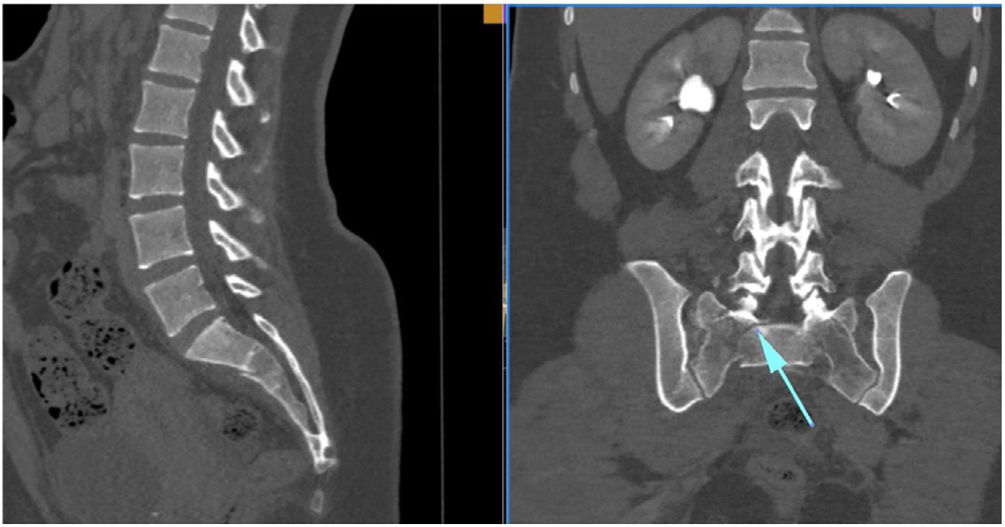
ConclusionsThe management of the injury we are analyzing represents a challenge. The diagnosis is carried out through a meticulous anamnesis and physical examination, supported by imaging tests, where tomography acquires special relevance. The treatment is fundamentally surgical, reserved the conservative option for a few cases. Triangular fixation is nowadays considered the treatment of choice.
La disociación espinopélvica es una lesión muy poco frecuente, pero también muy grave, ya que puede asociar importantes complicaciones con una elevada morbimortalidad. Su baja frecuencia provoca que la experiencia de los especialistas que tienen que hacerle frente, es a menudo muy limitada.
ObjetivoAnalizar las indicaciones de tratamiento basadas en las clasificaciones más empleadas y los detalles técnicos quirúrgicos de esta patología.
MétodoSe realizó una búsqueda de artículos científicos en revistas de impacto, a través de bases de datos internacionales, como PubMed, Cochrane Library, Scopus, ScienceDirect y OVID.
ConclusionesEl manejo de la disociación espinopélvica representa un reto. El diagnóstico se lleva a cabo a través de una minuciosa anamnesis y exploración física, apoyado en pruebas de imagen, fundamentalmente la tomografía. El tratamiento suele ser quirúrgico, reservando la opción conservadora para unos pocos supuestos. La fijación triangular se considera hoy día su tratamiento de elección.
Spinopelvic dissociation (SPD) is an injury characterised anatomically by discontinuity between the spine and pelvis.1 It is caused by a horizontal fracture of the sacrum usually associated with a longitudinal and bilateral fracture line. In 1985, Roy Camille described this injury as the “suicidal jumper's fracture” due to a strong association with this mechanism of injury. It is a rare injury that can occur in 2%–3% of transverse sacral fractures and in 3% of sacral fractures that combine injuries of the pelvic ring.2 It generally occurs in high-energy mechanisms, such as falls from height or motor vehicle accidents, although it can also occur after a fall from a very low height in elderly patients with osteoporotic bones.3 Both groups of fractures have increased in incidence in recent decades,4,5 partly attributable to the aging of the general population and also because they are being diagnosed more often thanks to the increasing use of computed tomography (CT) for these traumas. These injuries are associated with a high incidence of neurological deficits, such as paraesthesia of the L5 and S1 territories, bowel or bladder dysfunction, and even complete cauda equina syndromes. The heterogeneity of these fractures together with their low incidence means that the experience of specialists may be limited, which in turn may lead to inadequate diagnosis and treatment. For this article we conducted an exhaustive systematic literature review of the articles published in English and Spanish in order to list the evidence over the last 8 years and address the current debate.
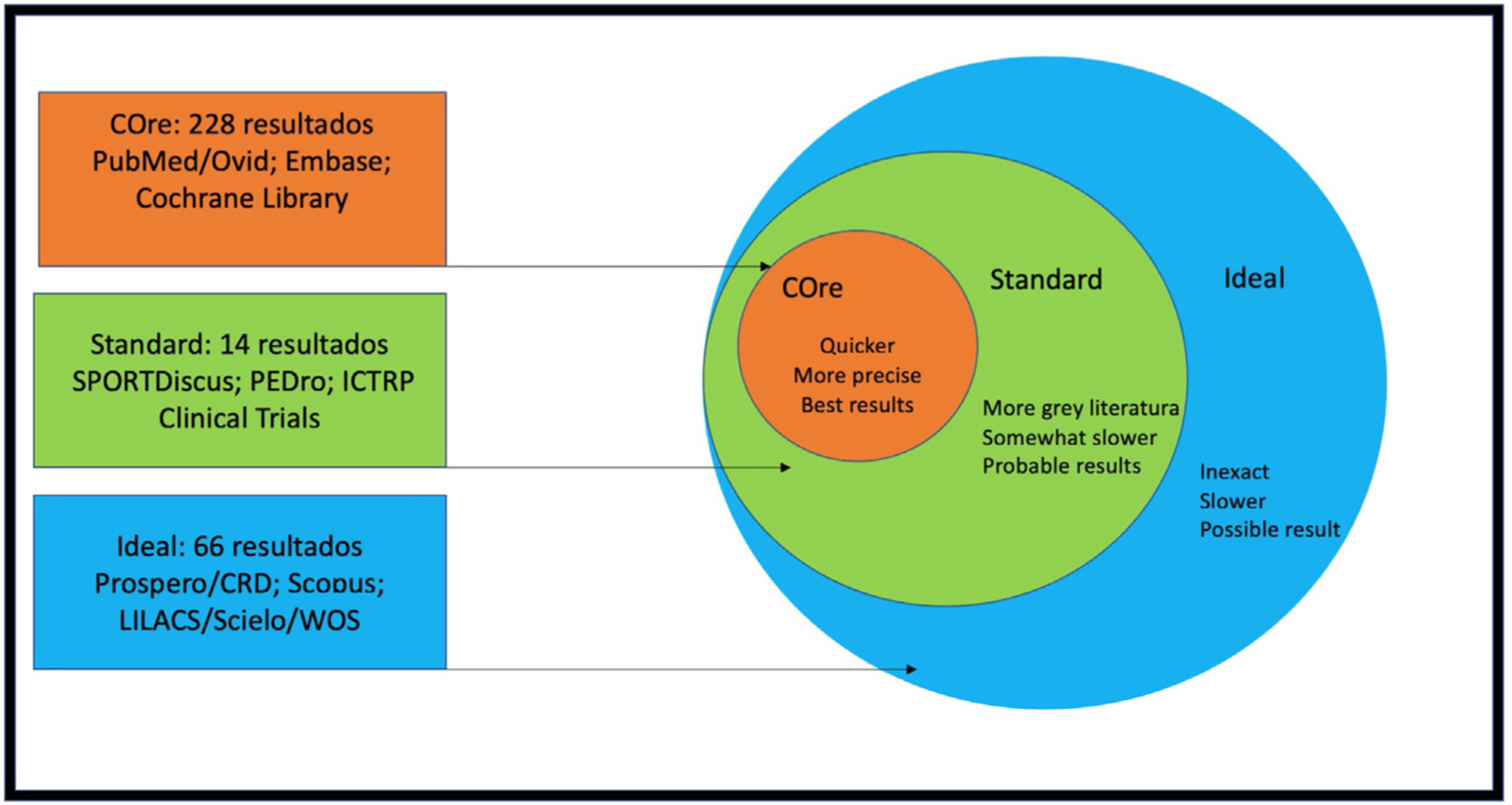
MethodsAll databases considered for the literature search were accessible through our online corporate library, the Virtual Library of the Andalusian Public Health System (BVSSPA). Articles were selected using the COre, Standard, Ideal (COSI) protocol (Fig. 1). We examined the MEDLINE (PubMed)/Ovid-MEDLINE Embase/SPORTDiscus/Cochrane Library/Web of Science/Scielo/Current Contents/PEDro/CINAHL (Nursing Ovid)/Google Scholar databases.
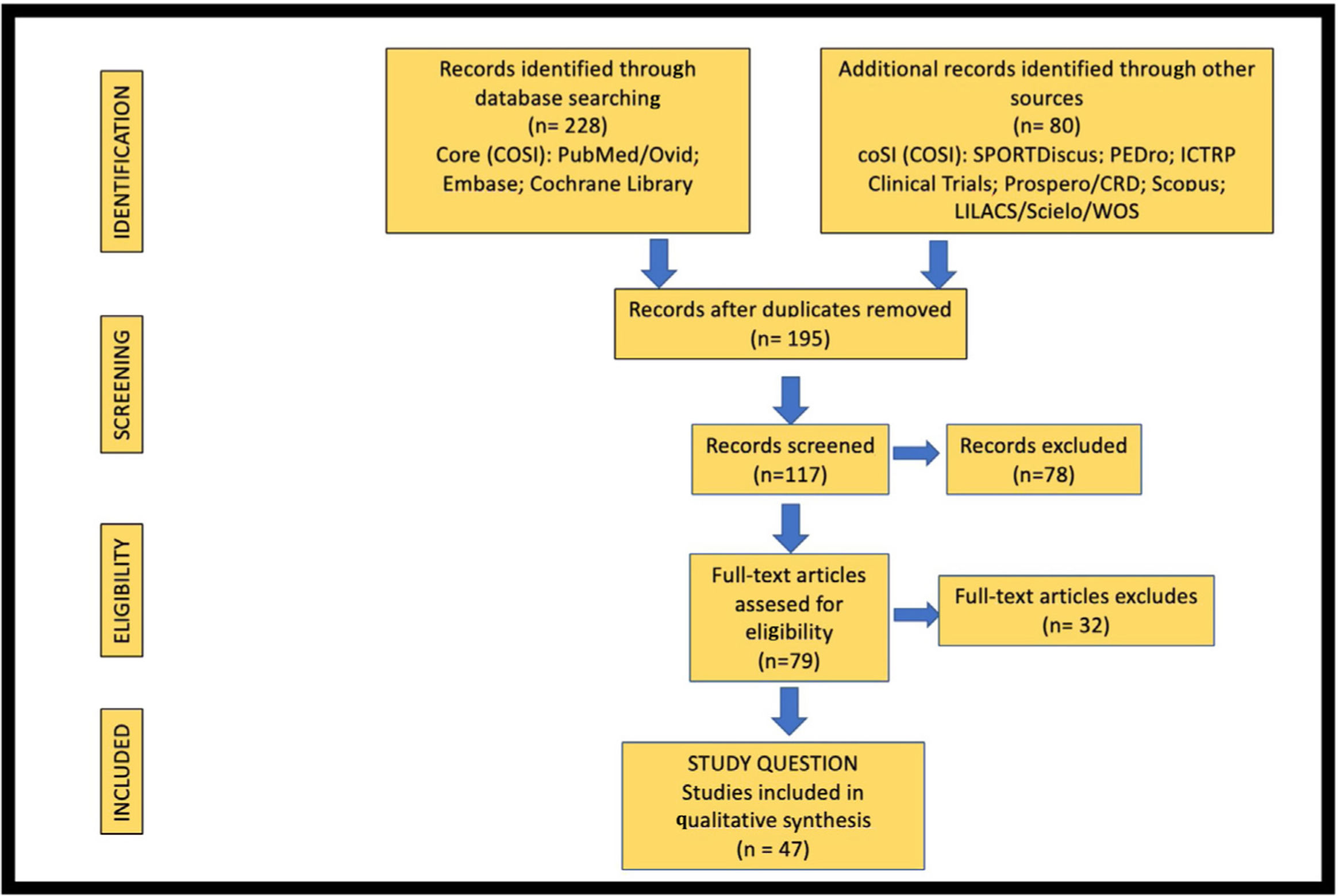
We conducted literature searches using the Patient, Intervention, Comparison, Outcome (PICO) template. Both free language (titles and abstracts) and controlled language (MeSH, Entrez, etc.) were used. Articles published in the last 8 years in English and Spanish were included. Articles consisting only of abstracts, conference presentations, commentaries, letters to the editor, and papers on single isolated clinical cases were excluded. Articles written by the same authors were meticulously compared to rule out duplicate studies. All queries and search steps were performed with Boolean operators (AND, OR, NOT, NEAR, ADJ, etc.) using the terms: “spinopelvic”, “sacral fractures” and “fixation”. For each question, papers were retrieved and selected according to the title and abstract in each case. We then conducted a manual search for relevant citations within the selected full texts. Data storage, elimination of duplicates and final editing was performed using the EndNote reference manager and the Google Drive platform. Before performing the review, we created a checklist for data extraction. A flow chart of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)6 was followed for the selection of studies and the number of references was adjusted according to editorial guidelines (Fig. 2).
ResultsA total of 308 articles were initially obtained, among which there were 113 duplicates that were eliminated, leaving a total of 195 papers. After applying secondary screening according to the inclusion and exclusion criteria as well as access to full texts and editorial standards, the final result was an inclusion of 47 papers.
The total number of references obtained included 2 studies with level of evidence I, 8 with level of evidence II, and 8 with level of evidence III. The remaining studies included in the analysis had a level of evidence of IV-V, the latter being the largest group. 2020 was the year that included the most papers on this subject, with only 3 of a total of 12 papers with level I–II evidence.
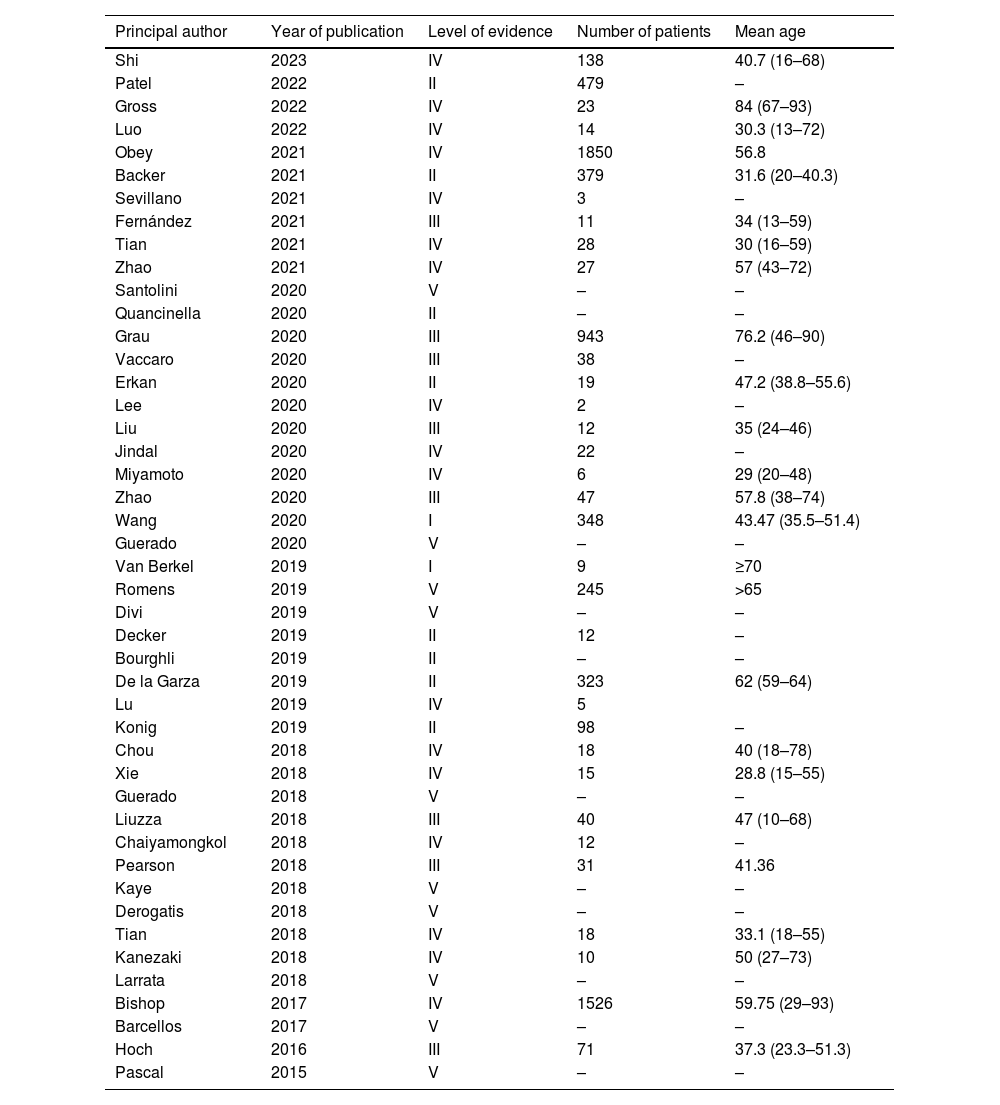
The overall number of patients included in the studies was 6768, a paper published in 2021 included the most patients at 1850. The mean age of the patients studied was 47 years, the youngest being 10 years old and the oldest 93 years old. Only 12 papers included patients aged ≥65 years (Table 1).
Summary of the studies included in the systematic review.
| Principal author | Year of publication | Level of evidence | Number of patients | Mean age |
|---|---|---|---|---|
| Shi | 2023 | IV | 138 | 40.7 (16–68) |
| Patel | 2022 | II | 479 | – |
| Gross | 2022 | IV | 23 | 84 (67–93) |
| Luo | 2022 | IV | 14 | 30.3 (13–72) |
| Obey | 2021 | IV | 1850 | 56.8 |
| Backer | 2021 | II | 379 | 31.6 (20–40.3) |
| Sevillano | 2021 | IV | 3 | – |
| Fernández | 2021 | III | 11 | 34 (13–59) |
| Tian | 2021 | IV | 28 | 30 (16–59) |
| Zhao | 2021 | IV | 27 | 57 (43–72) |
| Santolini | 2020 | V | – | – |
| Quancinella | 2020 | II | – | – |
| Grau | 2020 | III | 943 | 76.2 (46–90) |
| Vaccaro | 2020 | III | 38 | – |
| Erkan | 2020 | II | 19 | 47.2 (38.8–55.6) |
| Lee | 2020 | IV | 2 | – |
| Liu | 2020 | III | 12 | 35 (24–46) |
| Jindal | 2020 | IV | 22 | – |
| Miyamoto | 2020 | IV | 6 | 29 (20–48) |
| Zhao | 2020 | III | 47 | 57.8 (38–74) |
| Wang | 2020 | I | 348 | 43.47 (35.5–51.4) |
| Guerado | 2020 | V | – | – |
| Van Berkel | 2019 | I | 9 | ≥70 |
| Romens | 2019 | V | 245 | >65 |
| Divi | 2019 | V | – | – |
| Decker | 2019 | II | 12 | – |
| Bourghli | 2019 | II | – | – |
| De la Garza | 2019 | II | 323 | 62 (59–64) |
| Lu | 2019 | IV | 5 | |
| Konig | 2019 | II | 98 | – |
| Chou | 2018 | IV | 18 | 40 (18–78) |
| Xie | 2018 | IV | 15 | 28.8 (15–55) |
| Guerado | 2018 | V | – | – |
| Liuzza | 2018 | III | 40 | 47 (10–68) |
| Chaiyamongkol | 2018 | IV | 12 | – |
| Pearson | 2018 | III | 31 | 41.36 |
| Kaye | 2018 | V | – | – |
| Derogatis | 2018 | V | – | – |
| Tian | 2018 | IV | 18 | 33.1 (18–55) |
| Kanezaki | 2018 | IV | 10 | 50 (27–73) |
| Larrata | 2018 | V | – | – |
| Bishop | 2017 | IV | 1526 | 59.75 (29–93) |
| Barcellos | 2017 | V | – | – |
| Hoch | 2016 | III | 71 | 37.3 (23.3–51.3) |
| Pascal | 2015 | V | – | – |
The most common treatment was surgical, conservative treatment being found in 6 of the studies. The surgical technique of choice is spinopelvic triangular fixation recommended in 28 studies, and isolated pelvic fixation was used in 6 of the included papers.
Mechanism of injury and explorationThe sacrum is a large triangular bone that acts as a link between the spine and the pelvis. It plays a major role in the transmission of loads from the axial skeleton to the pelvic ring, of which it is a part, and in turn helps protect important surrounding structures. Therefore, an injury at this level may be associated with secondary vascular, neurological, or visceral injuries and, at the same time, alter the sufferer's ability to walk. SPD occurs after a fracture of the sacrum combining a longitudinal and a transverse line, with a bimodal presentation, in young patients after high-energy mechanisms7 and in older patients after banal trauma, forming part of the so-called fragility fractures of the pelvis. The presence of sacral dysmorphism appears to be a protective factor against the occurrence of SPD in high-energy axial trauma.8
In cases of non-osteoporotic fractures, because they are associated with high-energy mechanisms or in the context of a polytraumatised patient, it is essential to scrupulously follow the Advanced Trauma Life Support (ATLS) guidelines, paying attention to injuries that could have a fatal outcome, followed by a meticulous and serial neurological examination so that no sign of possible neurological injury goes unnoticed, including examination of the lumbosacral reflexes.9 The American Spinal Injury Classification (ASIA) is very useful in staging these patients. The association of neurological lesions in these injuries is high; in a 2021 meta-analysis it was stated that neurological deficits were present in up to 68.1% of cases, of which 65.1% improved after surgical treatment.10 When the fracture presents a kyphotic deformity of 20° or more, there is a high risk of neurological injury.10 The typical presentation of neurological injuries may resemble cauda equina syndrome, especially in the presence of bladder or bowel dysfunction, hypoaesthesia in the territory of the sacral root tributary, or motor deficits in zones corresponding to L5 and S1.
The association with other non-neurological traumatic injuries is high. In 2016, Gupta et al. conducted a retrospective radiological review of patients diagnosed with SPD and found associated spine fractures in 87.5% of cases, lower extremity fractures in 71%, contiguous fractures in the pelvis in 66.7% and visceral injuries in 28.6%. The association with soft tissue injuries, such as Morel-Lavallée injury, is also appreciable and may make management of these patients more complex.
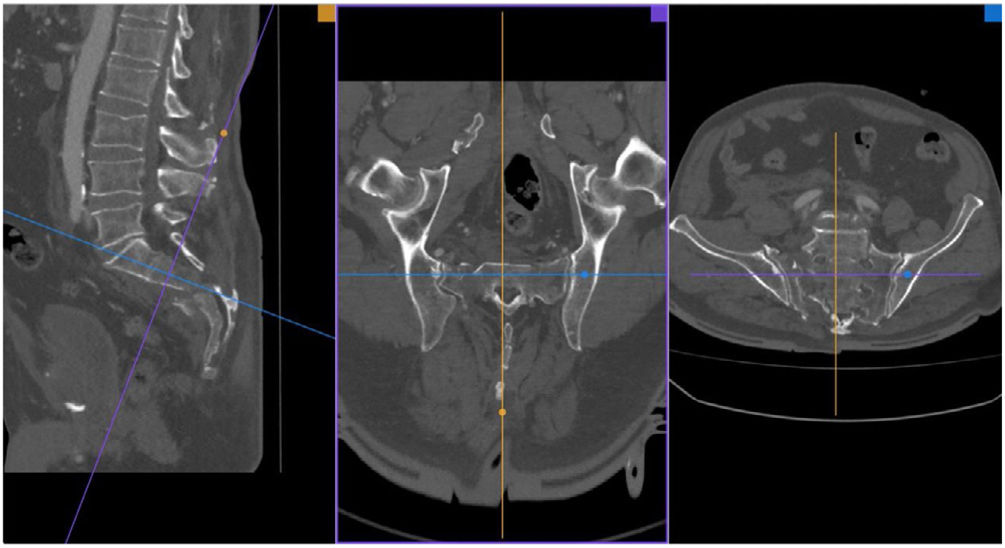
Diagnosis and classificationTaking a history and performing a physical examination should be the first steps guiding diagnosis in these patients, which will require confirmation by imaging tests. Given its low frequency, the diagnosis can be delayed or go unnoticed in ranges from 25% to 70%, depending on the study. By conventional radiology (anteroposterior, lateral, and inlet–outlet views of the pelvis) we can see direct and indirect signs suggestive of a sacral fracture, such as fracture of the transverse processes of L5; or a paradoxical inlet view of the sacrum on an AP view, due to the flexion deformity of the cranial fragment of the sacrum. To diagnose SPD the reference study is the multislice CT of less than 5mm due fundamentally to the multiplanar character of these injuries. The main role of MRI in the diagnosis of these injuries is in a subacute phase, in cases of non-displaced fractures, and in low-energy mechanisms.11 Over recent decades, different classifications have been proposed to help the specialist guide the management of these injuries. The first classifications proposed focused more on morphological aspects and as they progressed more emphasis has been placed on the biomechanical characteristics of these fractures. Initially, according to the mechanism of the fracture, fractures were differentiated as high-energy (young patients) or low-energy (older patients), insufficiency fractures (in frail patients), or stress fractures (in athletes).
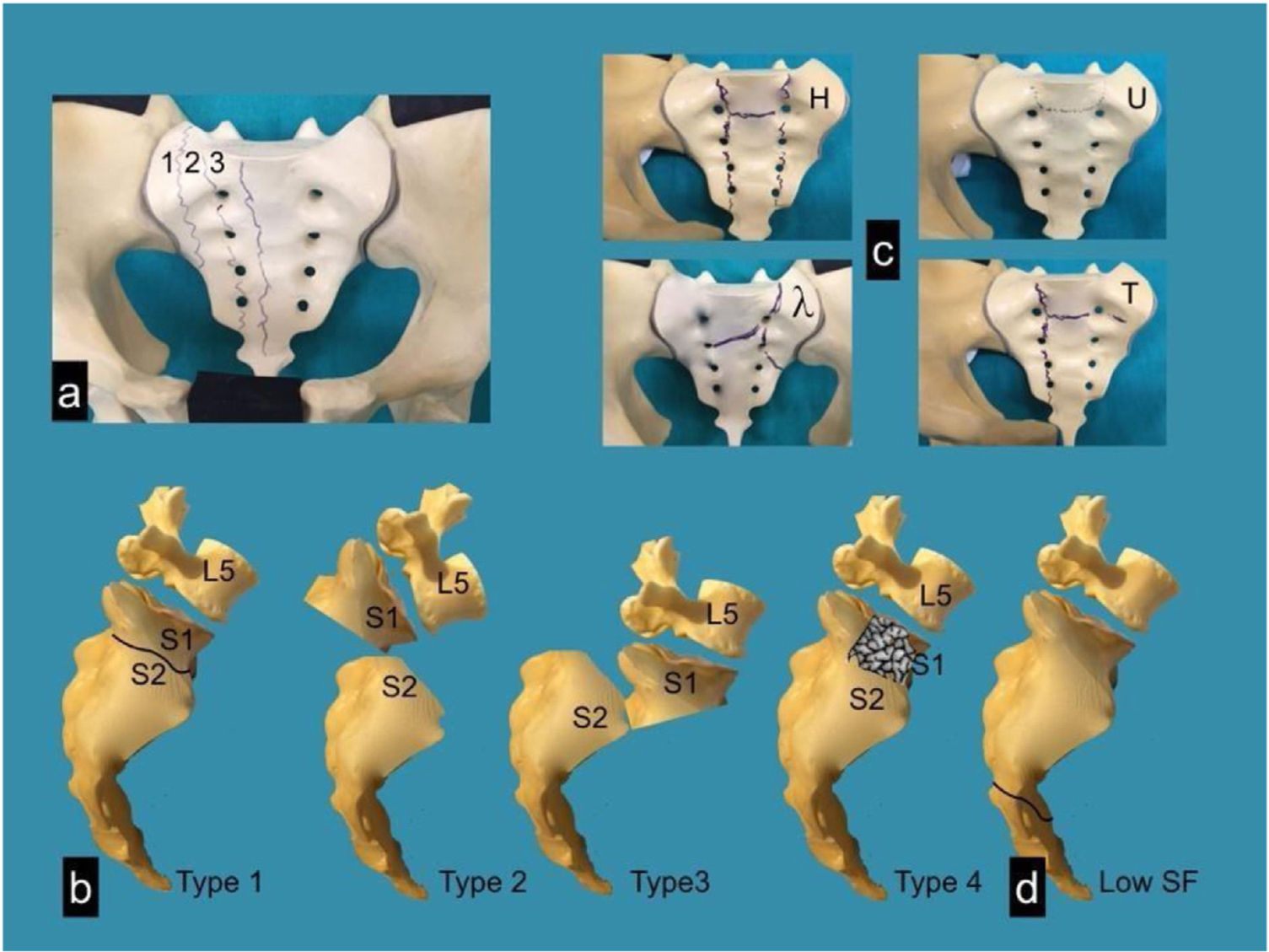
Focusing on the morphology of sacral fractures, Denis et al. proposed a classification according to the location of the fracture line on a coronal plane of the sacrum, thus distinguishing three zones and evaluating the risk of associated neurological injuries.12 Type I is described when the fracture line passes lateral to the foramina and presents a 6% risk of neurological injury, type II occurs when the line passes through the foramina, with an associated neurological risk of 28%, and type III is located medial to the foramina and carries a 56% risk of neurological injury. The Roy Camille classification was postulated later, modified by Strange-Vognsen and Lebech,13 which determines, from a sagittal view, the relationship between the cranial and caudal fragment of the sacrum, establishing 4 types: in type I, only some kyphosis of the cranial fragment is observed; in type II, in addition, there is associated retrolisthesis of this fragment; type III is characterised by complete anterolisthesis of the cranial fragment, and type IV by comminution of the S1 vertebral body.14 Isler presented a classification centred on the relationship of the longitudinal fracture line (Denis II) with the L5–S1 facet joint, establishing three types according to the trajectory lateral (type I), through (type II), or medial to this facet (type III), the latter being unstable by definition.15 This author considered that a bilateral type III fracture would produce an SPD, since spinopelvic stability depends on the posterior lumbosacral ligamentous structures, the integrity of the L5–S1 facet joints, and the level of the transverse fracture16 (Figs. 3 and 4).
At the same time, a description system has also been proposed that combines vertical and horizontal patterns to classify fractures morphologically (H-type, U-type, T-type, and lambda λ-type).17
In recent years, the Sacral Injury Classification System of the AOSpine has been developed to unify the different classification systems for these fractures and thus facilitate communication between specialists for more efficient multidisciplinary management. It is based on three criteria: the morphology of the fracture, integrity of the posterior ligamentous complex, neurological status, and specific clinical modifiers.18 Based on the first criterion, three types of injury are defined: type A injuries are low sacrococcygeal fractures that do not affect posterior pelvic stability; type B injuries are unilateral longitudinal (vertical) sacral fractures that primarily cause posterior pelvic instability but do not affect spinopelvic stability, and are comparable to those described in the Denis classification; type C injuries include unilateral type B injuries with involvement of the L5–S1 facets, bilateral longitudinal (vertical) sacral fractures, and U-fractures, all of which have spinopelvic instability in common (Fig. 5).
Recently, a new classification has been created according to the involvement of the sacroiliac joint. Called 301 Spinopelvic Dissociation Classification (301 SPD Classification), it establishes three groups: (I) trans-sacral fracture without involvement of the sacro-iliac joint (subtypes Ia: without displacement, with or without transverse sacral fracture; Ib: kyphotic deformity of the sacrum with fracture displacement; Ic: flexion deformity with fracture displacement; Id: anterior margin fracture and S1 bilateral superior articular process fracture), (II) Unilateral trans-sacral fracture+contralateral sacroiliac joint injury (IIa: sacroiliac involvement; IIb: trans-ilium sacroiliac involvement), and (III) bilateral sacroiliac joint injury (IIIa: bilateral sacroiliac involvement; IIIb: bilateral trans-sacroiliac and contralateral trans-ilium sacroiliac; IIIc: bilateral trans-ilium sacroiliac involvement).19 As a therapeutic orientation according to the type classified, systematic use of the classification cannot yet be recommended due to the limitations of the study that created it, because only 30 patients were included and the follow-up time was short (mean of 21.9 months).19
Principles of osteosynthesisThe treatment of any fracture should have a clear objective: to restore as far as possible the patient's anatomy through a stable system that preserves blood supply to the fracture site in order to recover functionality with fusion.1 This objective can be achieved by orthopaedic treatment, surgical treatment, or a combination of both. However, whichever therapeutic strategy we choose, to achieve this objective we must comply with certain basic treatment principles7: compression, neutralisation, buttressing, and tension band.
Simple sacral fractures can be treated by applying only the principle of compression, in which two force vectors meet at the fracture site, providing great stability and also inactivating small shear forces. We would apply this principle using partially threaded iliosacral screws, which also provide some neutralisation. However, this principle has three major problems: loss of function after 3–4 weeks, the relative contraindication to use it in fractures that cross the conjunction foramina due to the evident risk of neurological injury if we apply it and, finally, insufficient function when we apply it to complex sacral fractures, that are bilateral, or with SPD due to the increased requirements of shear and rotational forces. In these cases, we should apply the other principles: neutralisation, support, and tension band.
Neutralisation avoids the action of shear and rotational forces greater than those described above. These forces characterise complex sacral fractures, bilateral, comminuted, or with SPD. Applying this principle entails the use of lumbar transpedicular screws and iliac screws in posterolateral location, i.e., they require spinopelvic fixation. The wider the assembly, the greater the neutralisation force, so we must perform fixations more cranial to L5 or use devices that connect the two rods of the spinopelvic fixation, such as the “crosslink”. By performing a spinopelvic fixation, we are also applying the principle of support, by which we maintain the length of the fractured bone, in these cases the length of the sacrum with the lumbar spine.
The tension band principle comprises the absorption of tension by the implant and converting into compressive force at the fracture site on the opposite side. In the case of spinopelvic fixations this principle is difficult to apply, since the opposite side would be the abdominal and sacral area, and therefore we would need an anterior support for it to function. It could be used in sacral fractures with an intact anterior cortex if we osteosynthesise it with a plate.20 The impossibility of applying this principle in the usual spinopelvic fixation makes it necessary to seek alternatives that give more resistance to the assembly, which is why triangular fixation (spinopelvic fixation together with iliosacral fixation) is considered the most stable assembly for this type of fracture.
The success of these biomechanical principles will not only depend on their correct application intraoperatively, because any external circumstance that unduly increases the shear and/or rotational forces can cause the system to fail. Correct follow-up is therefore very important, applying the guidelines for sitting, assisted ambulation, and physiotherapy chronologically and appropriately.
TreatmentThe treatment of choice for complex sacral and SPD fractures is surgery. Conservative orthopaedic treatment is only recommended in 4 circumstances: non-displaced high transverse sacral fractures (<10mm), sacral fractures distal to the sacroiliac joint, patients whose general condition or comorbidities pose a high surgical risk or those who due to their baseline situation or associated injuries are not going to be walking for at least 2–3 months.7,10,16,21,22 According to the AO/OTA classification, type B and C fractures are to be treated surgically, except for B2.1 in young patients in whom surgical and orthopaedic treatment seem to have the same results.23 Attempts to standardise treatment through classifications that decrease indication error are ongoing, which leads us to believe that no system is good enough. This has led to the creation of numerical systems such as, among others, the abovementioned lumbosacral injury classification system (LSICS), in which scores above 4 generally indicate surgical treatment.8,16
Most of these patients are polytraumatised, in whom the presence of severe cranioencephalic trauma or other bone or visceral lesions makes both correct neurological physical examination and early surgical treatment difficult.1,19,22 This means that definitive surgical treatment often has to be delayed until haemodynamic stability is achieved, although it is recommended before 72h have elapsed as this facilitates reduction manoeuvres1; however, some authors set a limit of 14 days after the trauma.24 In cases with neurological symptoms, surgery should be performed as soon as possible, preferably within the first 24h.25
Once the surgical option has been decided, we should study the type of fracture and the osteosynthesis principles to be applied. Triangular osteosynthesis is currently considered the treatment of choice for SPD as it is the most vertically and rotationally stable fixation system, in addition to reducing the sacral kyphosis that is usually observed in the post-operative follow-up.1,7,20–22,25–27 This triangle is usually formed by two systems: a horizontal transverse fixation with iliosacral screws that allow us to apply fundamentally the principle of compression, as well as some neutralisation, and a vertical lumbopelvic fixation that acts according to the principles of support and neutralisation.1,7,20
The horizontal component of the triangle is usually performed with two percutaneous partial-threaded iliosacral screws with washers, although it is currently questioned whether two screws provide more stability than one.1,7,20,22,27,28 Full thread screws are recommended to avoid compression in cases of vertical sacral fractures that cross the conjunction holes and in comminuted fractures4,7,20; however, there are authors who even in these cases recommend compression, since they have not observed clinical neurological involvement after applying it.1 Transiliac-transsacral screws provide greater stability than two iliosacral screws, although they are more technically demanding, especially in cases of sacral dysmorphism, without providing advantages in terms of pain and function one year after the intervention.9,16,20,22 In recent works, based on biomechanical stability fundamentally in osteoporotic bone, the use of 2 transiliac-transsacral screws is recommended as the most stable construct (1 in S1+another in S2 as the best combination); in cases in which they cannot be used, only one can be used, or simple uni- or bilateral iliosacral screws are substituted/added, it is recommended to complete the construct with the vertical component of the triangle (spinopelvic fixation).29 In simple fractures in which the horizontal fracture line is very caudal and the displacement is minimal, essentially Roy Camille I fractures, we can use this horizontal component exclusively without a vertical component and without early loading1,8,9,28; however, the percentage of loosening of the system in these cases is 18% as opposed to the 5% observed when it is associated with vertical iliolumbar fixation.22,30,31 Although this procedure is usually performed with the patient in the supine position, good results have also been described with the patient prone.28,29 Osteosynthesis of the fracture of the anterior zone of the pelvic ring facilitates the reduction and posterior osteosynthesis of the sacral fracture, both are essential when there is a fracture with vertical instability in which, for whatever reason, spinopelvic fixation is not performed28; however, fixation of the fracture of the anterior pelvic ring is not routinely recommended.29
The vertical component of the triangle consists of bilateral vertebral fixation coupled with bilateral iliac screw fixation; it is usually performed using bilateral screws, both transpedicular and iliac. The wider the assembly, the greater the power of neutralisation, which is why authors are increasingly recommending spinopelvic fixation from L4 to the iliac bone, especially when there is a fracture of the transverse process of L5, fracture of the pedicle of L5, poor bone quality, or the impossibility of using iliosacral screws.7,22,31,32 In the latter case, in addition, both vertical fixation rods should be connected by “crosslink” systems to maintain correct neutralisation of rotational and shear forces.1,7,9,20,32,33 The presence of scoliosis does not worsen the functional results.22 There are other assembly systems with promising results in in vitro biomechanical studies that appear to provide clinical advantages for these patients, although more clinical evidence is needed to recommend their routine use.3,20
Iliac fixation of the vertical component is performed with a screw in each iliac bone that can be connected directly to the lumbar system or through an offset that medialises its position and aligns it with the rest of the system.21 The two most common ways of performing this fixation are the S1-iliac screws and the S2-alar-iliac screws (Fig. 6). Biomechanically, both options are similar in traumatic pathology, although the main difference is found in soft tissue involvement, infections, and discomfort due to the implant, with a lower incidence in S2-alar-iliac screws.7,32,34 In vitro biomechanical studies have shown that the use of 2 iliac screws on each side provides greater resistance to torsional forces and eliminates residual sacroiliac movement, which could reduce pain in these patients.27,35 Anatomically, the insertion of the S2-alar-iliac screws does not violate the sacroiliac joint, so that residual pain due to degeneration should be absent; however, up to 3.2% incidence of sacroiliac pain has been described with the use of these implants.32 Cemented screws, even in insufficiency fractures or revision surgeries, and even with promising in vitro results, cannot be recommended at present due to a lack of clinical evidence.25,36
The choice of surgical approach will largely depend on the degree of fracture displacement, considering that slightly displaced fractures with sacral kyphosis <30° are mostly reduced by placing the patient in prone decubitus without additional manoeuvres. Hip extension or Schanz placement on the pedicle of L5 and posterosuperior iliac spine are other minimally invasive manoeuvres that help us achieve adequate reduction.1,25 In all these cases, percutaneous spinopelvic fixation could be recommended, even robot-assisted, which involves less blood loss than the open approach37; however, it is a very demanding technique that has not provided clear advantages to date in terms of complications or intraoperative time10,38; neither are they useful in cases in which there is a neurological deficit.24 In cases in which these manoeuvres result in an insufficient reduction, we should opt for open approaches, and consider the implants of our fixation the best elements to achieve a good reduction, either manually or using distractors, forceps, or laminotomy punches.10,25 The pelvic incidence is the best parameter to assess the adequacy of our reduction.9,16,22,39 The use of preoperative or intraoperative trans-skeletal traction is not systematically recommended because it hinders rotational reduction manoeuvres.7
Approximately 70% of patients with SPD will present neurological symptoms on admission, although it is difficult to quantify them because, in many cases, physical examination is difficult because these are polytraumatised patients.10 Although neurological symptoms will improve in 80% regardless of the treatment performed (orthopaedic or surgical),1,22 better functional results have been described when surgical decompression is performed as soon as possible (<24h)22,39; however, there are authors who obtain favourable results by performing it in the first 72h.9 However, we must consider that a decompression of the sacral neural elements carries a high risk of iatrogenic neurological injury, as well as soft tissue coverage problems that can lead to serious complications, therefore we must consider the type of neurological symptoms that the patient presents, whether continuous or intermittent, triggered by movement, or progressive. In many cases the reduction of the fracture and immobilisation of the bone segment with the usual surgical fixation system is sufficient for these symptoms to disappear.1,39 The presence of bone fragments in the neural canal is not in itself an indication of neural decompression.7,16,24,40 The presence of these fragments at the foraminal level, even in the absence of neurological symptoms, is considered by some authors an indication for decompression, either directly by laminectomy or indirectly by means of a bone fixation system.10,41 The incidence of durotomy due to trauma can reach 80%, and therefore when decompression is performed, it should be considered preoperatively that it is highly likely that a dural repair will be necessary.9
Adding a bone graft to the construct does not seem necessary since the objective of triangular osteosynthesis in this fracture is sacral consolidation, but not posterolateral vertebral arthrodesis.1,7 This consideration is in line with the increasingly frequent recommendation to remove osteosynthesis material 6–9 months after implantation in patients who present pain when the sacral fracture has consolidated, in order to improve their quality of life,22,24,32,42 although there is no real evidence in this aspect regarding mobility or cartilage degeneration there does seem to be evidence of mechanical failure of the rods due to the presence of non-fused sacroiliac joints.7,24
After surgery, care and weightbearing recommendations are similar in all published works. If a triangular spinopelvic fixation is performed, weightbearing using a walking stick is allowed from the day after surgery, whereas if only a horizontal component iliosacral fixation is performed, it is recommended to delay weightbearing for 6–12 weeks.1,7,22,28,29,43
Postoperative follow-up should be performed with simple anteroposterior and lateral X-rays until bone callus is seen, generally recommended at 6 weeks, 3 months, 6 months, and 12 months postoperatively.28 Some authors protocolise a CT scan at 24 weeks to confirm fracture healing.1,10,22
ComplicationsComplications occur in about 30% of spinopelvic fixations, the most frequent being discomfort due to the osteosynthesis material (up to 95%) and infections (36%–50%, being higher in non-percutaneous approaches), followed by implant failure (11%–17%) and pseudoarthrosis (9.3%). Other less frequent complications are Morel-Lavallée lesion (7.9%), superior gluteal artery injuries (1.2%), sacral nerve root injuries (2%–15%, although this can increase to 40% when neural decompression is performed), screw malposition (2%–15%), deep vein thrombosis, progression of sacral kyphosis (not dependent on anterior ring fixation), cerebrospinal fluid leakage, or ureteral and bladder injury, the last being unlikely.8–10,22,24,28,44
Different strategies have been proposed to reduce these complications. As mentioned, the use of percutaneous surgical approaches decreases blood loss and seems to reduce the risk of infection.10,38,45,46 This risk also decreases with the use of iliac alar S2 screws versus iliac S1 screws,32,34,47 and with 3D planning and the use of intraoperative CT with navigation system, based fundamentally on the decreased surgical time, ample tissue destruction in the approach, and accurate positioning of implants.28,47–49
DiscussionThe wide heterogeneity of the classifications used for spinopelvic dissociation makes it difficult to establish any one as a guide to decide surgical or conservative treatment, beyond the logical general considerations that make orthopaedic treatment the preferred option.7,8,10,16,21,22 However, increasingly more studies analyse these indications according to a reproducible classification, this being one of the basic pillars to be investigated in future studies.8,16,23
Triangular osteosynthesis is now considered the surgical treatment of choice,1,7,20–22,25–27 although this fixation must be understood from its biomechanical bases for it to be used correctly.7 Applying basic concepts means we can understand when to make a horizontal construct only, when to add a vertical component, when to use longer fixations, unilateral, with double horizontal screws, or at various levels in the sacrum. In this regard, the field of research is very broad and little explored to date, and is of special interest in clinical practice because, together with the reproducibility of previous classifications, these concepts help to standardise treatment with a decrease in potential complications, and also avoid the use of very aggressive or insufficiently resistant techniques for each case. Currently, the results of finite element studies seem promising for application in humans, since they change concepts that previously seemed to be well established and involve less surgical aggression, such as unilateral fixation.20 However, all of them must be applied clinically to establish a change of recommendation and this has not happened as yet.
The interest in delivering increasingly more precise treatments with less margin for error and that are less aggressive has also led to the introduction of different techniques used in spinopelvic dissociation such as percutaneous approaches, navigation, or the use of intraoperative CT.28,47–49 However, the anatomical difficulty, the presence of frequent synchronous injuries, or the long learning curve mean that these are still considered innovative techniques even with good results, and therefore constitute another field for future research.
The limitations of this work the low incidence of this pathology and therefore of publications on it, together with their heterogeneity in terms of baseline characteristics, which makes them difficult to compare. The inclusion of elderly patients as well as adolescents studied in the same work means that the conclusions of the investigations do not have a strong recommendation, since they eliminate the basal chronological biological factor. In addition, biomechanical work on finite elements has been included without clinical studies in humans, thus opening new avenues of study although the current clinical evidence still should not be considered high.
ConclusionsSPD is a serious injury, although rare, and therefore, acquiring sufficient experience for it not to be challenging is generally complicated. It appears in the context of fractures through the sacrum that combine longitudinal and transverse fracture lines leading to a lack of continuity between the spine and the pelvis; in addition, they entail numerous associated neurological, vascular, and visceral injuries. They have a bimodal presentation, as they usually occur in young people, due to high-energy trauma, or in older people after mild trauma, forming part of the fragility fractures of the pelvis. For diagnosis, the most indicated imaging test is multislice CT of less than 5mm, due to the multiplanar nature of these fractures. MRI is relegated in these cases to the diagnosis of stress or insufficiency fractures. Many classifications have been described over the last decades, the most current are based on the biomechanical behaviour of these fractures, although more studies are needed to achieve a better diagnostic-therapeutic correlation based on these classifications.
The treatment of choice is surgical, reserving the conservative orthopaedic option for patients with low functional demand, non-displaced fractures, or very distal fracture lines in the sacrum. Surgery should be performed as soon as possible to facilitate reduction manoeuvres, triangular fixation being the most stable system using transiliac-transsacral screws, bilateral proximal transpedicular screws, and bilateral S2-alar-iliac screws. Neural decompression should be performed in cases presenting continuous neurological symptoms; the presence of bone fragments in the neural canal is not in itself an indication for direct decompression. The use of bone grafting is not recommended systematically, because it is also suggested that bone fixation material be removed as soon as the sacral fracture is consolidated. The most frequent complications are discomfort due to the osteosynthesis material and infection of the surgical site, although there are strategies that help minimise these, such as the use of percutaneous approaches, preoperative planning with 3D systems, intraoperative navigation, or the use of S2-alar-iliac screws.
Level of evidenceLevel of evidence I.
Conflict of interestsThe authors have no conflict of interests to declare.