Radiology is now an essential part of Clinical Medicine, but undergraduate training does not reflect its importance in medical practice. In the current course, there are 46 medical schools in our country. According to the information published on the institutional websites, the study plans are very different in terms of the presence of Diagnostic Radiology and the organization of teaching. The estimated number of teaching hours in diagnostic radiology (mean ± standard deviation) is 61.3 ± 22.2 h (range from 26 h to 137 h). There is a great shortage of clinical university professors, and a generational change is essential. The current situation poses various challenges, including adapting to new teaching methods and technologies and promoting the presence of radiology in medical study plans, paying special attention to hospital practices, the Final Degree Project (FDP) and the Objective Structured Clinical Examination (OSCE).
La radiología es actualmente una parte esencial de la medicina clínica, pero la formación en pregrado no refleja su importancia en la práctica médica. En el curso actual, hay 46 facultades de medicina en nuestro país. Según la información publicada en las web institucionales, los planes de estudio son muy diferentes en cuanto a la presencia del Radiodiagnóstico y organización de la docencia. El número de horas docentes de radiodiagnóstico estimadas (media ± desviación estándar) es de 67,0 ± 21,9 h (rango de 26 h a 137 h). Hay gran escasez de profesores universitarios clínicos y es imprescindible un recambio generacional. La situación actual plantea diversos retos, entre ellos adaptarnos a los nuevos métodos y tecnologías docentes y fomentar la presencia de radiología en los planes de estudio de medicina, prestando especial atención a las prácticas hospitalarias, el Trabajo Fin de Grado (TFG) y la Evaluación Clínica Objetiva Estructurada (ECOE).
Radiology is now an essential part of clinical medicine.1–3 Medical imaging is at the heart of clinical decision making, providing important morphological and functional information that is used in diagnosis, treatment monitoring and prognostic assessments for many diseases. In addition, image-guided interventions can treat pathologies, thus reducing morbidity and healthcare costs. For all these reasons, it is essential to train future doctors properly in radiology. However, radiology teaching in undergraduate courses does not reflect its importance in clinical practice. Not enough time is allocated in medical curricula,4 and both students and graduates call for more radiology training in their courses.5,6
There are various issues to consider when examining the current situation of undergraduate radiology training in Spain. Firstly, there is a huge diversity of medical curricula, with widely varying teaching hours, organisation and teaching methodologies, as is the case in other countries.4,7,8 In Spain, the situation is complicated by a severe shortage of university lecturers in clinical areas, such as in diagnostic radiology. Looking ahead, training in radiology should embrace new medical education teaching methods and technologies that increase motivation and reinforce self-directed student learning.
As radiologists, our challenge is to increase theoretical and practical radiology training during medical studies and promote our specialty among future doctors. To reiterate, our objective of incorporating strategies to boost radiological training is to inspire future medics to pursue this vocation.1,9 However, there are other more important objectives to be considered, such as the standardisation of physicians' knowledge and view of the diagnostic radiology specialty and improving diagnostic test ordering to ensure that it is appropriate at all times. This will result in a better use of the resources offered by our specialty.
Undergraduate content and instructorsThere are two key questions: how can radiology contribute to the training of future doctors; and what resources are needed to do so adequately?9 Radiological images help students learn about the anatomy and physiology of living human beings, with perfused and hydrated tissues and organs. Additionally, students learn about the variability that exists among patients and how anatomical structures correlate with the occurrence of pathology. Thus, for example, lung fissures, which are normally almost invisible, show up as a clear border in lobar or segmental alveolar infiltrates, while the presence of ascites clearly reveals peritoneal spaces on CT. Students can correlate the anatomy with the projected images provided by radiographs, in addition to CT or MRI images, providing an excellent opportunity to study three-dimensional anatomy in detail. Studying physiology can be complemented with the clinical applicability of contrast-enhanced studies, combinations with isotopic techniques (PET-CT and SPECT-CT), or techniques such as functional MRI. Ultrasound is increasingly used as a tool to study ‘living anatomy’, supporting students' anatomical knowledge and adding clinical contextualisation.10 Medical students must become skilled in interpreting chest and musculoskeletal radiographs to be able to interpret basic abnormalities and to distinguish normal from abnormal cases. In addition, a critical aspect of training in radiograph interpretation involves the ability to distinguish between those cases that can be managed by doctors who are not radiologists and those that should be referred for radiological consultation.11 Finally, students should be trained to request medical imaging appropriately, with an awareness of the indications, limitations and associated risks of each imaging modality.
An analysis of these needs and the heterogeneity detected a decade ago in radiology training in different countries8 led to a proposed European undergraduate curriculum, last revised in 2021.12 It consists of 14 modules of learning objectives concerning knowledge, skills, competences and attitudes, as a basis for curricular planning, which each medical school can adapt to its particular situation. Some countries, such as Germany13 and the United Kingdom14 have developed their own undergraduate radiology curricula.
Traditionally, it was not uncommon for non-radiologists to teach radiology at undergraduate level. In recent years this has become increasingly uncommon given the complexity of the different imaging modalities and the undeniable in-depth training of radiologists in their knowledge and clinical management.4 A recent survey by the European Society of Radiology on undergraduate training15 reports an improvement over the last decade in the participation of radiologists in undergraduate training in affiliated countries. The current trend is for radiology to be taught by radiologists, as they have a unique position as instructors within the health care system given that radiological images converge with almost all medical disciplines.16 This is important for students to acquire a deeper knowledge of radiology, and a more realistic view of the clinical specialty of diagnostic radiology. There must be no backtracking on this, and medical school deans must identify radiologists as the faculty members to be approached for medical imaging education.2
The situation in SpainSince 1983, with the publication of the University Reform Law, university education in Spain has been organised into areas of knowledge,17 defined in the Organic Law on Universities of 200118 as ‘fields of knowledge characterised by the homogeneity of their object of knowledge, a common historical tradition and the existence of national or international communities of teachers and researchers’. While an update is soon expected to the University System Law,19 each subject in a university curriculum is currently assigned to one of the 190 knowledge areas that exist,20 23 of which feature in medical graduate studies. Diagnostic radiology is integrated into knowledge area 770: ‘Radiology and Physical Medicine’, together with other medical specialties, nuclear medicine, radiation oncology, and physical medicine and rehabilitation. University professors must be assigned to a specific area of knowledge. University departments, for their part, constitute the smallest administrative and economic unit of the institution18 and each university organises its departments, often grouping together several areas of knowledge.
Radiology in national curriculaThe current Spanish medical curriculum is the result of a university curricular reform based on the European Higher Education Area. This reform introduced a system of equivalent credits throughout Europe (European Credit Transfer System [ECTS]), focusing on student work rather than on class attendance, prioritising learning over teaching. One ECTS credit is equivalent to approximately 25–30 h, which includes the estimated time for homework, as well as the time spent on assessment. The equivalent in face-to-face teaching hours of an ECTS credit may vary from one university to another, but is usually estimated at around 10 h per ECTS credit.
The undergraduate degree in Medicine takes 6 years (360 ECTS credits) to complete. The requirements for the verification of official undergraduate degrees in medicine, published in the Order ECI/332/2008,21 determine that the curriculum should include as a minimum the following modules:
- I.
Morphology, structure and function of the human body (64 ECTS credits).
- II.
Social medicine, communication skills and introduction to research (30 ECTS credits).
- III.
Human clinical training (100 ECTS credits).
- IV.
Diagnostic and therapeutic procedures (40 ECTS credits).
- V.
Supervised placements and final year projects (60 ECTS credits).
This Order also sets out the competences that students must acquire. Thus, module I includes the competence ‘can recognise the morphology and structure of tissue, organs and systems using imaging techniques’, and module III repeats ‘can recognise, diagnose and guide the management of leading pathologies, different devices, systems and clinical situations’. Moreover, module IV of Diagnostic and Therapeutic Procedures clearly states that diagnostic radiology should be included in all curricula.22
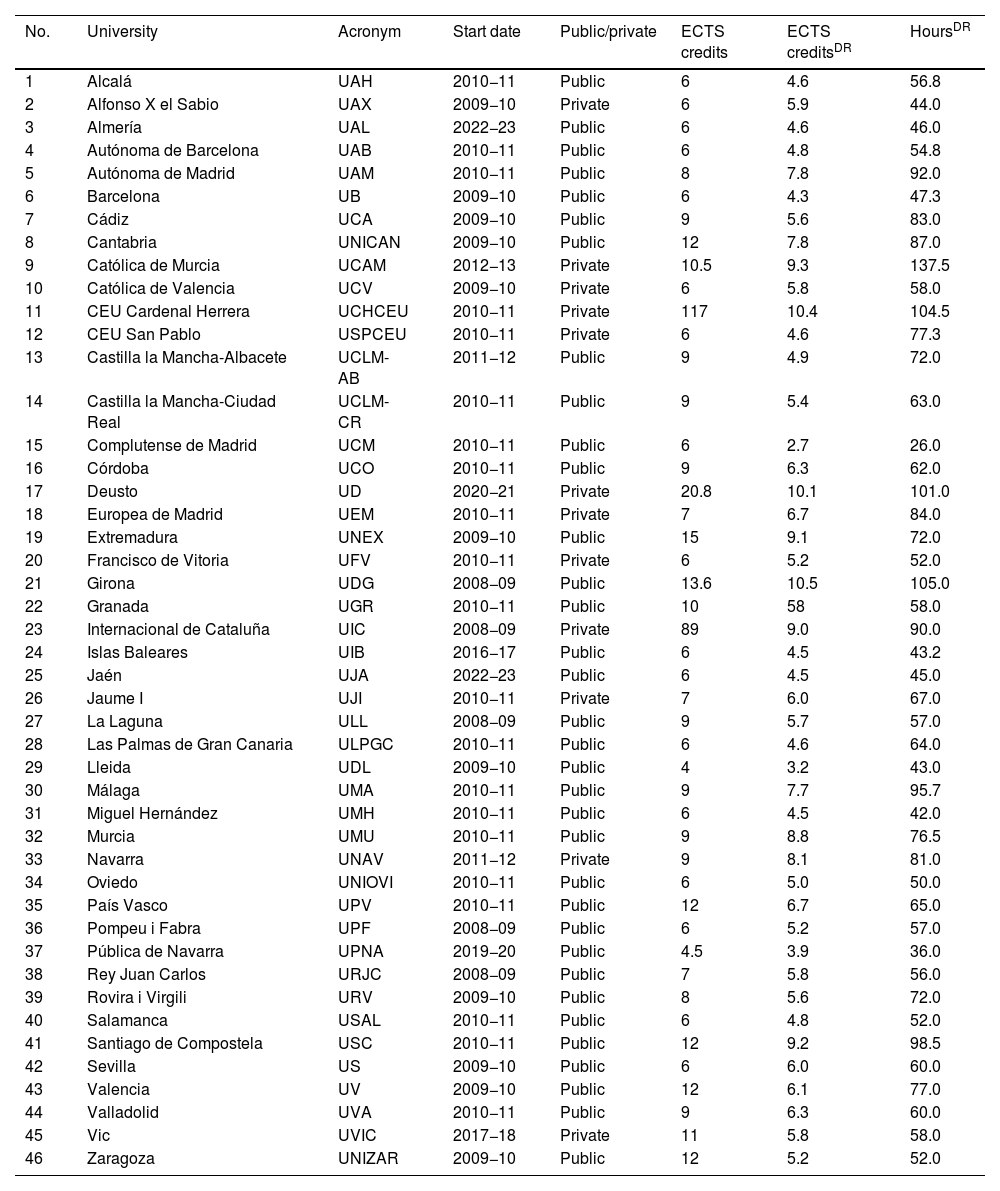
It is difficult to determine the exact status of radiology training in the different national curricula. In 2008, SERAM's training committee produced a report prior to the implementation of the current undergraduate studies model7 which concluded that radiology teaching was heterogeneous in its programmes and organisation in the 28 universities that existed at the time. In the current academic year 2022/2023, there are 46 medical schools in our country: 34 public and 12 private (Table 1). The new curriculum started being taught between 2008/2009 and 2010/2011 in 37 of them, and some have already embarked on reforming their curricula. Five medical schools have only recently been established and their first intake are yet to graduate. The two most recent, Jaén and Almería, only began offering medical studies this academic year.
Undergraduate medicine studies in Spain together with the ECTS credits and teaching hours for diagnostic radiology (DR).
| No. | University | Acronym | Start date | Public/private | ECTS credits | ECTS creditsDR | HoursDR |
|---|---|---|---|---|---|---|---|
| 1 | Alcalá | UAH | 2010−11 | Public | 6 | 4.6 | 56.8 |
| 2 | Alfonso X el Sabio | UAX | 2009−10 | Private | 6 | 5.9 | 44.0 |
| 3 | Almería | UAL | 2022−23 | Public | 6 | 4.6 | 46.0 |
| 4 | Autónoma de Barcelona | UAB | 2010−11 | Public | 6 | 4.8 | 54.8 |
| 5 | Autónoma de Madrid | UAM | 2010−11 | Public | 8 | 7.8 | 92.0 |
| 6 | Barcelona | UB | 2009−10 | Public | 6 | 4.3 | 47.3 |
| 7 | Cádiz | UCA | 2009−10 | Public | 9 | 5.6 | 83.0 |
| 8 | Cantabria | UNICAN | 2009−10 | Public | 12 | 7.8 | 87.0 |
| 9 | Católica de Murcia | UCAM | 2012−13 | Private | 10.5 | 9.3 | 137.5 |
| 10 | Católica de Valencia | UCV | 2009−10 | Private | 6 | 5.8 | 58.0 |
| 11 | CEU Cardenal Herrera | UCHCEU | 2010−11 | Private | 117 | 10.4 | 104.5 |
| 12 | CEU San Pablo | USPCEU | 2010−11 | Private | 6 | 4.6 | 77.3 |
| 13 | Castilla la Mancha-Albacete | UCLM-AB | 2011−12 | Public | 9 | 4.9 | 72.0 |
| 14 | Castilla la Mancha-Ciudad Real | UCLM-CR | 2010−11 | Public | 9 | 5.4 | 63.0 |
| 15 | Complutense de Madrid | UCM | 2010−11 | Public | 6 | 2.7 | 26.0 |
| 16 | Córdoba | UCO | 2010−11 | Public | 9 | 6.3 | 62.0 |
| 17 | Deusto | UD | 2020−21 | Private | 20.8 | 10.1 | 101.0 |
| 18 | Europea de Madrid | UEM | 2010−11 | Private | 7 | 6.7 | 84.0 |
| 19 | Extremadura | UNEX | 2009−10 | Public | 15 | 9.1 | 72.0 |
| 20 | Francisco de Vitoria | UFV | 2010−11 | Private | 6 | 5.2 | 52.0 |
| 21 | Girona | UDG | 2008−09 | Public | 13.6 | 10.5 | 105.0 |
| 22 | Granada | UGR | 2010−11 | Public | 10 | 58 | 58.0 |
| 23 | Internacional de Cataluña | UIC | 2008−09 | Private | 89 | 9.0 | 90.0 |
| 24 | Islas Baleares | UIB | 2016−17 | Public | 6 | 4.5 | 43.2 |
| 25 | Jaén | UJA | 2022−23 | Public | 6 | 4.5 | 45.0 |
| 26 | Jaume I | UJI | 2010−11 | Private | 7 | 6.0 | 67.0 |
| 27 | La Laguna | ULL | 2008−09 | Public | 9 | 5.7 | 57.0 |
| 28 | Las Palmas de Gran Canaria | ULPGC | 2010−11 | Public | 6 | 4.6 | 64.0 |
| 29 | Lleida | UDL | 2009−10 | Public | 4 | 3.2 | 43.0 |
| 30 | Málaga | UMA | 2010−11 | Public | 9 | 7.7 | 95.7 |
| 31 | Miguel Hernández | UMH | 2010−11 | Public | 6 | 4.5 | 42.0 |
| 32 | Murcia | UMU | 2010−11 | Public | 9 | 8.8 | 76.5 |
| 33 | Navarra | UNAV | 2011−12 | Private | 9 | 8.1 | 81.0 |
| 34 | Oviedo | UNIOVI | 2010−11 | Public | 6 | 5.0 | 50.0 |
| 35 | País Vasco | UPV | 2010−11 | Public | 12 | 6.7 | 65.0 |
| 36 | Pompeu i Fabra | UPF | 2008−09 | Public | 6 | 5.2 | 57.0 |
| 37 | Pública de Navarra | UPNA | 2019−20 | Public | 4.5 | 3.9 | 36.0 |
| 38 | Rey Juan Carlos | URJC | 2008−09 | Public | 7 | 5.8 | 56.0 |
| 39 | Rovira i Virgili | URV | 2009−10 | Public | 8 | 5.6 | 72.0 |
| 40 | Salamanca | USAL | 2010−11 | Public | 6 | 4.8 | 52.0 |
| 41 | Santiago de Compostela | USC | 2010−11 | Public | 12 | 9.2 | 98.5 |
| 42 | Sevilla | US | 2009−10 | Public | 6 | 6.0 | 60.0 |
| 43 | Valencia | UV | 2009−10 | Public | 12 | 6.1 | 77.0 |
| 44 | Valladolid | UVA | 2010−11 | Public | 9 | 6.3 | 60.0 |
| 45 | Vic | UVIC | 2017−18 | Private | 11 | 5.8 | 58.0 |
| 46 | Zaragoza | UNIZAR | 2009−10 | Public | 12 | 5.2 | 52.0 |
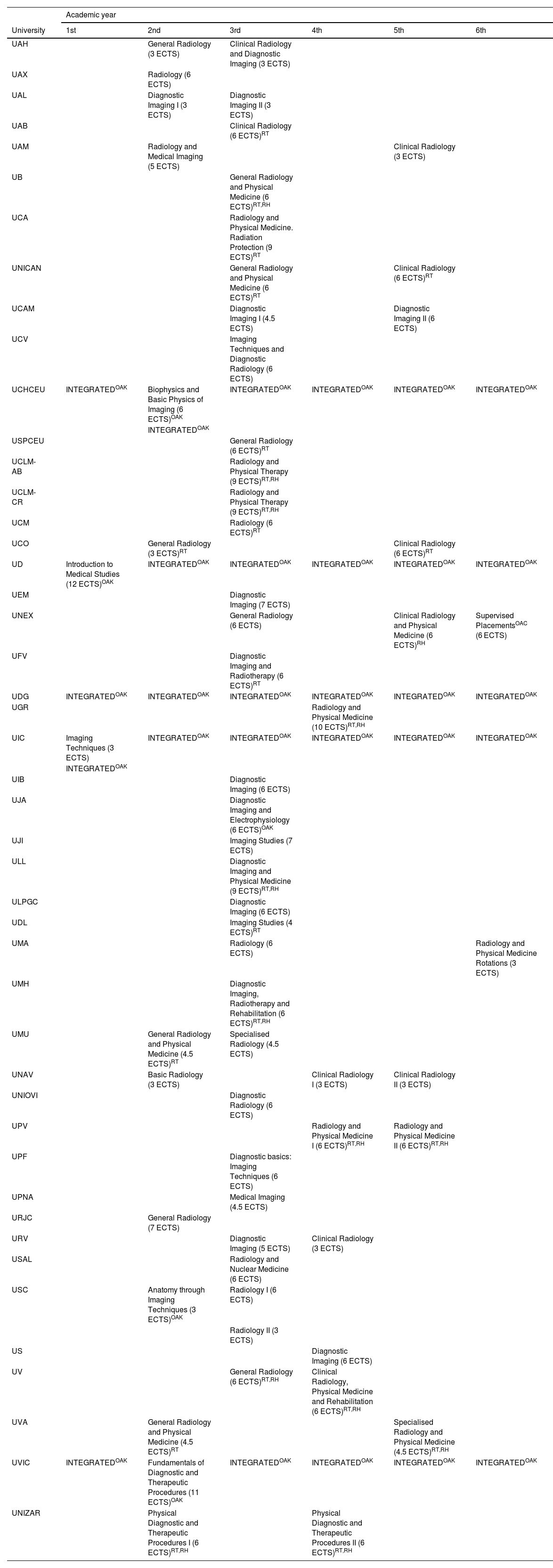
In March and April 2023, we reviewed the curricula published on the websites of 46 medical schools, identifying the compulsory subjects in which diagnostic radiology is taught and the corresponding year it is taught in (Table 2). We also examined the teaching manuals of the subjects in order to calculate how many ECTS credits it accounted for and how many classroom hours are dedicated to diagnostic radiology, taking into account the hours dedicated to theory, seminars and hospital placements as described in the teaching manuals, excluding hours spent on rehabilitation, radiotherapy or nuclear medicine. On this basis, we have calculated the proportion of ECTS credits that correspond to diagnostic radiology. In the medical schools where it was detected that diagnostic radiology is integrated into the teaching of other subjects in the degree course, the coordinators were contacted to request an estimate of the teaching hours.
Compulsory subjects which include diagnostic radiology content in each university, by academic year.
| Academic year | ||||||
|---|---|---|---|---|---|---|
| University | 1st | 2nd | 3rd | 4th | 5th | 6th |
| UAH | General Radiology (3 ECTS) | Clinical Radiology and Diagnostic Imaging (3 ECTS) | ||||
| UAX | Radiology (6 ECTS) | |||||
| UAL | Diagnostic Imaging I (3 ECTS) | Diagnostic Imaging II (3 ECTS) | ||||
| UAB | Clinical Radiology (6 ECTS)RT | |||||
| UAM | Radiology and Medical Imaging (5 ECTS) | Clinical Radiology (3 ECTS) | ||||
| UB | General Radiology and Physical Medicine (6 ECTS)RT,RH | |||||
| UCA | Radiology and Physical Medicine. Radiation Protection (9 ECTS)RT | |||||
| UNICAN | General Radiology and Physical Medicine (6 ECTS)RT | Clinical Radiology (6 ECTS)RT | ||||
| UCAM | Diagnostic Imaging I (4.5 ECTS) | Diagnostic Imaging II (6 ECTS) | ||||
| UCV | Imaging Techniques and Diagnostic Radiology (6 ECTS) | |||||
| UCHCEU | INTEGRATEDOAK | Biophysics and Basic Physics of Imaging (6 ECTS)OAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK |
| INTEGRATEDOAK | ||||||
| USPCEU | General Radiology (6 ECTS)RT | |||||
| UCLM-AB | Radiology and Physical Therapy (9 ECTS)RT,RH | |||||
| UCLM-CR | Radiology and Physical Therapy (9 ECTS)RT,RH | |||||
| UCM | Radiology (6 ECTS)RT | |||||
| UCO | General Radiology (3 ECTS)RT | Clinical Radiology (6 ECTS)RT | ||||
| UD | Introduction to Medical Studies (12 ECTS)OAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK |
| UEM | Diagnostic Imaging (7 ECTS) | |||||
| UNEX | General Radiology (6 ECTS) | Clinical Radiology and Physical Medicine (6 ECTS)RH | Supervised PlacementsOAC (6 ECTS) | |||
| UFV | Diagnostic Imaging and Radiotherapy (6 ECTS)RT | |||||
| UDG | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK |
| UGR | Radiology and Physical Medicine (10 ECTS)RT,RH | |||||
| UIC | Imaging Techniques (3 ECTS) | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK |
| INTEGRATEDOAK | ||||||
| UIB | Diagnostic Imaging (6 ECTS) | |||||
| UJA | Diagnostic Imaging and Electrophysiology (6 ECTS)OAK | |||||
| UJI | Imaging Studies (7 ECTS) | |||||
| ULL | Diagnostic Imaging and Physical Medicine (9 ECTS)RT,RH | |||||
| ULPGC | Diagnostic Imaging (6 ECTS) | |||||
| UDL | Imaging Studies (4 ECTS)RT | |||||
| UMA | Radiology (6 ECTS) | Radiology and Physical Medicine Rotations (3 ECTS) | ||||
| UMH | Diagnostic Imaging, Radiotherapy and Rehabilitation (6 ECTS)RT,RH | |||||
| UMU | General Radiology and Physical Medicine (4.5 ECTS)RT | Specialised Radiology (4.5 ECTS) | ||||
| UNAV | Basic Radiology (3 ECTS) | Clinical Radiology I (3 ECTS) | Clinical Radiology II (3 ECTS) | |||
| UNIOVI | Diagnostic Radiology (6 ECTS) | |||||
| UPV | Radiology and Physical Medicine I (6 ECTS)RT,RH | Radiology and Physical Medicine II (6 ECTS)RT,RH | ||||
| UPF | Diagnostic basics: Imaging Techniques (6 ECTS) | |||||
| UPNA | Medical Imaging (4.5 ECTS) | |||||
| URJC | General Radiology (7 ECTS) | |||||
| URV | Diagnostic Imaging (5 ECTS) | Clinical Radiology (3 ECTS) | ||||
| USAL | Radiology and Nuclear Medicine (6 ECTS) | |||||
| USC | Anatomy through Imaging Techniques (3 ECTS)OAK | Radiology I (6 ECTS) | ||||
| Radiology II (3 ECTS) | ||||||
| US | Diagnostic Imaging (6 ECTS) | |||||
| UV | General Radiology (6 ECTS)RT,RH | Clinical Radiology, Physical Medicine and Rehabilitation (6 ECTS)RT,RH | ||||
| UVA | General Radiology and Physical Medicine (4.5 ECTS)RT | Specialised Radiology and Physical Medicine (4.5 ECTS)RT,RH | ||||
| UVIC | INTEGRATEDOAK | Fundamentals of Diagnostic and Therapeutic Procedures (11 ECTS)OAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK | INTEGRATEDOAK |
| UNIZAR | Physical Diagnostic and Therapeutic Procedures I (6 ECTS)RT,RH | Physical Diagnostic and Therapeutic Procedures II (6 ECTS)RT,RH | ||||
INTEGRATED. Indicates those medical schools where diagnostic radiology is integrated into other medical disciplines.
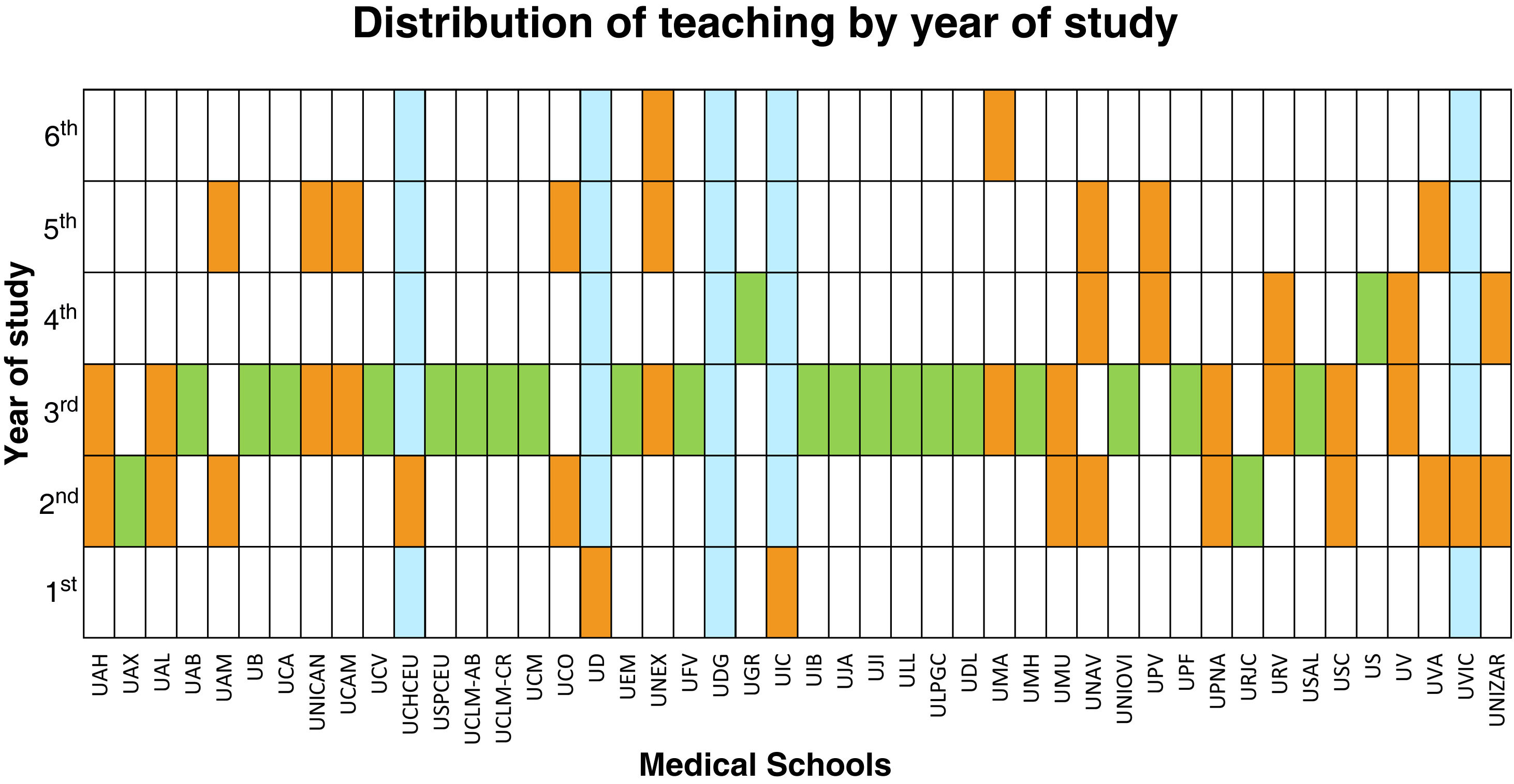
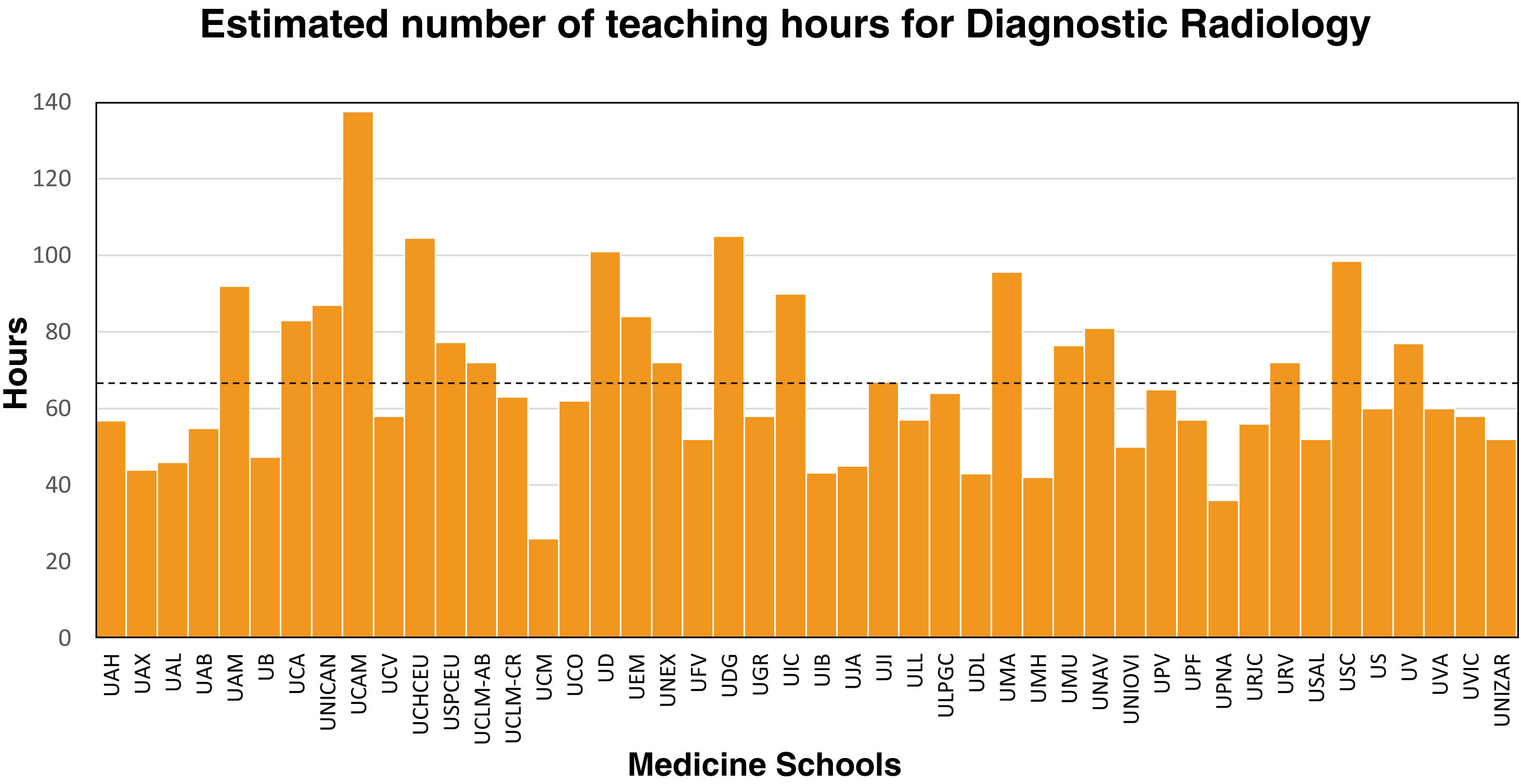
It can be seen that diagnostic radiology training starts at different points of the degree depending on the university (Table 2, Fig. 1). Only two schools offer radiology subjects in the first year (UIC and UD); the majority start teaching radiology in the second year (14 schools) or third year (26 schools), and in three schools it starts in the fourth year (UGR, UPV and US). In 24 medical schools there is only one subject where diagnostic radiology is taught, and in 16 there is one general core subject and one specialty or clinical subject. There are five faculties in which radiology teaching is integrated with other disciplines throughout the degree course (UCHCEU, UD, UDG, UIC, UVIC), most of them introduce the subject with a specific course in the first years of the degree, and then integrate it into other subjects in the following years. The estimated number of diagnostic radiology teaching hours (Table 1, Fig. 2) has a mean ± standard deviation of 67.0 ± 21.9 h, with a range of 26 h to 137 h. The number of ECTS credits for diagnostic radiology calculated for specific compulsory subjects is 5.8 ± 1.6, corresponding to an average mean percentage of 75.9% of the ECTS credits of these subjects (range from 43.3% to 100%).
Diagram showing how teaching is distributed among the academic years in the 46 medical schools, according to the data obtained in our study. Green indicates that radiology is taught in a single course in only one year of the degree. Orange indicates that radiology teaching features in more than one year. Blue indicates that radiology teaching is integrated with other areas of knowledge. At UCHCEU and UIC, in addition to the specific subject in the second and first year, respectively, radiology teaching is also integrated into other subjects in these same years.
Thus, the curricula vary considerably in terms of the presence of diagnostic radiology and the way in which teaching is organised. We face the challenge of promoting the presence of radiology in medical curricula: 1) integrated with other subjects; 2) in compulsory subjects; 3) in optional subjects; 4) in hospital placements; 5) in the final year project (TFG, to use the Spanish acronym), and 6) in the Objective Structured Clinical Examination (OSCE).
When radiology teaching is integrated with other clinical specialties, there are advantages and disadvantages that warrant an in-depth analysis beyond the scope of this article. Teaching radiology in an integrated curriculum provides students with a better appreciation of the role of radiology in relation to other specialties23 and allows for a more effective, patient-centred clinical approach to radiological imaging.24 But, in our opinion, this may lead to a situation in which the radiology content is considered secondary, or is taught by non-radiologists, with a consequent decline in the quality of teaching. We recommend a separate assessment for radiology or that it comprises a proportionate share of the assessment, otherwise the students' learning objectives will be dominated by the other subjects they know they will be assessed on.25 The number of diagnostic radiology teaching hours in four of the five universities with integrated teaching is above average (Fig. 2). In any case, having a longitudinal approach to the role of radiology in medical practice is much more beneficial if the fundamentals and basics of the different radiological modalities are introduced beforehand in a specific subject.
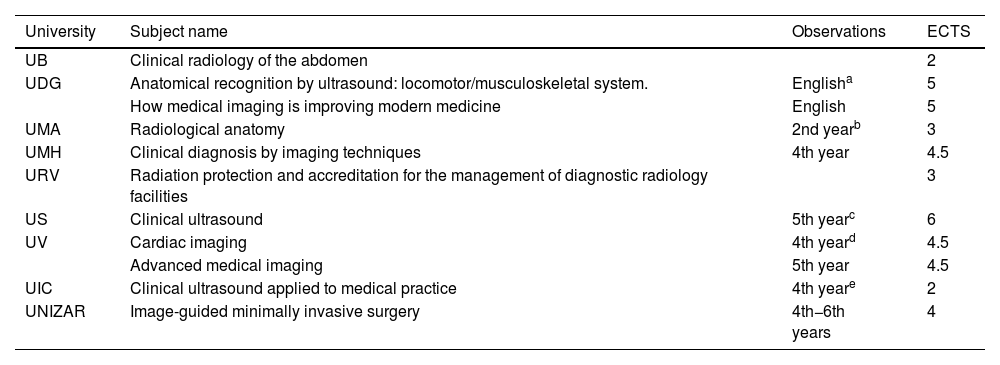
Increasing radiology training in compulsory subjects is important, but changing them in the curriculum is a time-consuming procedure. The inclusion of radiology as one of the optional subject choices is a more flexible approach, and can be a good way of increasing the presence of radiology in the curriculum, deepening knowledge on technological and clinical advances, or reinforcing basic aspects of radiology. Currently, nine medical schools include 11 radiology as an optional subject in their curricula (Table 3).
Optional diagnostic radiology subjects.
| University | Subject name | Observations | ECTS |
|---|---|---|---|
| UB | Clinical radiology of the abdomen | 2 | |
| UDG | Anatomical recognition by ultrasound: locomotor/musculoskeletal system. | Englisha | 5 |
| How medical imaging is improving modern medicine | English | 5 | |
| UMA | Radiological anatomy | 2nd yearb | 3 |
| UMH | Clinical diagnosis by imaging techniques | 4th year | 4.5 |
| URV | Radiation protection and accreditation for the management of diagnostic radiology facilities | 3 | |
| US | Clinical ultrasound | 5th yearc | 6 |
| UV | Cardiac imaging | 4th yeard | 4.5 |
| Advanced medical imaging | 5th year | 4.5 | |
| UIC | Clinical ultrasound applied to medical practice | 4th yeare | 2 |
| UNIZAR | Image-guided minimally invasive surgery | 4th−6th years | 4 |
Clinical placements in radiology services help students better understand how patient studies are performed and provide them with an excellent opportunity to access radiology-specific software systems.26 It also gives them an insight into the work of a radiologist, the thought processes behind diagnoses and the value of communication with other specialists. Although training in the first years, known as pre-clinical training, usually includes anatomy and basic radiological semiology, it is important to encourage placements in radiology departments as early as possible. In general, students perceive early clinical exposure as an important motivator for their studies, enabling links to be made between basic concepts and real patient cases. Similarly, teachers perceive a more integrated approach to teaching basic sciences and clinical medicine, and an increase in students' enthusiasm during their learning.27 As well as motivating the students, this first contact as observers helps them to make better use of their placements in following years.
Medical students should be a regular part of the hospital and care setting, and this is also true for diagnostic radiology services. Our challenge is to increase medical students’ contact with radiology services. Providing high-quality clinical placements requires organisational effort, as well as personal involvement on the part of the radiologist. Attending to a student alongside a busy caseload can indeed require extra effort. Yet, if we want doctors to understand and respect our specialty, we must begin by passing this knowledge and respect on to the students. The first step can perhaps be summed up as caring for students as we would have liked to have been cared for during our studies.
The sixth year of rotations is an entire year devoted to clinical practice. This addition is a vast improvement compared to previous models of medical training. Only two faculties have a specific radiology rotation (UEX and UMA). There may be elective radiology placements in the remaining universities that are not detailed in their curricula. This information is important to know and it is important to increase these elective placements. Some universities include integrated workshops in the final years (UPF), while others include a clinical rotation of 51−54 ECTS credits in the sixth year of their curriculum without specifying the medical specialities involved (UNIOVI, ULPGC, UCA and UAM). This system makes it easy to negotiate the inclusion of specific diagnostic radiology clinical placements in the final year.
The TFG is a compulsory subject worth 6 ECTS credits in which students are trained in research skills. At present, it is estimated that more than 7000 medical students graduate in Spain every year.28 It is important to know how many TFGs are carried out in radiology each year and to encourage students to carry out their TFGs in radiology. An introduction to clinical research and collaboration in the diagnostic radiology services' projects is highly motivating and, furthermore, it increases the students' appreciation of the medical specialty.
The OSCE format facilitates the evaluation of students' clinical skills in a reliable, objective, uniform and standardised manner. It consists of different clinical stations that simulate real clinical scenarios and situations. Since the academic year of 2015/2016, as agreed by the Conference of Deans of Spanish Faculties of Medicine, a multidisciplinary OSCE has been held at the end of the degree course in all Spanish medical schools. Radiology should be present in the medical schools' multidisciplinary OSCEs to reflect its importance in clinical practice.25,29 At least one radiology station should be included in each medical school. Furthermore, these assessment formats allow for the training of students in practical skills specific to diagnostic radiology, so it is appropriate to incorporate their use in undergraduate radiology courses.29
Teaching staffIt is difficult to calculate the number of lecturers specialising in diagnostic radiology at Spanish universities as the information is organised in different ways at different universities and, even if we know how many lecturers there are in the area of knowledge, it is difficult to know which specialty each of them covers. In the 2008 SERAM training commission report7 it was estimated that 28 medical schools were staffed by 199 radiology instructors, an average of 7.1 radiology instructors per school. Ten years later, at the 34th SERAM congress30 a new study estimated that there were 243 radiology instructors at 42 medical schools. The average had fallen to 5.8 instructors per faculty. Moreover, only 16% were permanent lecturers (4 professors, 19 senior lecturers, 16 temporary lecturers and no assistant lecturers), and the vast majority did not work exclusively in teaching. This is compounded by the fact that there is currently a severe shortage of lecturers in all clinical areas. It is estimated that in Spain there is a deficit of 3817 lecturers in medical schools — 2654 permanent and 1163 non-tenured.31 In addition, the current requirements have made it difficult for candidates to access permanent lecturer positions, resulting in an average accreditation age of 56 years for tenured lecturer positions.32 There is an urgent need to recruit more young lecturers, so the challenge is to encourage teaching vocations among students as a way of ensuring there is an adequate number of specialist diagnostic radiology lecturers in medical schools.
New teaching methods and technologiesToday's medical students are digital natives, with an innate aptitude for technology, and they have moved away from taking notes on paper. They have a lot of information at their disposal and need guidance on which study sources are reliable. They do not want lecturers who are ‘PowerPoint readers’, but rather teachers who interact with them, explaining essential aspects of the subject they are studying. They want clinical training, even in the first years, so as not to feel disconnected from medicine. Medical education has evolved, incorporating new teaching formats, such as the flipped classroom, problem-based learning (PBL) or gamification, and e-learning strategies are an essential asset in radiology training.33 Learning formats that include these new combined pedagogical concepts and modern technologies contribute to improved academic performance and increased satisfaction and engagement of medical students.34 Our challenge as radiologists is to learn about these changes and incorporate them into undergraduate radiology teaching.
In the flipped classroom, the focus shifts to the students who are provided with the teaching content in advance, and the classroom time is used to encourage discussion and clarify doubts. The flipped classroom encourages students to work independently and maximises the application of the content learned in highly interactive sessions.33 In PBL, problems are posed to develop problem-solving skills in clinical situations while teachers act as facilitators or guides as students acquire information through self-directed learning.35 This teaching strategy can be easily incorporated into undergraduate radiology training and enables students to acquire skills in understanding, reasoning and a further appreciation of radiological diagnosis.36 Gamification is an alternative educational approach that encourages student motivation and participation in the learning process through the use of games, and has proven effective in undergraduate and postgraduate diagnostic radiology training.37 When integrating these methods into radiology training, diagnostic reasoning should be included as one of the central objectives, thereby making them more attractive at the same time as favouring the development of clinical judgement in students.33
Education is undergoing a digital transformation, giving rise to new learning tools. The use of e-learning in medical school teaching is on the rise, enabling both real-time interaction with teachers and asynchronous activities that allow students to learn at their own pace. Advances in technology and the Picture Archiving and Communication Systems (PACS), as well as access to radiological images, mean that it has never been easier to illustrate living anatomy and clinical pathology in exceptional detail to students.3 Computer programmes that simulate routine work are available and can be used to learn to recognise anatomical structures and pathological patterns, as well as ultrasound and interventional radiology, maximising patient safety.33 It is most cost-effective to employ blended learning strategies integrating traditional face-to-face teaching sessions with synchronous or asynchronous e-learning to support and enhance interactions between students, teachers and e-resources.34 There are also excellent websites for studying radiology, the use of which has increased since the COVID-19 pandemic,38 and social networks appear to have an interesting role to play in radiology education, suited to the habits of today's students.39,40
LimitationsOur study has some limitations, which are described below. The analysis of teaching hours and subjects in which diagnostic radiology is taught has been based on published curricula, but the way these curricula are actually delivered has not been confirmed, meaning it is possible that differences exist that we have not identified. Our study has not established the number of hours spent on practical placements, nor the methodology used in diagnostic radiology teaching in the different medical schools. These issues will be addressed in future studies that quantify in depth the different radiology teaching models used. It is also necessary to determine the current number of radiology lecturers at each faculty, both overall and by category, and the number of hours of radiology teaching carried out by non-radiologist medical professionals.
Institutions, universities and medical schools are all aware that we are heading towards a new training model for doctors, with new tools, more clinical practice and simulation elements. We need to be present in the decision-making process as radiologists and take the opportunity to have a say in the changes that are on the horizon.
ConclusionThe current situation of radiology training in medical studies is characterised by its rather heterogeneous nature in terms of the extent to which diagnostic radiology is present and the way in which teaching is organised. The number of university lecturers specialising in diagnostic radiology per medical school is decreasing. This trend is accompanied by a shortage of clinical university lecturers and the short-term need to replenish teaching posts with younger staff. The current situation poses a number of challenges, described throughout the text, including the need to adapt to new teaching methods and technologies, the need to promote the presence of radiology in medical curricula and the need to raise the profile of the specialty among future doctors.
FundingFunding of Open Access charges: University of Malaga/CBUA.
Author contributions- 1.
Accountable for the integrity of the study: FSP, DDP and MSB.
- 2.
Study conception: FSP, DDP and MSB.
- 3.
Study design: FSP.
- 4.
Data acquisition: FSP and MSB.
- 5.
Data analysis and interpretation: FSP, DDP and MSB.
- 6.
Statistical analysis: N/A.
- 7.
Literature search: FSP and DDP.
- 8.
Drafting of article: FSP and MSB.
- 9.
Critical review for important intellectual content: FSP, DDP and MSB.
- 10.
Approval of final version: FSP, DDP and MSB.
The authors declare that they have no conflicts of interest.