The aim of this study was to analyze risk factors for nosocomial infection (NI) in patients receiving extracorporeal membrane oxygenation (ECMO) support.
Patients and methodsClinical NI data were collected from patients who received ECMO support therapy, and analyzed retrospectively.
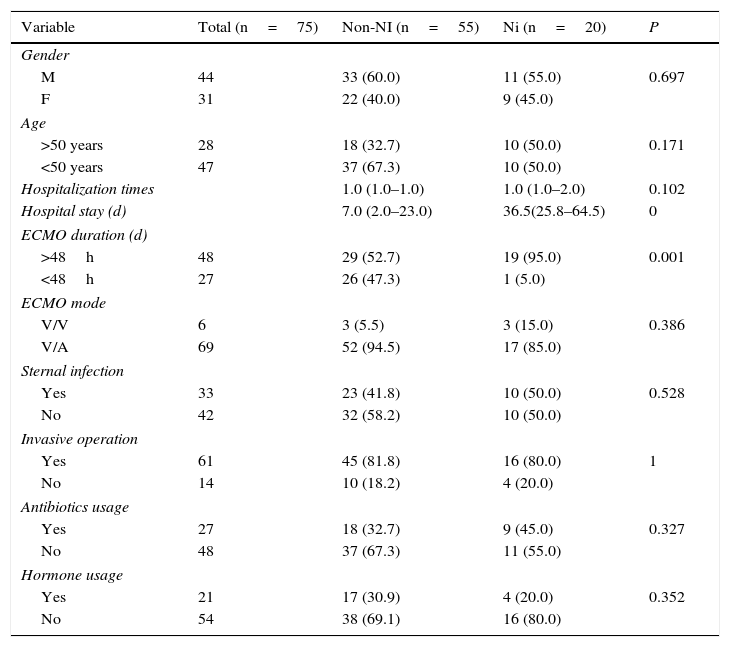
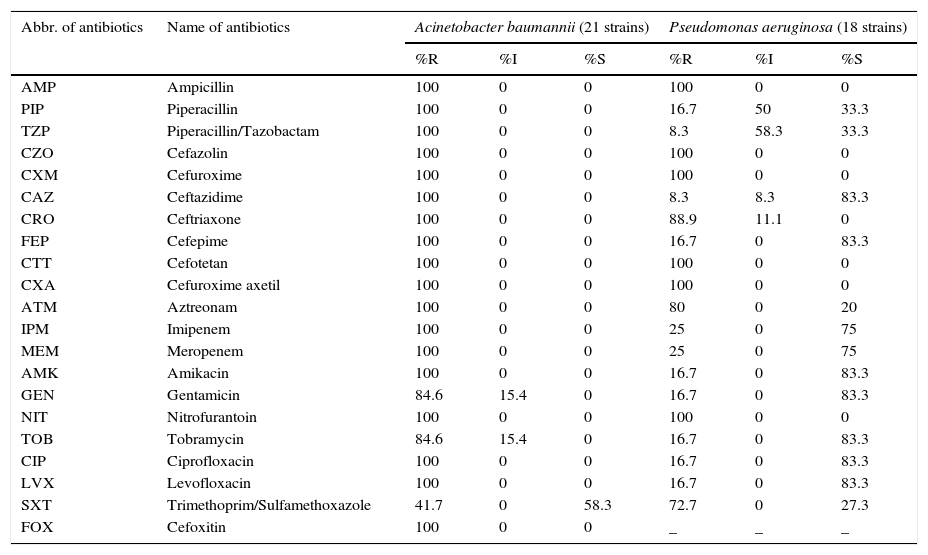
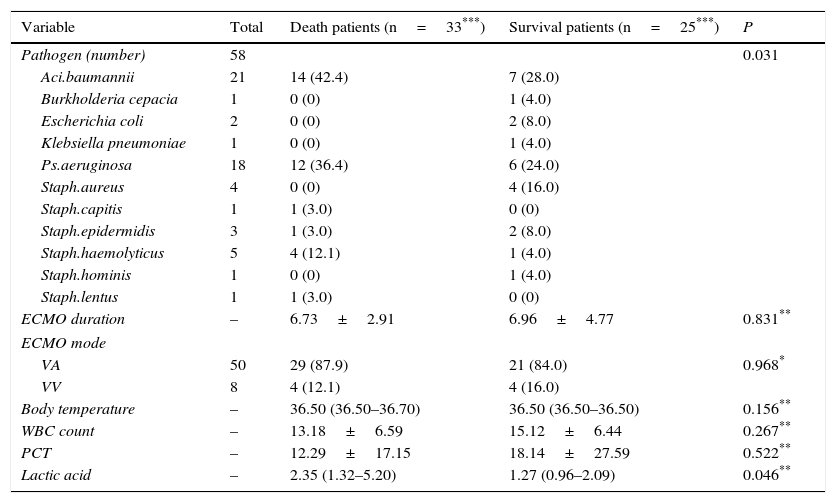
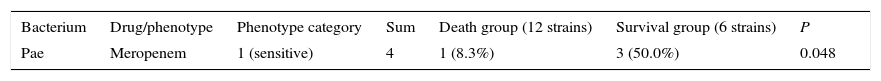
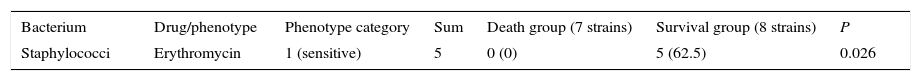
ResultsAmong 75 ECMO patients, 20 were found to have developed NI (infection rate 26.7%); a total of 58 pathogens were isolated, including 43 strains of gram-negative bacteria (74.1%) and 15 strains of gram-positive bacteria (25.9%). Multi-drug resistant strains were highly concentrated and were mainly shown to be Acinetobacter baumannii, Pseudomonas aeruginosa, and coagulase-negative staphylococci. Incidence of NI was related to the duration of ECMO support therapy and the total length of hospital stay, and the differences were statistically significant (P<0.05). A prolonged period of ECMO support extended the hospital stay, but it did not increase the mortality rate. However, an elevated level of lactic acid increased the mortality rate in this study population.
ConclusionsECMO-associated secondary NIs correlated significantly with the length of hospital stay and with the duration of ECMO support. Therefore, to reduce the incidence of ECMO-associated NIs, preventive strategies that aim to shorten the duration of ECMO support therapy and avoid lengthy hospitalization should be applied, wherever possible.
El objetivo de este estudio fue analizar los factores de riesgo de la infección nosocomial (IN) en pacientes que reciben soporte de extracorporeal membrane oxygenation (ECMO, «oxigenación por membrana extracorpórea»).
Pacientes y métodosSe recolectaron los datos clínicos de las IN de los pacientes que recibieron tratamiento de soporte ECMO, analizándose retrospectivamente.
ResultadosEntre los 75 pacientes con ECMO, se encontró que 20 habían desarrollado IN (tasa de infección del 26,7%), aislándose un total de 58 patógenos, incluyendo 43 cepas de bacterias gramnegativas (74,1%) y 15 cepas de bacterias grampositivas (25,9%). Las cepas resistentes a múltiples fármacos se hallaban altamente concentradas, componiéndose principalmente de Acinetobacter baumannii, Pseudomonas aeruginosa y estafilococos coagulasa negativos. La incidencia de IN se relacionó con la duración del tratamiento de soporte ECMO y la estancia hospitalaria total, siendo las diferencias estadísticamente significativas (p<0,05). Un período prolongado de soporte ECMO ampliaba la estancia hospitalaria, aunque no incrementaba la tasa de mortalidad. Sin embargo, la elevación del nivel de ácido láctico incrementaba la tasa de mortalidad en esta población de estudio.
ConclusionesLas IN secundarias asociadas a ECMO guardaron una correlación considerable con la duración de la estancia hospitalaria y la duración del soporte ECMO. Por tanto, para reducir la incidencia de las IN asociadas a ECMO, deberán aplicarse estrategias en aras de reducir la duración del tratamiento de soporte ECMO y evitar la hospitalización prolongada, cuando ello sea posible.