At the beginning of the pandemic, the interaction between HIV and COVID-19 became a concern among researchers, given the higher mortality of patients living with HIV (PLWH) during seasonal flu.1 However, subsequent studies proved to be conflicting, because some authors suggest that immunosuppression may favor infection by the COVID-19 virus, while others suggest that low CD4 counts may reduce the deleterious systemic inflammatory response (SIRS) in patients infected with SARS-COV-2.2
Faced with a clinical condition as complex as that caused by HIV, dealing with the unknown SARS-COV-2 virus has become an even greater challenge, for those who contract both infections and for the health professionals who coordinate the care for patients. Thus, the purpose of this scientific letter is to describe the clinical presentation, laboratory data, and mortality rate observed in adult patients admitted to a referral unit in Recife, Brazil.
This is a retrospective observational case series study that included all adult patients with laboratory-confirmed co-infection by SARS-COV-2/HIV hospitalized at a referral unit between March 2020 and March 2021. We compiled all patients’ demographics, clinical, treatment, and laboratory data. The project was approved by the local ethics committee.
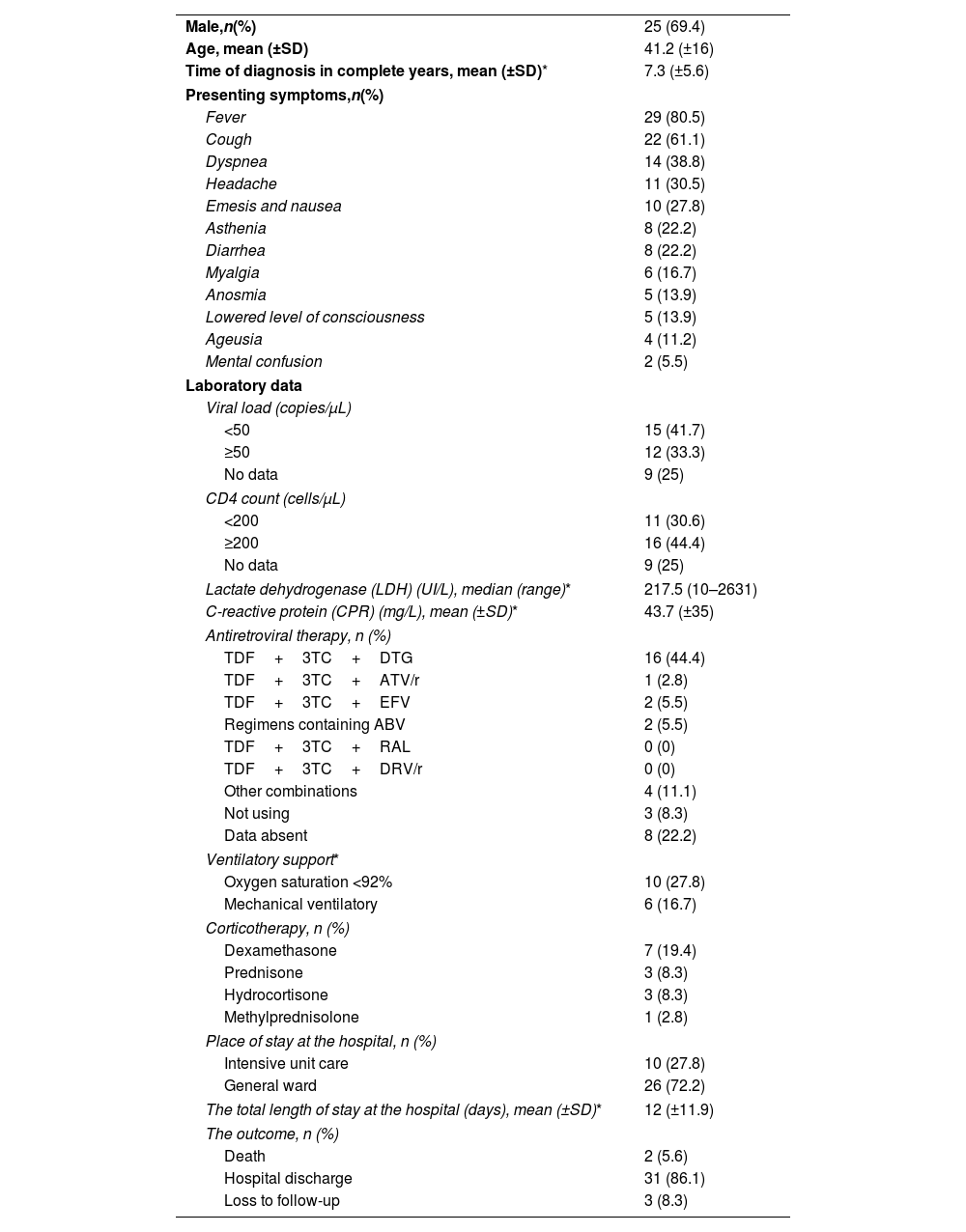
Included 36 patients, the majority (69.4%) being male, with a mean age of 41.2 years (±16). The mean time of diagnosis of HIV infection was 7.3 years (±5.6). Fever (80.5%), cough (61.1%), and dyspnea (38.8%) were the most prevalent symptoms after COVID-19 infection. A systematic review reported similar results and there are no differences in the symptomatology between PLWH and the general population.3
About 70% of patients were using antiretroviral therapy (ART) and more than 90% survived. The regimens utilized are described in Table 1. ART restores concentrations of interferon, cytokines, and chemokines. Although the evidence is limited, it is known that the repair of concentrations of interferon may be advantageous for responses to COVID-19.4 The viral load (VL) data of 25% of the patients were not collected during hospitalization. More than 50% of the individuals who had the data described had adequate virological control with VL below the limit of detection at the time of co-infection with SARS-COV-2.
Characteristics of the studied population (n=36).
| Male,n(%) | 25 (69.4) |
| Age, mean (±SD) | 41.2 (±16) |
| Time of diagnosis in complete years, mean (±SD)* | 7.3 (±5.6) |
| Presenting symptoms,n(%) | |
| Fever | 29 (80.5) |
| Cough | 22 (61.1) |
| Dyspnea | 14 (38.8) |
| Headache | 11 (30.5) |
| Emesis and nausea | 10 (27.8) |
| Asthenia | 8 (22.2) |
| Diarrhea | 8 (22.2) |
| Myalgia | 6 (16.7) |
| Anosmia | 5 (13.9) |
| Lowered level of consciousness | 5 (13.9) |
| Ageusia | 4 (11.2) |
| Mental confusion | 2 (5.5) |
| Laboratory data | |
| Viral load (copies/μL) | |
| <50 | 15 (41.7) |
| ≥50 | 12 (33.3) |
| No data | 9 (25) |
| CD4 count (cells/μL) | |
| <200 | 11 (30.6) |
| ≥200 | 16 (44.4) |
| No data | 9 (25) |
| Lactate dehydrogenase (LDH) (UI/L), median (range)* | 217.5 (10–2631) |
| C-reactive protein (CPR) (mg/L), mean (±SD)* | 43.7 (±35) |
| Antiretroviral therapy, n (%) | |
| TDF+3TC+DTG | 16 (44.4) |
| TDF+3TC+ATV/r | 1 (2.8) |
| TDF+3TC+EFV | 2 (5.5) |
| Regimens containing ABV | 2 (5.5) |
| TDF+3TC+RAL | 0 (0) |
| TDF+3TC+DRV/r | 0 (0) |
| Other combinations | 4 (11.1) |
| Not using | 3 (8.3) |
| Data absent | 8 (22.2) |
| Ventilatory support* | |
| Oxygen saturation <92% | 10 (27.8) |
| Mechanical ventilatory | 6 (16.7) |
| Corticotherapy, n (%) | |
| Dexamethasone | 7 (19.4) |
| Prednisone | 3 (8.3) |
| Hydrocortisone | 3 (8.3) |
| Methylprednisolone | 1 (2.8) |
| Place of stay at the hospital, n (%) | |
| Intensive unit care | 10 (27.8) |
| General ward | 26 (72.2) |
| The total length of stay at the hospital (days), mean (±SD)* | 12 (±11.9) |
| The outcome, n (%) | |
| Death | 2 (5.6) |
| Hospital discharge | 31 (86.1) |
| Loss to follow-up | 3 (8.3) |
TDF: tenofovir; 3TC: lamivudine; DTG: dolutegravir; ATV/r: atazanavir; RAL: raltegravir; DRV/r: darunavir; EFV: efavirenz; ABV: abacavir.
As for the CD4+ T lymphocyte count, 11 patients (30.6%) had values less than 200cells/μL, which may be associated with lower overall survival, as it configures severe immunosuppression. In this regard, about 30% of these patients required admission to the ICU with the mean total length of stay at the hospital being 12 days (±11.9). Three patients (8.3%) were lost to follow-up due to transfer or hospital evasion. Two patients (5.6%) died, one of them dropped out of treatment and has VL ≥50copies/μL and CD4 count <200cells/μL. The other patient had a recent diagnosis and was not yet using ART, in addition to not having a VL and CD4 result.
All individuals diagnosed more than 10 years ago were cured of COVID-19. SARS-COV-2 virus seems to develop mechanisms to contain the interferon immune response. Consequently, patients with worse prognosis have interferon pathways less active. PLWH in the acute phase, to maintain control over the viral replication, also targets interferon. In contrast, in the course of chronic disease, there are high concentrations of interferon, with a gene stimulus for its production. Thus, we can infer that long-standing HIV may be favorable to controlling COVID-19.4
Lymphocytopenia caused by HIV would be responsible for a delay in the seroconversion and consequent impairment in the production of antibodies so that the T lymphocyte CD4+ would be a key player in the activation of B lymphocytes, followed by an adequate immune response to SARS-COV-2.5 Therefore, COVID-19/HIV co-infection would not be a protective factor, since inflammatory cytokines would not be in a leading position. More studies are needed to conclude which is the intersection between the pathogens and the immune system, as well as the consequences of such interaction for the infected organism.
In the present study, co-infected patients had a clinical presentation similar to that described in previously published studies, which does not differ from the symptoms presented by the general population. The clinical course was favorable in most patients, with a low mortality rate and predominant care in the general ward.
Ethical approvalThe local ethics committee approved the project (consubstantiated opinion no. 4,995,059) and the need to obtain informed consent was waived, as it was a retrospective study using medical records, without interfering with the care provided to the individual.
FundingThis research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestWe have no conflicts of interest to disclose.