The under-utilisation of taps is associated with the generation of reservoirs of non-fermenting gram-negative bacilli with the ability to disseminate. We describe the detection and approach of the problem in an ICU.
MethodsObservational descriptive study in an ICU with individual cubicles with their own sink. We collected clinical samples from patients and environmental samples from tap aerators and reviewed the unit's hygiene measures.
ResultsWe detected four cases due to Chryseobacterium indologenes, one to Elizabethkingia meningoseptica and another to Pseudomonas aeruginosa; they were identified both in clinical and the environmental samples. The healthcare professionals reported that almost every hand hygiene opportunity was performed with a hydroalcoholic solution. After considered the daily flushing of water outlets as inefficient, it was decided to remove them.
ConclusionsNational recommendations were insufficient for preventing, detecting and controlling tap contamination in units with a high risk of infection. The management of taps in these units needs to be improved.
La infrautilización de grifos se relaciona con reservorios de bacilos gramnegativos no fermentadores en su interior con capacidad de diseminación. Se describe la detección del problema y abordaje en una UCI.
MétodosEstudio descriptivo en una UCI con boxes individuales con lavabo propio. Se recogieron muestras clínicas de pacientes y ambientales de los aireadores de los grifos. Se revisaron medidas de higiene.
ResultadosSe identificaron 4 casos de Chryseobacterium indologenes, uno de Elizabethkingia meningoseptica y otro por Pseudomonas aeruginosa, tanto en muestras clínicas como ambientales. Los profesionales indicaron utilizar solución hidroalcohólica casi siempre en la higiene de manos. Tras descartar la apertura controlada diaria de grifos por ineficiente, se decidió su retirada.
ConclusionesLas recomendaciones nacionales resultaron insuficientes para la prevención, detección y control de la contaminación de los grifos de una unidad de alto riesgo de infección. Es necesario mejorar el manejo de los grifos en estas unidades.
Health care-related infections are the second most frequent adverse event during care, after medication errors.1 The latest data from the EPINE study2 show that they affect 7.92% of patients admitted to a hospital, with non-fermenting gram-negative bacilli (NFGNB) being the third most frequent group of microorganisms. They behave like opportunistic pathogens with diverse capacity of dissemination and clinical relevance.3,4
Due to their low requirements and chlorine resistance of some of its types,4 the role that tap aerators can play as reservoirs of NFGNB in units with patients at high risk of infection and that are not monitored in water quality samples for human consumption has been noted.5–7 In addition, the increased number of sinks in these units, accompanied by the diffusion of hydroalcoholic solutions for hand hygiene, favours the underuse of the former with stagnation of water and formation of biofilms8; therefore, measures have been proposed, such as the daily opening of taps that are used infrequently in these units, for their prevention.9
The objective of this work is to describe the detected cases that contributed to the identification of the problem and its approach in an intensive care unit (ICU).
MethodsDescriptive study, whose period is subdivided into 2, one of surveillance of a group of cases of Chryseobacterium indologenes between January and April 2015, whose index case is declared by the intensive care workers to the Preventive Medicine Department for review of special precautions, and another of surveillance of sporadic cases initiated in the same way as a result of the identification of a case of Elizabethkingia meningoseptica in November 2015 and until March 2016, when a case of Pseudomonas aeruginosa was detected. The attack rate was calculated on patients admitted to the ICU during the first period.
The centre studied has an ICU with 8 individual boxes, with its own sink and a surveillance system for microorganisms of epidemiological interest among the Microbiology and Preventive Medicine Departments. The ICU adheres to the national Zero Resistance initiative,10 which means that weekly screening samples of multi-resistant micro-organisms are carried out in the unit, including bronchial aspiration, which was the nosocomial infection/colonisation index location in all cases. Age, sex, week of stay, intrinsic and extrinsic risk factors of infection/colonisation2 and presence of nebulised therapy of patients were collected.
Environmental samples were collected by vortexing the aerators of the taps in sterile physiological serum for 5min, one of the ICU box in which the last 2 cases of the first period arose, and in all the boxes, medication preparation room, living room and rubbish tip, before each of the 2 cases of the second period, 11 locations in total.
All samples were seeded on Trypticase Soy agar+5% sheep blood (TSS), PolyViteX chocolate agar (PVX) and MacConkey agar. The TSS and PVX agar were incubated for 48h in a 37°C oven with 5% CO2, while the MacConkey agar was incubated in an oven at 37°C without CO2. Each plate was checked at 24h of incubation. The identification at the species level of the microorganisms isolated in the study was carried out using the mass spectrometry technique (VITEK MS, Biomerieux) based on the MALDI-TOF. In all the isolates, identification results were obtained with a confidence value of 99.9%, and antibiotic sensitivity studies were carried out based on the Kirby Bauer agar disk diffusion method.
Coinciding with the last case of the first period, controls of water in the consumer's tap were requested from the 8 boxes to the accredited external laboratory with which the hospital performs the water self-monitoring,7 which were repeated at 24h to verify the effectiveness of the corrective action carried out (thermal shock of terminal points and cleaning/disinfection of taps with refill of diffusers of all the boxes), together with sampling of entry point to the centre and points distal to the ICU.
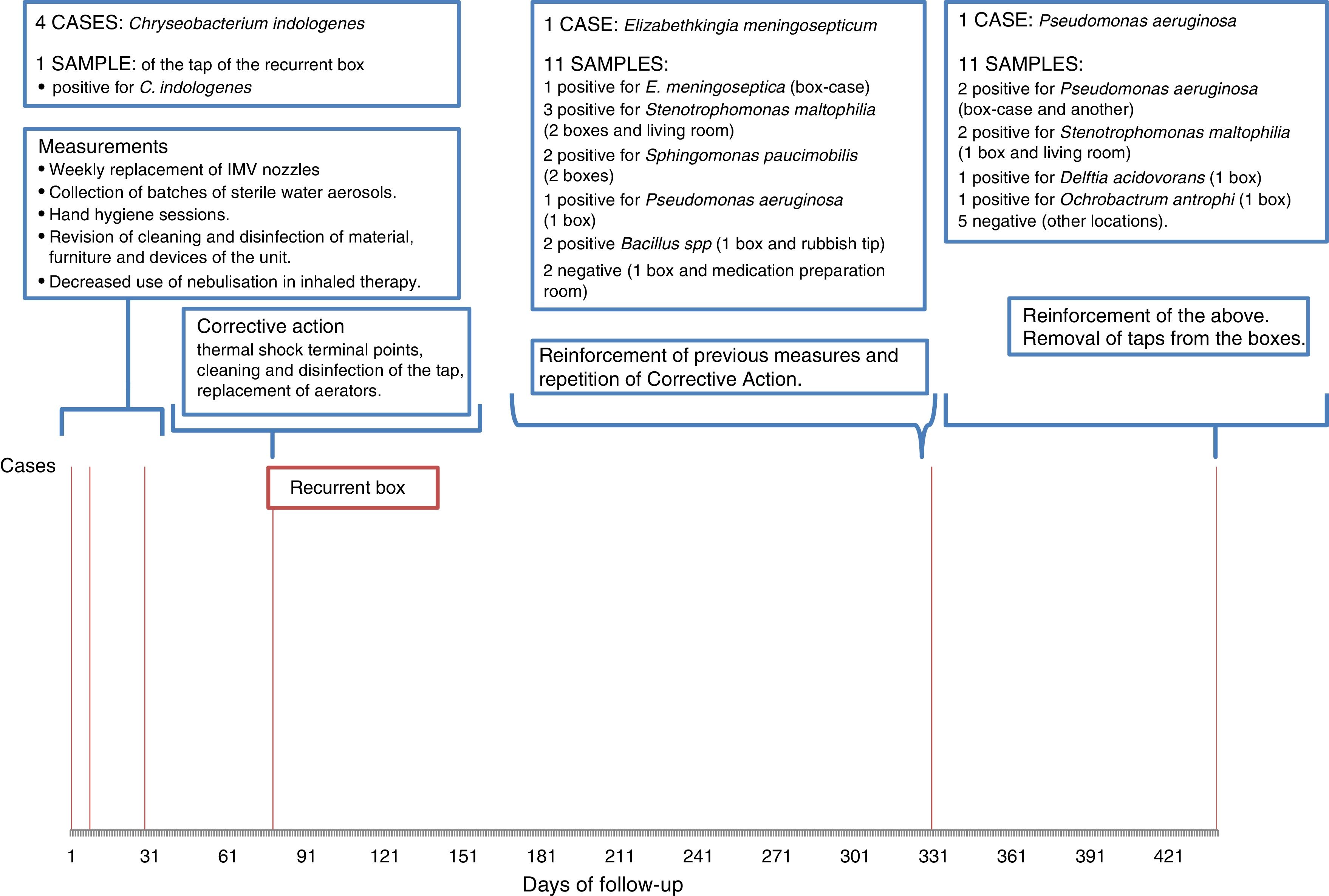
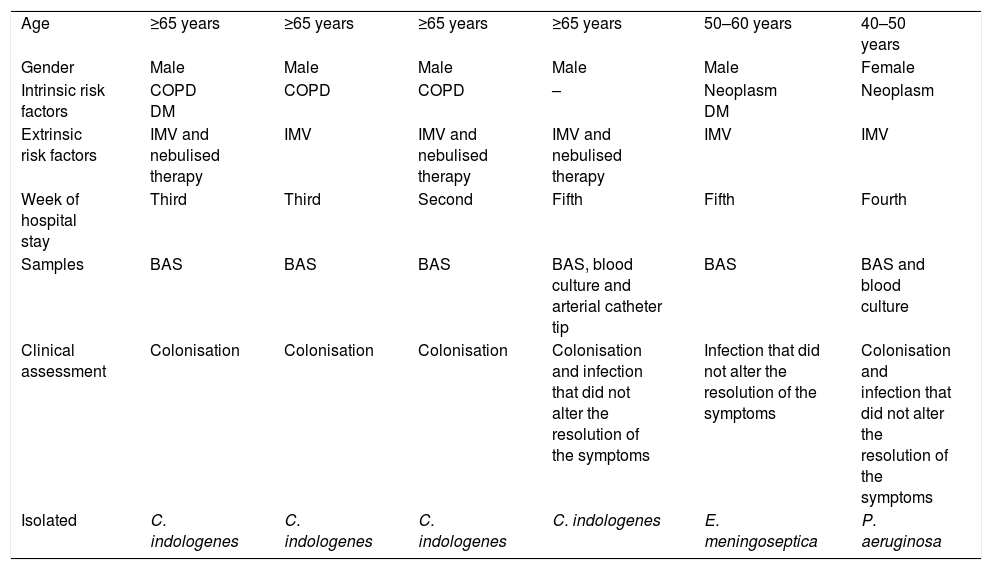
ResultsTable 1 summarises the characteristics of the cases and Fig. 1 its chronology, listing of results of environmental samples by locations and control actions.
Characteristics of patients who presented with infection/colonisation by NFGNB.
| Age | ≥65 years | ≥65 years | ≥65 years | ≥65 years | 50–60 years | 40–50 years |
| Gender | Male | Male | Male | Male | Male | Female |
| Intrinsic risk factors | COPD DM | COPD | COPD | – | Neoplasm DM | Neoplasm |
| Extrinsic risk factors | IMV and nebulised therapy | IMV | IMV and nebulised therapy | IMV and nebulised therapy | IMV | IMV |
| Week of hospital stay | Third | Third | Second | Fifth | Fifth | Fourth |
| Samples | BAS | BAS | BAS | BAS, blood culture and arterial catheter tip | BAS | BAS and blood culture |
| Clinical assessment | Colonisation | Colonisation | Colonisation | Colonisation and infection that did not alter the resolution of the symptoms | Infection that did not alter the resolution of the symptoms | Colonisation and infection that did not alter the resolution of the symptoms |
| Isolated | C. indologenes | C. indologenes | C. indologenes | C. indologenes | E. meningoseptica | P. aeruginosa |
BAS: bronchoaspiration; COPD: chronic obstructive pulmonary disease; DM: diabetes mellitus; IMV: invasive mechanical ventilation.
During the period of grouped cases of C. indologenes a total of 91 patients were admitted to the ICU with an average age of 59.8 years (SD: 16.3) and a median of days of stay 2 (IQR: 1–4). 54% were men and 46% women. Four cases appeared, with the attack rate being 4.4%.
C. indologenes was isolated in the tap aerator sample from the same box that housed the last 2 cases and coliforms were isolated in consumer water tap samples both in this and in another box in which there were no cases. The other parameters were appropriate. After the corrective action, all the consumer water tap sample verification tests performed were negative for coliforms.
During the period of sporadic cases, a first case was presented with E. meningoseptica, also being identified in the tap sample of its box. In the rest of the locations, 6 more positive for NFGNB and 2 positive for Bacillus spp. were found, not being identified in patient samples. The second case presented P. aeruginosa that was isolated in the tap of its box, with NFGNB being found in 5 more locations that were also not identified in patient samples.
DiscussionThe approach to control the group of cases of C. indologenes was aimed at eliminating reservoirs in wet medical devices,4 cleaning/disinfection reinforcement and standard precautions, which has resolved similar situations documented for Chryseobacterium spp.11,12 The intensification of these measures could contribute to the distancing of cases, but recurrence in the same box led to a belief of the taps as a reservoir5,6 and in addition to consumer tap sample controls (thinking of an origin prior to the ICU) it was decided to sample its aerator, resulting in the identification of C. indologenes and the final control after cleaning/disinfection of taps with replacement of diffusers.
The absence of coliforms in the input samples to the centre as well as points distal to the ICU limited its presence to the 2 boxes mentioned, attributing its appearance to an external contamination of the tap during some use of hygiene or cleaning.9
The appearance of a case of E. meningoseptica (formerly Chryseobacterium meningosepticum), whose isolation in clinical samples is documented as being strongly associated with the contamination of taps,5 gave rise to a new surveillance period accompanied by corrective action, verifying that the cleaning and disinfection of ICU taps will be carried out monthly as recommended in units at high risk for control of Legionella.13
The discussion of these findings with professionals revealed that the taps of the boxes were hardly used because almost all hand hygiene opportunities are done with hydroalcoholic solution, which favours the formation of biofilms,8,9 a fact consistent with the negativity of the 2 samples from the medication preparation room, which was identified as the unit's most used tap. Although there may still be hidden reservoirs (including the drains themselves and siphons of the sinks14) and there are limitations to directly relating the contaminations with the infections/colonisations detected, the need to work on these underused taps was made clear.8 After dismissing its daily preventive opening9 for being inefficient (a frequency higher than the recommended weekly opening for the prevention of Legionella15), coinciding with the case of P. aeruginosa, the definitive withdrawal of the taps from the boxes was decided without identifying new cases until the writing of this article.
Despite the low pathogenic capacity of C. indologenes, its persistence was used to initiate the surveillance. Although none of the isolates altered the clinical resolution of the patients, the consequences could have been serious, given the greater potential impact of the other NFGNB as well as the rest of isolates in taps and not in patients (e.g. Stenotrophomonas maltophilia).2,4 The prevention measures and samples of Legionella or quality of water for human consumption recommended in Spain were insufficient for the surveillance and prevention of health care-related infections by NFGNB in a unit with a high risk of infection. The collection of samples for the “Zero Resistance” project implemented in the unit has been useful for the identification of the problem in patients and for proposing a surveillance aimed at its resolution, whilst simultaneously allowing for the effectiveness of the actions performed to be evaluated.
FundingNone declared.
Conflicts of interestNone declared.
To Carolina Giráldez-García for her great work coordinating the measurements.
Please cite this article as: de-las-Casas-Cámara G, Martín-Ríos MD, Adillo-Montero MI, Muñoz-Egea MC, Zapardiel-Ferrero J, Pérez-Jorge Peremarch C. La infrautilización de grifos en una unidad de cuidados intensivos como causa de reservorios de bacilos gramnegativos no fermentadores. Enferm Infecc Microbiol Clin. 2018;36:214–217.