Rupture of cruciate ligaments of the knee is a common injury that is repaired by arthroscopic reconstruction, which can give rise to septic arthritis. The objective of this article is to describe the clinical and microbiological aspects of this entity.
MethodsRetrospective review of cases of septic arthritis following arthroscopic reconstruction of cruciate ligaments of the knee that occurred at a single institution from 2000 to 2015. According to time elapsed from surgery, infections were classified as acute (<14 days), subacute (>14 days and <30 days), and late (>30 days). A descriptive and comparative analysis stratified by type of infection and causative microorganism was performed.
Results3219 patients underwent arthroscopic reconstruction of cruciate ligaments of the knee and 30 (0.9%) developed septic arthritis. Seventeen (57%) were acute infections and 12 (40%) subacute; there was one late infection. The causative microorganisms were coagulase-negative Staphylococci (n=13; 43%), Staphylococcus aureus (n=12; 40%), other Gram positive cocci (n=3; 10%), and Gram negative bacilli (n=2; 7%). All patients underwent arthroscopic debridement; no grafts were removed. All patients received antibiotic therapy for a median of 23.5 days (range: 14–78 days); all infections were cured. No significant differences were found in any of the variables analysed among the infection type or the causative microorganism.
ConclusionsSeptic arthritis after arthroscopic reconstruction of cruciate ligaments of the knee is uncommon. It generally presents within 4 weeks of surgery and is caused by Staphylococci. Its treatment consists of arthroscopic debridement (without necessarily removing the graft) and antibiotic therapy.
La rotura de los ligamentos cruzados de la rodilla es frecuente y se repara mediante ligamentoplastia artroscópica. Entre sus complicaciones está la artritis séptica. El objetivo de este trabajo es describir las características clínicas y microbiológicas de esta entidad.
MétodosRevisión retrospectiva de casos de artritis séptica tras ligamentoplastia de rodilla ocurridos en una institución durante los años 2000–2015. Según los días transcurridos desde la ligamentoplastia, la infección se consideró aguda (< 14 días), subaguda (> 14 días y<30 días) o tardía (> 30 días). Se realizó un análisis descriptivo y comparativo, estratificado según el tipo de infección y microorganismo causante.
ResultadosSe intervinieron 3.219 pacientes; 30 (0,9%) desarrollaron artritis séptica. Diecisiete (57%) infecciones fueron agudas, 12 (40%) subagudas y una tardía. Los microorganismos causantes fueron Staphylococcus coagulasa-negativos (n=13; 43%), Staphylococcus aureus (n=12; 40%), otros cocos grampositivos (n=3; 10%) y bacilos gramnegativos (n=2; 7%). Se realizó desbridamiento artroscópico en todos los casos; en ninguno fue necesario retirar la plastia. Los pacientes recibieron tratamiento antibiótico durante una mediana de 23,5 días (rango, 14 – 78 días); todas las infecciones se curaron. No se evidenciaron diferencias significativas en ninguna de las variables analizadas entre el tipo de infección o el microorganismo responsable.
ConclusionesLa artritis séptica es una complicación poco frecuente de la ligamentoplastia de rodilla. Se manifiesta generalmente dentro de las 4 semanas después de la cirugía y está causada por Staphylococcus. El tratamiento consiste en desbridamiento artroscópico precoz (pudiendo no ser necesario retirar la plastia) y antibioterapia.
Rupture of the cruciate ligaments of the knee is a common injury which is currently repaired by arthroscopic anterior cruciate ligament reconstruction.1 Its complications include septic arthritis, with an incidence which ranges from 0.1% to 2.6%.2–5 The series on this complication of anterior cruciate ligament reconstruction of the knee are published in the surgical literature and provide few microbiological details. This article presents a review of cases of septic arthritis following anterior cruciate ligament reconstruction of the knee, focusing on the clinical and microbiological aspects of this entity.
MethodsRetrospective review of the medical records of patients with septic arthritis following anterior cruciate ligament reconstruction of the knee which occurred between 2000 and 2015 at our institution. Cases were considered to be patients who underwent anterior cruciate ligament reconstruction of the knee with symptoms/signs of arthritis and positive culture from synovial fluid. The variables collected were: age, gender, co-existing conditions, previous surgery in the same knee, preoperative antibiotic prophylaxis, duration of the surgery, symptoms, days elapsed from the surgery until the onset of arthritis symptoms, days elapsed from the surgery until the date of diagnosis of septic arthritis, leukocyte count, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) in blood, isolated microorganism in synovial fluid, antibiotic therapy and surgical procedure performed, duration of hospital stay and outcome. For the calculation of the time intervals, the date of diagnosis of septic arthritis was established as that in which the sample of synovial fluid with a positive culture was obtained. According to the days elapsed from the anterior cruciate ligament reconstruction until the onset of symptoms/signs of arthritis, the infection was considered acute (≤14 days), sub-acute (>14 days and ≤30 days) or delayed (>30 days).
A descriptive analysis was carried out of the patient characteristics, clinical variables (including the treatment received and aspects related to the surgical intervention), type of microorganism isolated in the synovial fluid cultures and laboratory data in blood and synovial fluid. For the comparative analysis, the frequencies and percentages were calculated, stratified by the type of infection (acute, sub-acute, delayed) and by the microorganism isolated in the synovial fluid. The chi-square test was used to evaluate the significance of the differences (p value <0.05) found in the different groups. Finally, to analyse the effect of the treatment with rifampicin, the median and the 25th (P25) and 75th (P75) percentiles of the time elapsed (in days) from the onset until the end of the antibiotic treatment and of the duration of the hospital stay were compared.
ResultsPatients and arthroscopic surgeryDuring the study period, 3219 patients underwent anterior cruciate ligament reconstruction of the knee at our institution. Thirty (0.9%) developed septic arthritis: 28 were male and two female (median age: 33 years; range: 21–54 years). In nine cases (30%), isolated anterior cruciate ligament reconstruction had been performed and in 21 cases (70%), additional procedures had been performed during the arthroscopic surgery. Eight patients (27%) had undergone previous surgery of the affected knee, one patient was receiving corticosteroids and another was diabetic. Twenty-eight patients (93%) received preoperative antibiotic prophylaxis with cefazolin (n=24), erythromycin (n=3) or vancomycin (n=1); in two cases no information about the antibiotic prophylaxis used was available. Antibiotic prophylaxis was started in the operating theatre before the induction of anaesthesia and was maintained until the removal of the drains.
Clinical manifestationsThe symptoms developed a median of 12 days (range, 3–35 days) after the anterior cruciate ligament reconstruction and included joint effusion in 30 patients (100%), pain in 29 (97%), local heat in 27 (90%), febricula/fever in 25 (83%) and purulent exudate through the arthroscopy portals in 5 (17%). Arthrocentesis which established the diagnosis of septic arthritis was performed a median of four days (range, 0–12 days) after the onset of symptoms. Seventeen infections (57%) were acute, 12 (40%) were sub-acute and one was delayed.
MicrobiologyIn the synovial fluid cultures, Gram-positive cocci were isolated in 28 patients (93%): coagulase-negative Staphylococci (CoNS) in 13 cases (43%), Staphylococcus aureus (S. aureus) in 12 cases (40%), Enterococcus faecalis in two cases (6.7%) and Streptococcus agalactiae in one case (3.3%). Gram-negative bacilli were isolated in two patients (7%): Serratia marcescens in one case (3.3%) and Enterobacter cloacae in one case (3.3%). Nine strains (75%) of S. aureus and seven strains (40%) of CoNS were methicillin-resistant.
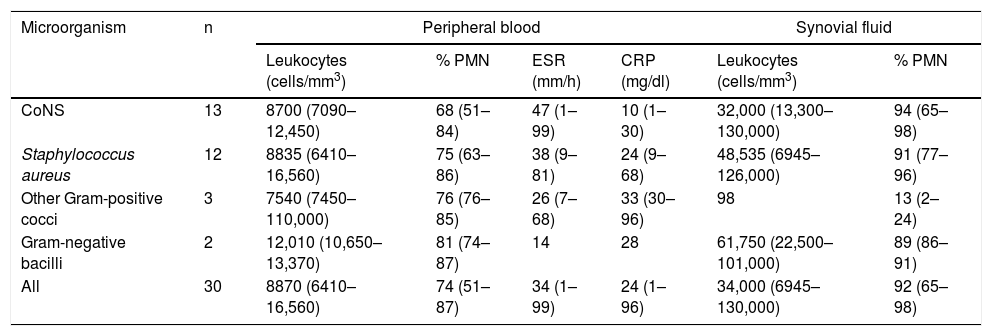
Laboratory testsThe results of the blood and synovial fluid analysis are shown in Table 1. Seven patients (23%) had >10,800leukocytes/mm3 in peripheral blood. The ESR was high (>15mm/h) in 18 (75%) of the 24 cases in which this parameter was measured. C-reactive protein was high (>0.5mg/dl) in 13 (93%) of the 14 patients in which this parameter was measured. The cell count in synovial fluid was <50,000cells/mm3 in 17 (63%) of the 27 patients in which this parameter was measured.
Laboratory results (median and range) according to the causative microorganism of septic arthritis.
| Microorganism | n | Peripheral blood | Synovial fluid | ||||
|---|---|---|---|---|---|---|---|
| Leukocytes (cells/mm3) | % PMN | ESR (mm/h) | CRP (mg/dl) | Leukocytes (cells/mm3) | % PMN | ||
| CoNS | 13 | 8700 (7090–12,450) | 68 (51–84) | 47 (1–99) | 10 (1–30) | 32,000 (13,300–130,000) | 94 (65–98) |
| Staphylococcus aureus | 12 | 8835 (6410–16,560) | 75 (63–86) | 38 (9–81) | 24 (9–68) | 48,535 (6945–126,000) | 91 (77–96) |
| Other Gram-positive cocci | 3 | 7540 (7450–110,000) | 76 (76–85) | 26 (7–68) | 33 (30–96) | 98 | 13 (2–24) |
| Gram-negative bacilli | 2 | 12,010 (10,650–13,370) | 81 (74–87) | 14 | 28 | 61,750 (22,500–101,000) | 89 (86–91) |
| All | 30 | 8870 (6410–16,560) | 74 (51–87) | 34 (1–99) | 24 (1–96) | 34,000 (6945–130,000) | 92 (65–98) |
CoNS: coagulase-negative staphylococci; CRP: C-reactive protein; ESR: erythrocyte sedimentation rate; PMN: polymorphonuclear leukocytes.
In all cases, arthroscopic debridement was performed after diagnosis (median: 0 days; range, 0–20 days). In 17 patients (57%), the debridement was performed on the same day on which septic arthritis was diagnosed. In 22 cases (73%), a single debridement was sufficient, six patients required two and two patients required three debridements. In 28 cases, information about the state of the graft was available: normal in 18 cases (64%), partially broken in six cases (20%) and loose in four cases (13%); it was not necessary to remove it in any case.
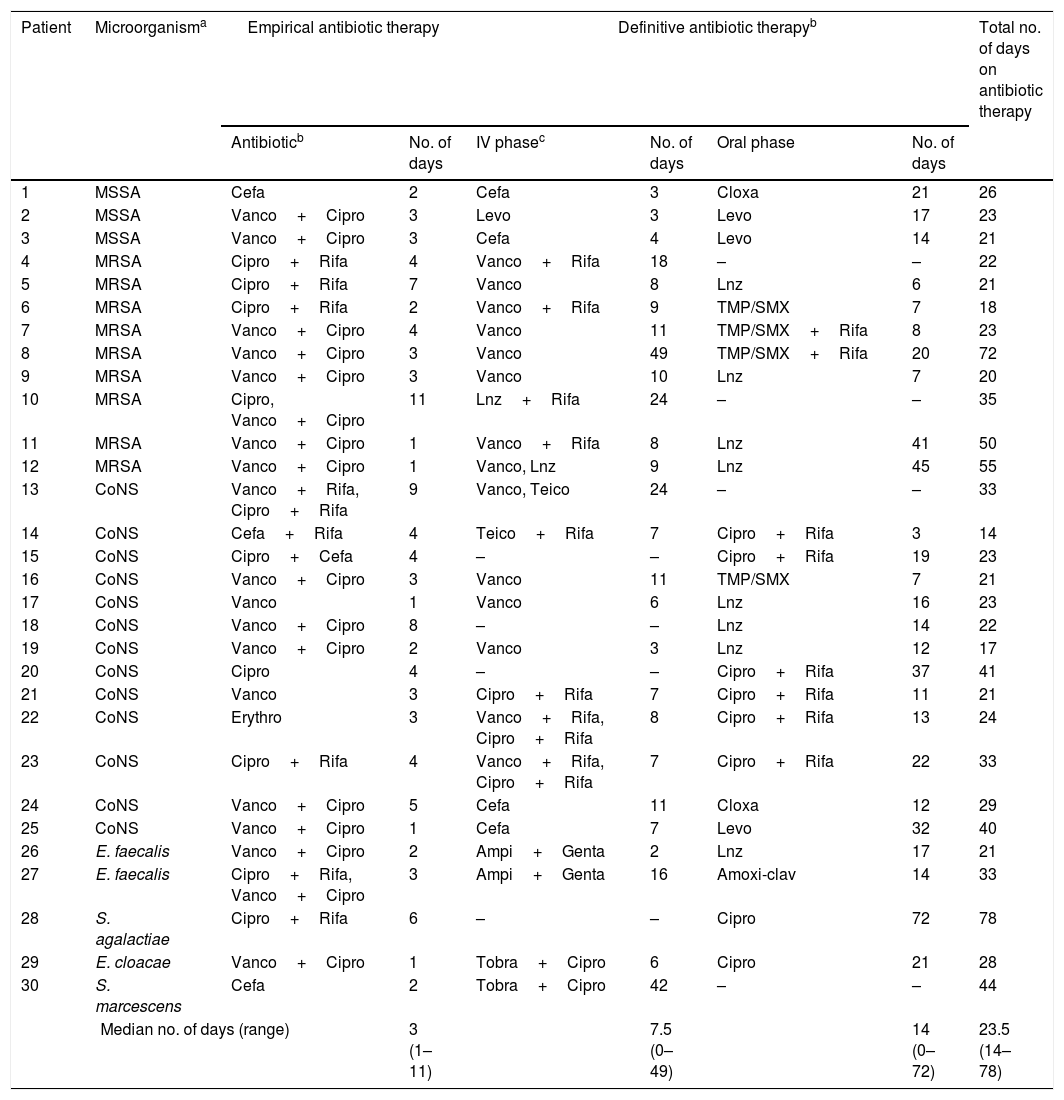
All patients received antibiotic treatment, as detailed in Table 2. Initially, intravenous empirical antibiotic therapy was used, which was subsequently adjusted to the susceptibility profile of the microorganism isolated in synovial fluid, and was changed to the oral route if the infection was caused by a microorganism susceptible to antibiotics with good bioavailability. Empirical antibiotic treatment included vancomycin in 19 patients (63%). Rifampicin was used at some point during treatment in 12 (48%) of the staphylococcal infections, including six (46%) of the 13 CoNS infections and six (50%) of the 12 S. aureus infections.
Antibiotic treatment.
| Patient | Microorganisma | Empirical antibiotic therapy | Definitive antibiotic therapyb | Total no. of days on antibiotic therapy | ||||
|---|---|---|---|---|---|---|---|---|
| Antibioticb | No. of days | IV phasec | No. of days | Oral phase | No. of days | |||
| 1 | MSSA | Cefa | 2 | Cefa | 3 | Cloxa | 21 | 26 |
| 2 | MSSA | Vanco+Cipro | 3 | Levo | 3 | Levo | 17 | 23 |
| 3 | MSSA | Vanco+Cipro | 3 | Cefa | 4 | Levo | 14 | 21 |
| 4 | MRSA | Cipro+Rifa | 4 | Vanco+Rifa | 18 | – | – | 22 |
| 5 | MRSA | Cipro+Rifa | 7 | Vanco | 8 | Lnz | 6 | 21 |
| 6 | MRSA | Cipro+Rifa | 2 | Vanco+Rifa | 9 | TMP/SMX | 7 | 18 |
| 7 | MRSA | Vanco+Cipro | 4 | Vanco | 11 | TMP/SMX+Rifa | 8 | 23 |
| 8 | MRSA | Vanco+Cipro | 3 | Vanco | 49 | TMP/SMX+Rifa | 20 | 72 |
| 9 | MRSA | Vanco+Cipro | 3 | Vanco | 10 | Lnz | 7 | 20 |
| 10 | MRSA | Cipro, Vanco+Cipro | 11 | Lnz+Rifa | 24 | – | – | 35 |
| 11 | MRSA | Vanco+Cipro | 1 | Vanco+Rifa | 8 | Lnz | 41 | 50 |
| 12 | MRSA | Vanco+Cipro | 1 | Vanco, Lnz | 9 | Lnz | 45 | 55 |
| 13 | CoNS | Vanco+Rifa, Cipro+Rifa | 9 | Vanco, Teico | 24 | – | – | 33 |
| 14 | CoNS | Cefa+Rifa | 4 | Teico+Rifa | 7 | Cipro+Rifa | 3 | 14 |
| 15 | CoNS | Cipro+Cefa | 4 | – | – | Cipro+Rifa | 19 | 23 |
| 16 | CoNS | Vanco+Cipro | 3 | Vanco | 11 | TMP/SMX | 7 | 21 |
| 17 | CoNS | Vanco | 1 | Vanco | 6 | Lnz | 16 | 23 |
| 18 | CoNS | Vanco+Cipro | 8 | – | – | Lnz | 14 | 22 |
| 19 | CoNS | Vanco+Cipro | 2 | Vanco | 3 | Lnz | 12 | 17 |
| 20 | CoNS | Cipro | 4 | – | – | Cipro+Rifa | 37 | 41 |
| 21 | CoNS | Vanco | 3 | Cipro+Rifa | 7 | Cipro+Rifa | 11 | 21 |
| 22 | CoNS | Erythro | 3 | Vanco+Rifa, Cipro+Rifa | 8 | Cipro+Rifa | 13 | 24 |
| 23 | CoNS | Cipro+Rifa | 4 | Vanco+Rifa, Cipro+Rifa | 7 | Cipro+Rifa | 22 | 33 |
| 24 | CoNS | Vanco+Cipro | 5 | Cefa | 11 | Cloxa | 12 | 29 |
| 25 | CoNS | Vanco+Cipro | 1 | Cefa | 7 | Levo | 32 | 40 |
| 26 | E. faecalis | Vanco+Cipro | 2 | Ampi+Genta | 2 | Lnz | 17 | 21 |
| 27 | E. faecalis | Cipro+Rifa, Vanco+Cipro | 3 | Ampi+Genta | 16 | Amoxi-clav | 14 | 33 |
| 28 | S. agalactiae | Cipro+Rifa | 6 | – | – | Cipro | 72 | 78 |
| 29 | E. cloacae | Vanco+Cipro | 1 | Tobra+Cipro | 6 | Cipro | 21 | 28 |
| 30 | S. marcescens | Cefa | 2 | Tobra+Cipro | 42 | – | – | 44 |
| Median no. of days (range) | 3 (1–11) | 7.5 (0–49) | 14 (0–72) | 23.5 (14–78) | ||||
E. faecalis: Enterococcus faecalis; S. agalactiae: Streptococcus agalactiae; MSSA: methicillin-susceptible Staphylococcus aureus; MRSA: methicillin-resistant Staphylococcus aureus; CoNS: coagulase-negative staphylococci; S. marcescens: Serratia marcescens.
Amoxicillin/clavulanic acid; Ampi: ampicillin; Cefa: cefazolin; Cipro: ciprofloxacin; Cloxa: cloxacillin; Erythro: erythromycin; Genta: gentamicin; Levo: levofloxacin; Lnz: linezolid; Rifa: rifampicin; TMP/SMX: trimethoprim-sulfamethoxazole; Tobra: tobramycin; Vanco: vancomycin. Rifampicin was always administered orally.
The median hospital stay was 14 days (range, 3–51 days). Two patients had complications: one of them (case 2, Table 2) had suffered from septic arthritis of sub-acute presentation caused by methicillin-susceptible S. aureus and suffered a relapse due to the same microorganism five days after having finished the antibiotic treatment. A new arthroscopic debridement was performed and antibiotic therapy was established with intravenous vancomycin followed by oral linezolid, with resolution of the infection after four weeks of treatment. The other patient (case 12, Table 2) had suffered from sub-acute arthritis caused by methicillin-resistant S. aureus and developed osteomyelitis of the tibia caused by the same microorganism, which was treated with linezolid for six weeks. Five weeks after having finished the treatment, he had reactivation of osteomyelitis, which was resolved after a new surgical debridement followed by combined antibiotic therapy with linezolid and rifampicin (28 days) and, subsequently, trimethoprim-sulfamethoxazole (46 days). This patient had experienced one of the highest synovial fluid cell counts of the entire series (101,840cells/mm3).
All infections were cured. After a median follow-up of 136 days (range, 29–539 days), 23 patients (77%) had returned to their normal work.
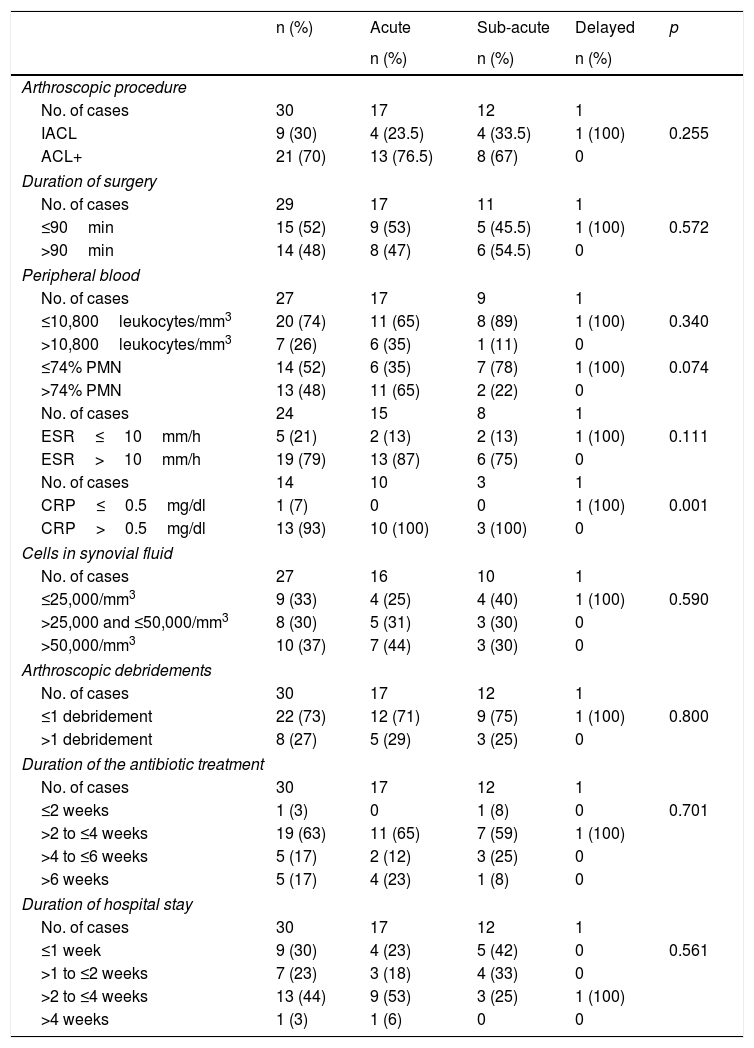
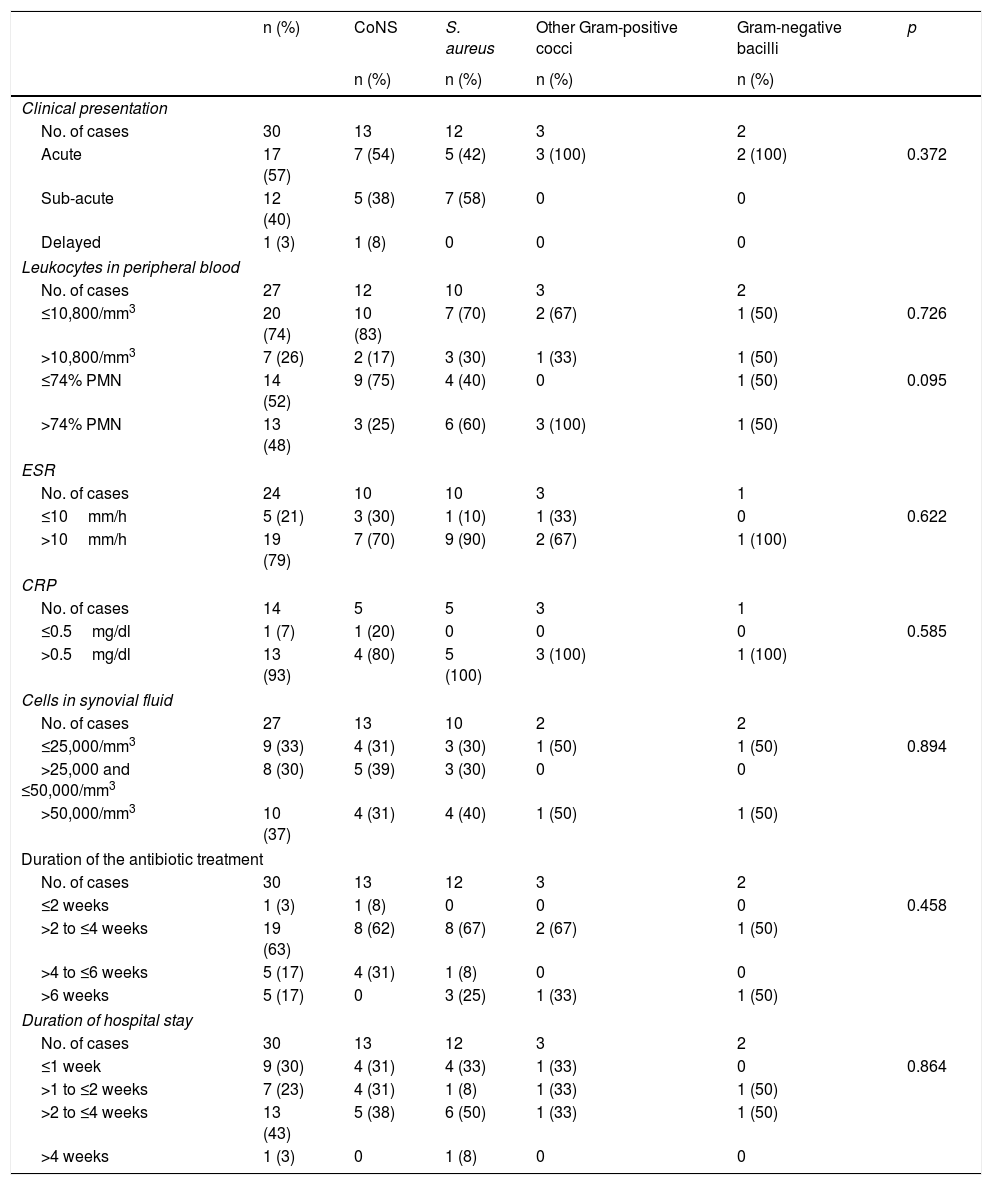
Comparative analysisThe analysis performed did not show any significant difference between the different types of infection, with the exception that acute arthritis tended to be associated with elevated CRP (Table 3). Similarly, no significant differences were revealed between infections according to the causative microorganism (Table 4). Finally, no statistically significant differences were observed in the median of treatment duration (in days) and in the hospital stay among treated patients (duration of treatment: median 25; P25-P75: 21–35; hospitalisation time: median 15; P25-P75: 9–20) and untreated patients (duration of treatment: median 22; P25-P75: 21–28; hospitalisation time: median 9; P25-P75: 7–16) with rifampicin (data not shown in the tables).
Characteristics of septic arthritis after anterior cruciate ligament reconstruction of the knee according to the type of infection.
| n (%) | Acute | Sub-acute | Delayed | p | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Arthroscopic procedure | |||||
| No. of cases | 30 | 17 | 12 | 1 | |
| IACL | 9 (30) | 4 (23.5) | 4 (33.5) | 1 (100) | 0.255 |
| ACL+ | 21 (70) | 13 (76.5) | 8 (67) | 0 | |
| Duration of surgery | |||||
| No. of cases | 29 | 17 | 11 | 1 | |
| ≤90min | 15 (52) | 9 (53) | 5 (45.5) | 1 (100) | 0.572 |
| >90min | 14 (48) | 8 (47) | 6 (54.5) | 0 | |
| Peripheral blood | |||||
| No. of cases | 27 | 17 | 9 | 1 | |
| ≤10,800leukocytes/mm3 | 20 (74) | 11 (65) | 8 (89) | 1 (100) | 0.340 |
| >10,800leukocytes/mm3 | 7 (26) | 6 (35) | 1 (11) | 0 | |
| ≤74% PMN | 14 (52) | 6 (35) | 7 (78) | 1 (100) | 0.074 |
| >74% PMN | 13 (48) | 11 (65) | 2 (22) | 0 | |
| No. of cases | 24 | 15 | 8 | 1 | |
| ESR≤10mm/h | 5 (21) | 2 (13) | 2 (13) | 1 (100) | 0.111 |
| ESR>10mm/h | 19 (79) | 13 (87) | 6 (75) | 0 | |
| No. of cases | 14 | 10 | 3 | 1 | |
| CRP≤0.5mg/dl | 1 (7) | 0 | 0 | 1 (100) | 0.001 |
| CRP>0.5mg/dl | 13 (93) | 10 (100) | 3 (100) | 0 | |
| Cells in synovial fluid | |||||
| No. of cases | 27 | 16 | 10 | 1 | |
| ≤25,000/mm3 | 9 (33) | 4 (25) | 4 (40) | 1 (100) | 0.590 |
| >25,000 and ≤50,000/mm3 | 8 (30) | 5 (31) | 3 (30) | 0 | |
| >50,000/mm3 | 10 (37) | 7 (44) | 3 (30) | 0 | |
| Arthroscopic debridements | |||||
| No. of cases | 30 | 17 | 12 | 1 | |
| ≤1 debridement | 22 (73) | 12 (71) | 9 (75) | 1 (100) | 0.800 |
| >1 debridement | 8 (27) | 5 (29) | 3 (25) | 0 | |
| Duration of the antibiotic treatment | |||||
| No. of cases | 30 | 17 | 12 | 1 | |
| ≤2 weeks | 1 (3) | 0 | 1 (8) | 0 | 0.701 |
| >2 to ≤4 weeks | 19 (63) | 11 (65) | 7 (59) | 1 (100) | |
| >4 to ≤6 weeks | 5 (17) | 2 (12) | 3 (25) | 0 | |
| >6 weeks | 5 (17) | 4 (23) | 1 (8) | 0 | |
| Duration of hospital stay | |||||
| No. of cases | 30 | 17 | 12 | 1 | |
| ≤1 week | 9 (30) | 4 (23) | 5 (42) | 0 | 0.561 |
| >1 to ≤2 weeks | 7 (23) | 3 (18) | 4 (33) | 0 | |
| >2 to ≤4 weeks | 13 (44) | 9 (53) | 3 (25) | 1 (100) | |
| >4 weeks | 1 (3) | 1 (6) | 0 | 0 | |
ACL+: anterior cruciate ligament reconstruction with additional procedures during the arthroscopic surgery; CRP: C-reactive protein; ESR: erythrocyte sedimentation rate; IACL: isolated anterior cruciate ligament reconstruction; PMN: polymorphonuclear leukocytes.
Characteristics of septic arthritis after anterior cruciate ligament reconstruction of the knee according to the microorganism causing the infection.
| n (%) | CoNS | S. aureus | Other Gram-positive cocci | Gram-negative bacilli | p | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||
| Clinical presentation | ||||||
| No. of cases | 30 | 13 | 12 | 3 | 2 | |
| Acute | 17 (57) | 7 (54) | 5 (42) | 3 (100) | 2 (100) | 0.372 |
| Sub-acute | 12 (40) | 5 (38) | 7 (58) | 0 | 0 | |
| Delayed | 1 (3) | 1 (8) | 0 | 0 | 0 | |
| Leukocytes in peripheral blood | ||||||
| No. of cases | 27 | 12 | 10 | 3 | 2 | |
| ≤10,800/mm3 | 20 (74) | 10 (83) | 7 (70) | 2 (67) | 1 (50) | 0.726 |
| >10,800/mm3 | 7 (26) | 2 (17) | 3 (30) | 1 (33) | 1 (50) | |
| ≤74% PMN | 14 (52) | 9 (75) | 4 (40) | 0 | 1 (50) | 0.095 |
| >74% PMN | 13 (48) | 3 (25) | 6 (60) | 3 (100) | 1 (50) | |
| ESR | ||||||
| No. of cases | 24 | 10 | 10 | 3 | 1 | |
| ≤10mm/h | 5 (21) | 3 (30) | 1 (10) | 1 (33) | 0 | 0.622 |
| >10mm/h | 19 (79) | 7 (70) | 9 (90) | 2 (67) | 1 (100) | |
| CRP | ||||||
| No. of cases | 14 | 5 | 5 | 3 | 1 | |
| ≤0.5mg/dl | 1 (7) | 1 (20) | 0 | 0 | 0 | 0.585 |
| >0.5mg/dl | 13 (93) | 4 (80) | 5 (100) | 3 (100) | 1 (100) | |
| Cells in synovial fluid | ||||||
| No. of cases | 27 | 13 | 10 | 2 | 2 | |
| ≤25,000/mm3 | 9 (33) | 4 (31) | 3 (30) | 1 (50) | 1 (50) | 0.894 |
| >25,000 and ≤50,000/mm3 | 8 (30) | 5 (39) | 3 (30) | 0 | 0 | |
| >50,000/mm3 | 10 (37) | 4 (31) | 4 (40) | 1 (50) | 1 (50) | |
| Duration of the antibiotic treatment | ||||||
| No. of cases | 30 | 13 | 12 | 3 | 2 | |
| ≤2 weeks | 1 (3) | 1 (8) | 0 | 0 | 0 | 0.458 |
| >2 to ≤4 weeks | 19 (63) | 8 (62) | 8 (67) | 2 (67) | 1 (50) | |
| >4 to ≤6 weeks | 5 (17) | 4 (31) | 1 (8) | 0 | 0 | |
| >6 weeks | 5 (17) | 0 | 3 (25) | 1 (33) | 1 (50) | |
| Duration of hospital stay | ||||||
| No. of cases | 30 | 13 | 12 | 3 | 2 | |
| ≤1 week | 9 (30) | 4 (31) | 4 (33) | 1 (33) | 0 | 0.864 |
| >1 to ≤2 weeks | 7 (23) | 4 (31) | 1 (8) | 1 (33) | 1 (50) | |
| >2 to ≤4 weeks | 13 (43) | 5 (38) | 6 (50) | 1 (33) | 1 (50) | |
| >4 weeks | 1 (3) | 0 | 1 (8) | 0 | 0 | |
CoNS: coagulase-negative staphylococci; CRP: C-reactive protein; ESR: erythrocyte sedimentation rate; PMN: polymorphonuclear leukocytes; S. aureus: Staphylococcus aureus.
Septic arthritis is a rare complication of anterior cruciate ligament reconstruction of the knee; the incidence in our series (0.9%) is similar to that in other studies.2–6 The risk factors for the development of this complication include those of the patient him/herself and surgery-dependent factors.5–8 Possible risk factors in our study included the fact that 27% of patients had undergone previous surgery in the same knee, and that in 70% of cases additional procedures were performed during the anterior cruciate ligament reconstruction.
Most patients in our series manifested symptoms/signs of arthritis within the four weeks following anterior cruciate ligament reconstruction. The most common were pain, joint effusion, local heat and febricula/fever. This clinical presentation is similar to that of other studies. Although pain and joint effusion are common after an uncomplicated anterior cruciate ligament reconstruction,4,8,9 their persistence for more than two days after surgery or their onset de novo should warn that there is a possibility of infection.2,4,8
If septic arthritis is suspected, a diagnostic arthrocentesis should be performed as soon as possible. In our series, the time elapsed from the onset of symptoms until the diagnostic arthrocentesis was performed was four days (range, 0–12 days). This delay reflects the difficulty in differentiating between a normal and abnormal clinical course following anterior cruciate ligament reconstruction and the resistance of the surgeon to perform a puncture in a knee which has recently been operated on.
Only 26% of patients had leukocytosis (>10,800cells/mm3), while the ESR and CRP were high in 79% and 93% of cases, respectively. After anterior cruciate ligament reconstruction of the knee, the ESR and CRP were raised until day 4–7 and, in the absence of complications, were normalised after four and two weeks, respectively.10–12 Therefore, if the CRP and ESR continue increasing or do not decrease to normal values within two weeks, the possibility of infection should be considered. The cell count in synovial fluid was similar to that described in other studies2,4; it is important to point out that the cell count was <25,000cells/mm3 in 33% of the cases and that 63% of patients had <50,000cells/mm3. Therefore, a normal cell count in synovial fluid in the appropriate clinical context does not rule out the diagnosis of septic arthritis.6,13 No differences were found between the lab test results of blood or synovial fluid and the form of presentation (acute, sub-acute and delayed) of septic arthritis.
Most infections in our series (83%) were caused by staphylococci, with the frequency of arthritis caused by S. aureus (40%) similar to that of arthritis caused by CoNS (43%). No differences were observed between the clinical presentation or the analytical data of arthritis caused by S. aureus or by CoNS. These results differ from those of other studies in which cases of arthritis caused by S. aureus are more common and present in a more acute form than those caused by CoNS.2,6 The frequency of infections caused by methicillin-resistant staphylococci in our series is striking. This means that this possibility should be taken into account when prescribing empirical antibiotic treatment for this complication.
In the event of septic arthritis, an arthroscopic debridement has to be performed as soon as possible in order to protect the graft and the joint cartilage.2,4–6 In more than half of the cases, arthroscopic debridement was performed the same day as the diagnostic arthrocentesis. Unlike in other studies, performing a single debridement was sufficient in most of our patients.4,9 In our series, the graft had a normal appearance in 64% of cases and it was not necessary to remove it in any patient.
There are no clearly established recommendations regarding the optimal antibiotic treatment of septic arthritis after anterior cruciate ligament reconstruction. The most common antibiotic regimen consists of intravenous treatment of various durations followed by oral antibiotic therapy for a total duration of six weeks.2–6 Although the antibiotic treatment of patients in our series was very heterogeneous, its duration was shorter than in other series and the infection was resolved in all cases.
No differences were observed between the clinical presentation of the infection (acute, sub-acute, delayed) or the responsible microorganism and the duration of the antibiotic therapy or hospitalisation. Nor were differences observed in the duration of treatment or hospitalisation between patients treated and patients not treated with rifampicin, although the very small number of patients treated with this antibiotic does not make it possible to draw any conclusions. Finally, we also failed to observe clinical or analytical differences in the patient with a relapse of arthritis or in the patient who developed osteomyelitis of the tibia, except for the high cell count in the synovial fluid in the latter.
Our study has significant limitations. As it is a retrospective series, the results should be interpreted with caution. As patients were selected based on positive cultures from synovial fluid, no possible cases of septic arthritis with negative cultures from synovial fluid were included. Therefore, the real incidence of this complication could be higher than that observed in this study. In this regard, it should be noted that the overall sensitivity of the synovial fluid cultures for the diagnosis of septic arthritis ranges between 76% and 95%,13 and that the frequency with which these are negative in septic arthritis after anterior cruciate ligament reconstruction of the knee has not been established. Lastly, another limitation of our series is the lack of functional assessment of the knee once the episode of septic arthritis is resolved. The series that include functional assessment studies describe similar or lower results than those obtained after uncomplicated anterior cruciate ligament reconstruction, with an incidence of arthrosis of up to 50% after 10–20 years.1,2,14,15
In conclusion, septic arthritis after anterior cruciate ligament reconstruction of the knee is a rare complication which generally manifests within four weeks following surgery. The most common symptoms/signs are pain, joint effusion, local heat and febricula/fever; it is not always accompanied by leukocytosis in the blood or in synovial fluid but the ESR and CRP are usually high. The most common causative microorganisms are CoNS and S. aureus, which may be resistant to methicillin. Treatment consists of early arthroscopic debridement (which may not be necessary to remove the graft) and antibiotic therapy, the optimal duration of which is not well established.
Conflict of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Erice A, Neira MI, Vargas-Prada S, Chiaraviglio A, Gutiérrez-Guisado J, Rodríguez de Oya R. Artritis séptica tras ligamentoplastia artroscópica de la rodilla: análisis retrospectivo de casos. Enferm Infecc Microbiol Clin. 2018;36:336–341.