Gastro-bronchial fistula is a rare complication in gastroesophageal surgical procedures. It is difficult to diagnose and its management is complex. Non-surgical alternatives have been developed to eliminate the mortality of small fistulas. Endoscopic treatment is an option for patients with small fistulas or in a serious condition.
Clinical caseA 38 year-old woman with evidence of a gastro-bronchial fistula after gastric sleeve surgery, which was diagnosed during the post-operative period due to presenting with a various clinical symptoms. It was initially managed as a respiratory infection. When the trajectory of the fistula was established, an attempt was made to close with endoclips. However, there was also a haemo-pneumothorax, which required inserting drainage tubes and a thoracotomy. Endoscopic management was chosen with polytetrafluoroethylene oesophageal prosthesis and fibrin as a last therapeutic option as the patient had systemic inflammatory response syndrome. The outcome was favourable.
DiscussionBariatric surgery has shown satisfactory results; however the complexity of the procedure can lead to severe complications, such as the present case. Gastro-bronchial fistulas represent a diagnostic and therapeutic challenge, requiring treatments from conservative management to endoscopic procedures, as in our patient.
ConclusionAlthough gastro-bronchial fistulas are a rare complication, the use of endoscopy in their resolution should be considered as the method of choice, as it offers a lower morbidity in the patient that usually presents a difficult to control respiratory problem, and with satisfactory results in the medium and long term.
La fístula gastrobronquial es una complicación infrecuente en procedimientos quirúrgicos gastroesofágicos. Resulta difícil su diagnóstico y complejo su manejo, por lo que se han desarrollado alternativas no quirúrgicas para obliterar las fístulas con la menor morbilidad y mortalidad. El tratamiento endoscópico es una opción para pacientes con fístulas pequeñas o en estado grave.
Caso clínicoMujer de 38 años de edad, con evidencia de fístula gastrobronquial postoperada de manga gástrica, diagnosticada durante el postoperatorio tardío debido a un cuadro clínico abigarrado, manejado inicialmente como cuadro respiratorio infeccioso; establecido el trayecto fistuloso se intentó cerrar el trayecto utilizando endoclips; sin embargo, se agrega hemoneumotórax, que ameritó colocación de sondas de drenaje y toracotomía, se optó por un manejo endoscópico con prótesis esofágica de politetrafluroetileno y fibrina como última alternativa terapéutica debido a que la paciente cursó con síndrome de respuesta inflamatoria sistémica, con respuesta favorable al manejo endoscópico.
DiscusiónLa cirugía bariátrica ha mostrado resultados satisfactorios; sin embargo, la complejidad del procedimiento favorece complicaciones graves, como en la del presente caso; las fístulas gastrobronquiales representan un reto diagnóstico y terapéutico, considerándose desde el manejo conservador hasta los procedimientos endoscópicos, como en nuestra paciente.
ConclusiónSi bien las fístulas gastrobronquiales son una complicación infrecuente, el uso de endoscopia en su resolución debe ser un arma de primer nivel en el manejo, ya que ofrece una morbilidad menor en un paciente que habitualmente cursa con un cuadro respiratorio de difícil control, con resultados satisfactorios a mediano y largo plazo.
Of all the gastric fistulas described in the medical literature, those that communicate to the bronchi appear to be one of the rarest. It occurs most frequently as a complication of a subphrenic or perigastric abscess that extends through the diaphragm to form an empyema, or a lung abscess, which in turn arrives at the bronchial tree. The formation of a bronchial fistula results from a perforation of the stomach, or when there is necrosis of a portion of the stomach wall. Other causes include trauma originating as a result of a ruptured diaphragm associated with lung and stomach injury, and necrosis in infiltrating neoplasia, which could either be a primary tumor of the stomach or a tumour originating in a nearby area1.
In most cases, antibiotic treatment is usually sufficient, so long as the clinical conditions of the patient allow it. A treatment alternative for gastro-bronchial fistula, when conservative treatment fails, may be the percutaneous drainage of collections. For this reason, non-surgical alternatives have been developed to close bronchial fistulas with the lowest possible number of complications. Some of the endoscopic techniques described feature the application of sealing substances, the introduction of catheters or vascular spirals for the occlusion of the fistula, silicone or metal prosthetics, and submucosal injection of substances to bring the edges of the fistula closer2–5.
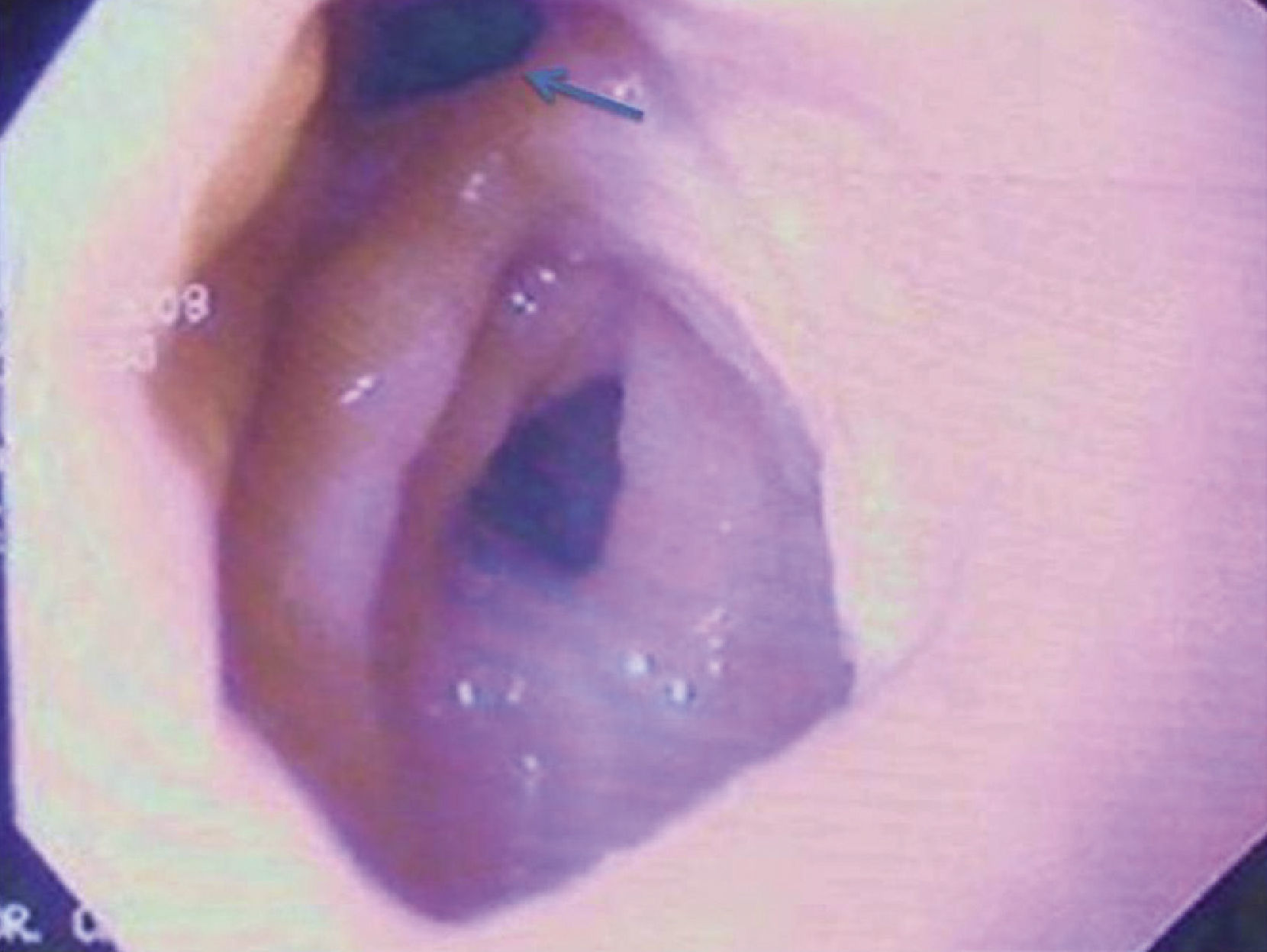
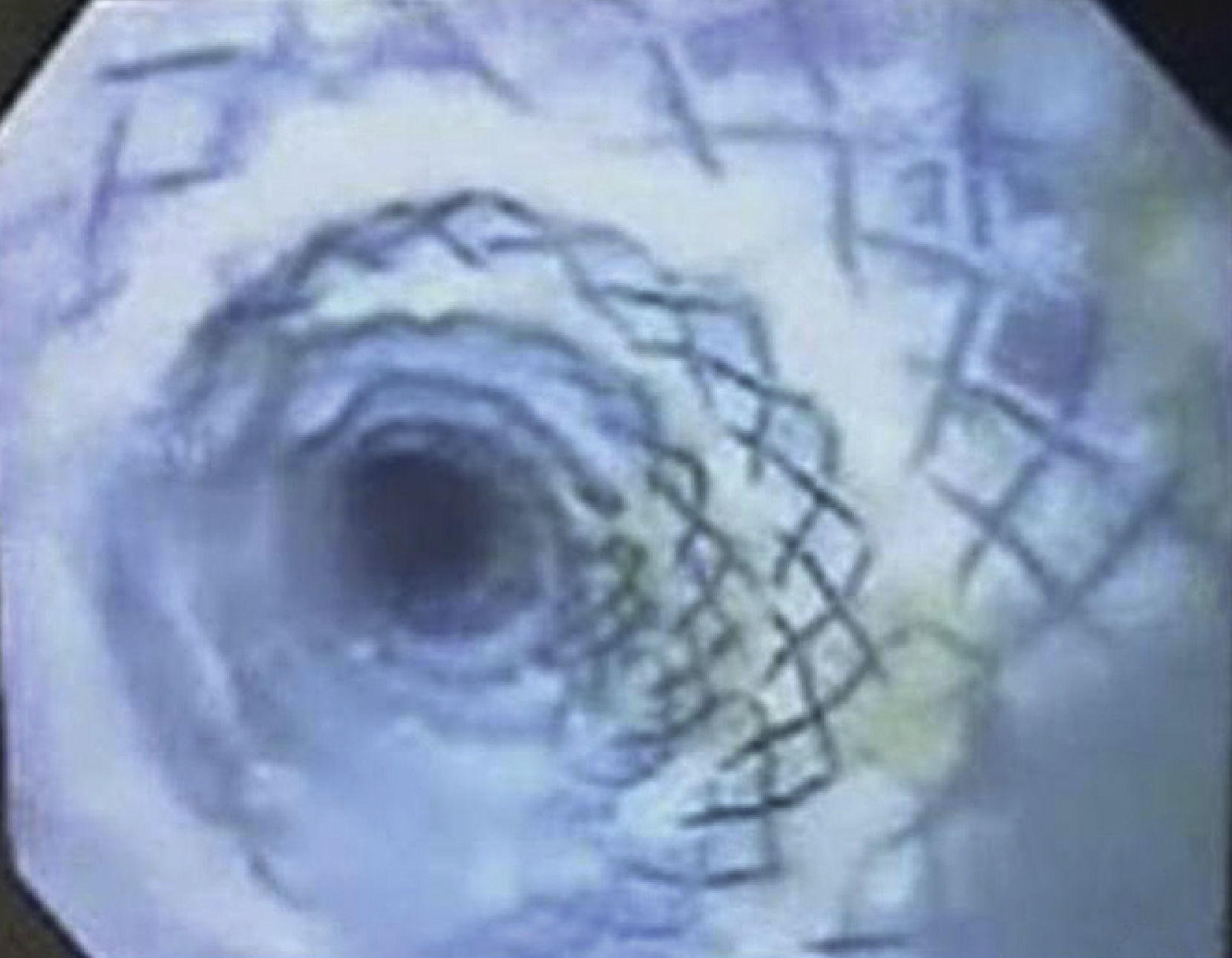
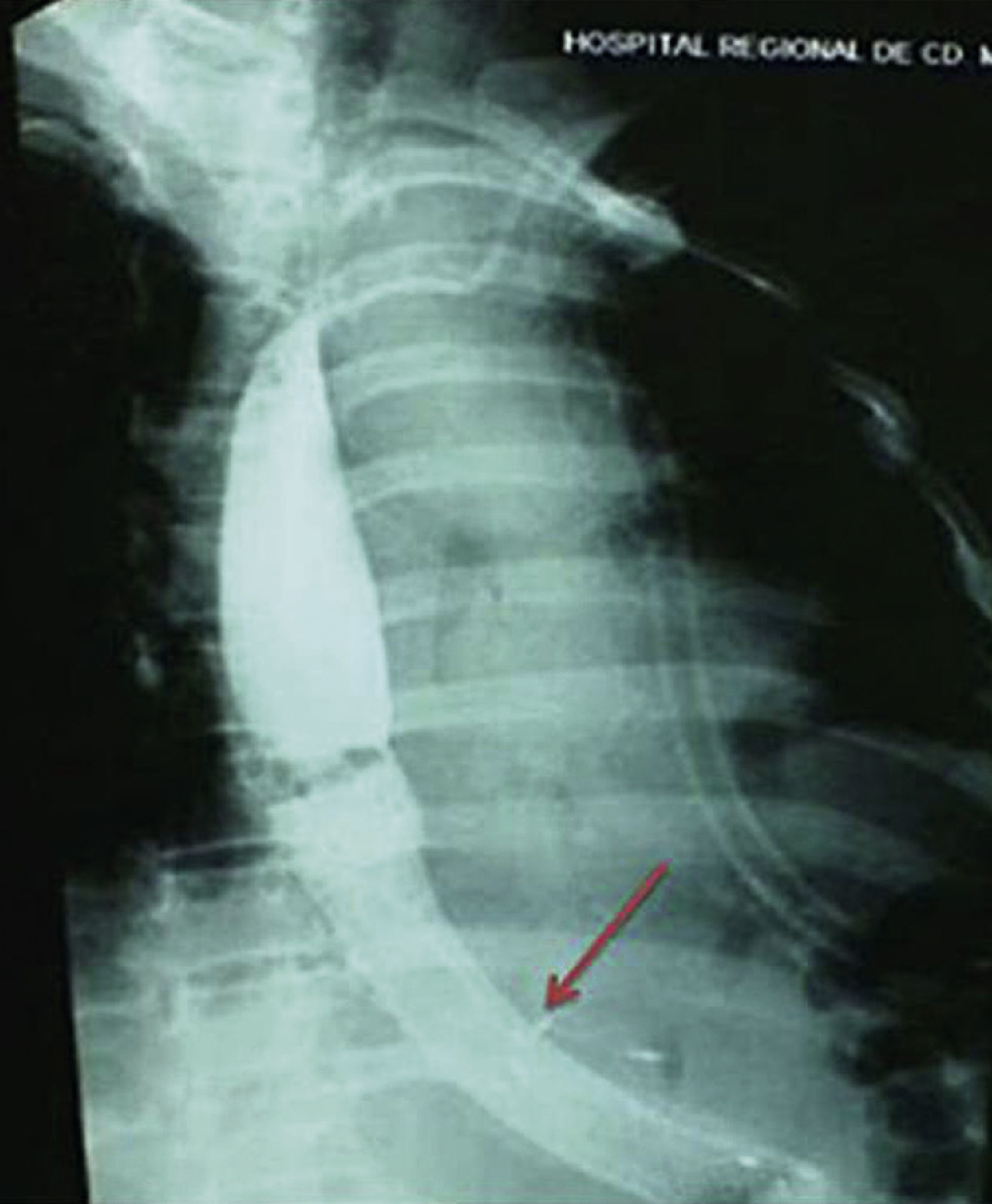
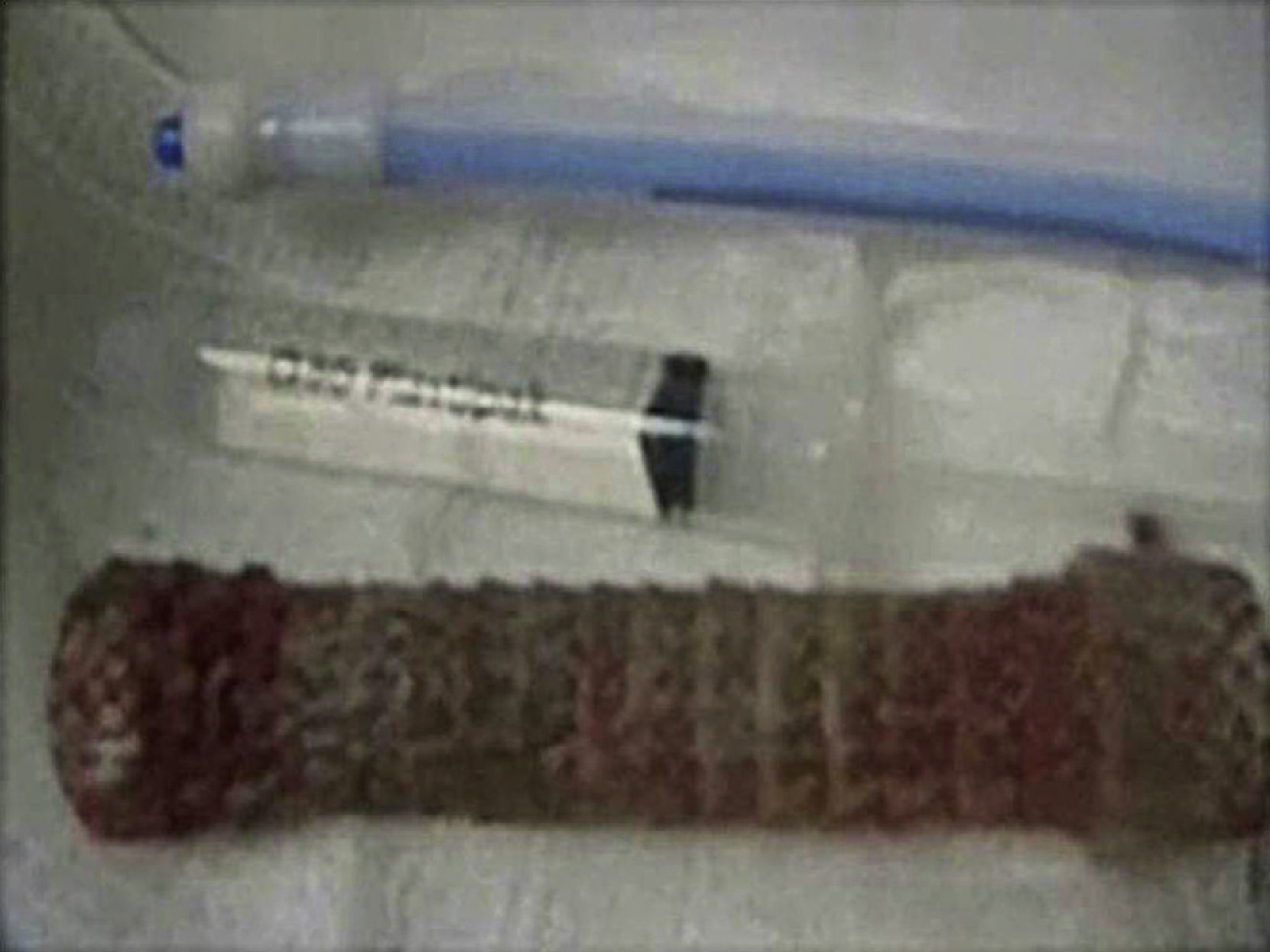
Clinical caseWoman, 38 years, with morbid obesity, with a body mass index of 45, with no response to medical treatment, complete preoperative assessment pursuant to the hospital protocol. The sleeve gastrectomy was carried out laparoscopically, with peritonization of the staple line with vicryl 2-0, without complications, pneumatic leak test showed negative; a soft suction drainage was left, without evidence of leakage during surgery and the immediate postoperative period (Fig. 1). She was readmitted on the eighth postoperative day with fever, tachycardia, pain on the left side, leukocytosis 20,000 cells/mm3, at the expense of neutrophils 85.2%, haemoglobin 12 g/dl, platelets 283,000 cells/mm3, glucose 105 mg/dl, urea 21.4 mg/dl, creatinine 0.64 mg/dl, glutamic-oxaloacetic transaminase 20 UI/l, glutamate pyruvate transaminase 23 IU/l, lactic dehydrogenase 408 IU/l, alkaline phosphatase 189 IU/l, amylase 31 IU/l, total bilirubin 2 IU/l, total protein 7.1, albumin 3.8, sodium 135 mEq/l, potassium 3.2 mEq/l and chloride 96 mEq/l, with turbid drain in the suction drainage area and more than 1,000 IU/l of amylase on said account. A pancreatic fistula was suspected and it was treated as such. She was discharged the following week, practically asymptomatic. On the fourteenth day, she presented left basal pneumonia symptoms, without abdominal clinical manifestations, with ultrasound and CT scan results negative for abdominal collection. A fistula orifice was found below the cardio-oesophageal junction at the level of the sleeve gastrectomy during a control endoscopy (Figs. 2 and 3). Endoclips, fasting and parenteral nutrition were prescribed; she presented haemopneumothorax, which required the placement of a double chest drainage tube, documenting a gastro-bronchial fistula with contrast radiological studies, deciding to place an oesophageal prosthetic of polytetrafluorethylene and fibrin in the fistulous tract (Figs. 4 and 5). She was treated in the Intensive Care Unit with ventilation support due to persistent haemothorax which required left thoracotomy with suture of bronchopleural fistulas. The oesophageal prosthetic was removed, showing a closure of the fistulous tract and ulcerations secondary to the use of said prosthetic, with good response to medical treatment (Fig. 6). Currently, she is controlled as an outpatient, having resolved this severe complication.
DiscussionIn the long term, bariatric surgery has shown the best results for morbid obesity, in patients with obesity refractory to medical treatment. Traditionally, the primary mechanisms through which bariatric surgery achieves its objectives are related to the following: restriction of food ingestion and reduction of absorption, and a combination of both. However, these surgical techniques increase the risk of causing proteo-energetic malnutrition or selective deficit of some micronutrients, and fistulas in the gastro-oesophageal junction. One of the most severe complications is leaks in the staple line or anastomosis (the early resolution of which is complex); in late presentations, the main symptoms that may be mentioned are occlusion, internal hernias, eventrations, cholelithiasis and gastro-bronchial/gastro-pulmonary fistulas; the latter poses difficult diagnosis6.
In recent years, the number of surgical interventions for the treatment of obesity has increased exponentially, and, in accordance, so has the number of complications, which is currently between 4 and 22%, depending on the technique of choice. The rate of gastric fistulas is around 8.3%; it is a severe complication that frequently causes abdominal sepsis and respiratory pathologies, particularly in the left lung, secondary to a subphrenic abscess7–9.
In the medical literature we find different articles making reference to gastro-bronchial fistulas after obesity surgery. Gastro-bronchial fistulas are a severe complication that may compromise the life of the patient and, therefore, require early diagnosis and treatment. Some of the surgical risk factors are the following: postpneumonectomy empyema, prolonged mechanical ventilation, excessive intravenous fluids during postsurgical period (first 12 hours) and haemotransfusions. The reported clinical risk factors are the following: resection due to swelling or infection, tuberculosis, empyema, culture (+), use of steroids, diabetes, immunosuppression, malnutrition and resection following radiation10–13.
For many years, surgical reintervention was considered the only way to resolve this complication, despite the high rate of morbidity and mortality (79%). Mortality ranges between 20 and 70% depending on the series, and it is mostly due to aspiration pneumonia, acute respiratory difficulty syndrome and sepsis14–16.
This case required comprehensive treatment due to the extreme severity of the clinical conditions that were present at the time of admission in the Intensive Care Unit. By means of endoscopy, it was decided to place an oesophageal prosthetic of polytetrafluorethylene and fibrin in the fistulous tract, and, thanks to the thoracotomy, the fistula was sutured at the bronchopleural level, without the need to modify the bariatric technique. Being an infrequent complication, there are no well-established diagnostic and treatment algorithms, and, in our case, the result of the strategy of choice was satisfactory.
ConclusionBariatric surgery has shown results in morbid obesity; however, the complexity of the procedure favours severe complications such as in this case. The presence of gastro-bronchial/gastro-pulmonary fistulas poses a difficult diagnosis due to the degree of variability in presentation, since resolution represents a true therapeutic challenge.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Guerrero-Silva L. A. et al. Fístula gastrobronquial: complicación mayor de manga gástrica. Cirugía y Cirujanos. 2015; 83: 46-50.