Serial lengthening with growing rods is recommended every six months for the treatment of early onset scoliosis. The objective of this study was to evaluate the longitudinal growth of the thorax and control of the deformity in a series of patients with juvenile scoliosis when time intervals were increased between lengthenings.
Material and methodsRetrospective study of eight patients. The following variables were measured: the Cobb angle, the apical vertebral translation, the coronal balance, thoracic T1–L1 length, thoracic T5–T12 kyphosis, the proximal junctional kyphosis (PJK) angle, and the lumbar lordosis. Complications were recorded.
ResultsFive idiopathic and three syndromic scoliosis cases (mean age 9.4±1.5 years) were evaluated. The initial surgery was followed by with an average of two distractions per patient. The mean time between distractions was 15.7 months. The final coronal main curve correction was 58%. Apical translation and coronal balance were improved and maintained after the surgeries. The thoracic (T1–L1) preoperative length was 20.8cm, the postoperative length was 24.4cm, and the final length was 26cm. At the end of follow-up, the average growth of the thorax was 5.2cm. The preoperative (T5–T12) kyphosis was 33.5°, and final 32.1°. The change in the PJK angle was 2.5° at the end of follow-up. Most complications were related to instrumentation. Two superficial wound infections were encountered.
ConclusionFor less severe juvenile scoliosis patients treated with growing rods, spacing out lengthenings over more than a year can decrease the number of surgeries, while still controlling the deformity and allowing longitudinal thoracic growth.
Evaluar el crecimiento longitudinal del tórax y el control de la deformidad en una serie de pacientes con escoliosis juvenil tratados con barras de crecimiento aumentando los intervalos de tiempo entre alargamientos más de seis meses.
Material y métodosEstudio retrospectivo de ocho pacientes midiendo las siguientes variables: el ángulo de Cobb, la traslación vertebral apical, el balance coronal, la longitud torácica T1-L1, la cifosis torácica T5-T12, el ángulo de cifosis de unión proximal (CUP) y la lordosis lumbar. Se registraron las complicaciones.
ResultadosSe evaluaron cinco escoliosis idiopáticas y tres casos de sindrómica (media de edad 9,4±1,5 años). Se realizó una cirugía inicial y un promedio de dos retensados por paciente. El tiempo medio entre retensados fue de 15,7 meses. La corrección coronal final de la curva principal fue del 58%. La longitud torácica (T1-L1) preoperatoria fue de 20,8cm, postoperatoria de 24,4cm, y final de 26cm. Al final del seguimiento el crecimiento medio del tórax fue de 5,2cm. La cifosis preoperatoria (T5-T12) fue 33,5°, y final 32,1°. El cambio en el ángulo CUP fue de 2,5° en el seguimiento final. La mayoría de las complicaciones estuvieron relacionadas con la instrumentación. Se encontraron dos infecciones superficiales de la herida.
ConclusiónEn pacientes con escoliosis juvenil en formas «menos graves» tratados mediante barras de crecimiento, es posible espaciar los alargamientos más de un año y con ello disminuir el número de cirugías y al mismo tiempo controlar la deformidad y permitir el crecimiento longitudinal torácico.
The main objective in the management of spinal deformity in immature patients is to delay fusion for as long as possible.1 Several growth-preserving techniques have been proposed in order to control early onset scoliosis in these patients.2 These methods range from casts and braces to surgical techniques without fusion, which enable correction of the deformity, preserving the growth of the spine and rib cage, as well as lung maturation, which mainly occur during the first 8 years of life.3
Growing rods are another treatment option.4 Through solid proximal and distal anchors, they allow elongation by consecutive surgeries to apply distraction through connectors joining the rods. Frequent elongations are required in order to prevent joint fusion secondary to immobilization caused by the instrumentation and to allow the growth of the spine.5 The most commonly recommended interval between distractions is 6 months.6–8 However, this technique requires patients to undergo repeated interventions, which may lead to potential complications such as recurrent infections, wound dehiscence, unacceptable scarring and negative psychological consequences.9,10
This method is currently being applied in the treatment of early onset scoliosis, and its results among patients aged between 4 and 6 years have been published.4,8,11,12 Growth at this age takes place at an accelerated rate.3 However, there is scarce literature on “older” immature patients, that is, those aged between 5 and 10 years; a period considered as juvenile scoliosis. Although thoracic growth slows down at this stage,3 patients with significant spinal curvature can still benefit from non-fusion techniques to help in the final stages of thoracic growth and lung development.
In the present study we examined the use of growing rods among patients with juvenile scoliosis to control the deformity whilst preserving spinal growth. The working hypothesis was based on the fact that, due to a slower rate of growth of the spine and rib cage, as well as lung development taking place at this stage, these patients could benefit from decreasing the frequency of distractions. This change could reduce the rate of potential complications published without impacting thoracic growth significantly. The objective of this study was to evaluate the longitudinal growth of the thorax and control of the deformity among a series of patients with juvenile scoliosis treated by growing rods when the time intervals between elongations were increased.
Materials and methodsWe retrospectively reviewed the medical records of children with juvenile scoliosis treated consecutively with growing rods by the same surgeon at a single hospital. Patients included in the study were those with scoliosis in juvenile age (“older” immature patients, aged between 5 and 10 years, but still with Risser sign 0 and open triradiate cartilage), who were treated with growing rods by serial elongations spaced over 6 months and a follow-up period of at least 2 years. We excluded patients who underwent other non-fusion techniques, those treated with growing rods with less than 2 elongations or with elongations spaced less than 6 months apart, and those undergoing surgical revisions (non-primary surgery). All parents signed informed consent forms and were aware of the clinical study, which followed the principles of the Helsinki declaration.
All patients were treated through a single posterior approach and the technique of growing rods described by Akbarnia et al.4 Lengthening of the instrumentation was not performed every 6 months as recommended, in an attempt to avoid the complications derived from repeated surgeries. The decision of when to distract the instrumentation was adopted based exclusively on curve progression, coronal or sagittal decompensation, and clinical evidence of worsening of the deformity during the follow-up period.
Frontal and sagittal radiographs were analyzed before the initial surgery, before and after each elongation, and at the end of the follow-up period. The following variables were measured: coronal Cobb angle of the primary curve, apical vertebral translation (as the distance in centimeters from the central sacral vertical line to the apex of the primary curve), coronal balance, T1–T12 thoracic length (used to calculate the growth of the thoracic spine over the course of the treatment), thoracic T5–T12 kyphosis, angle of proximal junctional kyphosis (PJK) and lumbar lordosis. All complications were recorded.
Descriptive statistics were carried out using the software package SPSS (version 11.5, SAS Institute Inc., Cary, NC, USA). Mean values were presented along with standard deviations or ranges.
ResultsA total of 8 patients met the inclusion criteria. The mean age at the time of the first intervention was 9.4±1.5 years (range: 6.5–11 years). All patients presented Risser 0 and an open triradiate cartilage before the initial surgery. Of these, 4 were males and 4 were females. A total of 5 patients suffered idiopathic scoliosis (62.5%), whilst 3 had syndromic scoliosis (37.5%): 1 Klippel–Trenaunay syndrome, 1 Sotos syndrome, and 1 nemaline myopathy. In total, 5 patients had a single thoracic curve, whilst 3 had double primary curves. Six patients had right thoracic curves, and 2 patients had left primary thoracic curves.
All patients were treated by a single posterior approach and the technique of growing rods described by Akbarnia et al.4 Two patients were treated with unilateral rods and the rest with bilateral growing rods. The mean number of instrumented levels was 12.4±3.1. The mean period between distractions was 15.7 months (range: 7–36 months), with a mean number of 2 distractions per patient. The mean period elapsed between the initial surgery and the first elongation was 17.4±10.1 months and the mean time from the first to the second elongation was 14±4.6 months. A total of 4 definitive fusions were performed. The mean follow-up period was 78 months (range: 30–180 months).
The mean values of the coronal Cobb angle of the primary curve in the preoperative and postoperative periods and at the end of follow-up were 56.5°±8.1°, 24.7°±12.7° and 23.7°±12.8°, respectively. The mean final correction was 58%. On average, 16.8° were lost before the first elongation and 11.5° before the second elongation. The mean value of preoperative apical translation was 4.8±2.8cm and the final was 1.9±0.5cm. The mean value of preoperative coronal balance was 1.8±2.2cm and the final was 1±1.2cm.
Mean thoracic length (T1–T12) values in the preoperative and postoperative periods and at the end of follow-up were 20.8±4.6cm, 24.4±4.0cm and 26±4cm, respectively. The initial surgery increased thoracic length by 3.5±1.6cm, the first elongation by 3±2.1cm and the second elongation by 2.6±1.1cm, with a mean 1.5cm being lost between elongations. At the end of the follow-up period, the mean thoracic growth was 5.2cm.
The mean values of kyphosis (T5–T12) in the preoperative and postoperative periods and at the end of follow-up were 33.5°±15°, 23.4°±11.8° and 32.1°±14.6°, respectively. The first surgical procedure achieved a mean correction of 10°, the second of 5.3° and the third of 4°. A mean 6.4° were corrected by each elongation, with a mean 5° being lost between elongations.
Mean initial PJK was 7.7°±8.8°, and the final mean value was 10.1°±7.9°. The change in the PJK angle at the end of the follow-up period was 2.5°.
Preoperative lumbar lordosis was of 47.5°±7.4°, with a final value of 44.7°±10.3°.
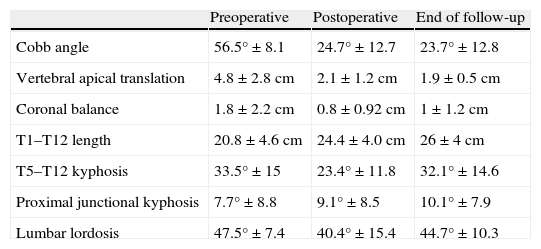
The results are shown in Table 1.
Surgical results.
| Preoperative | Postoperative | End of follow-up | |
| Cobb angle | 56.5°±8.1 | 24.7°±12.7 | 23.7°±12.8 |
| Vertebral apical translation | 4.8±2.8cm | 2.1±1.2cm | 1.9±0.5cm |
| Coronal balance | 1.8±2.2cm | 0.8±0.92cm | 1±1.2cm |
| T1–T12 length | 20.8±4.6cm | 24.4±4.0cm | 26±4cm |
| T5–T12 kyphosis | 33.5°±15 | 23.4°±11.8 | 32.1°±14.6 |
| Proximal junctional kyphosis | 7.7°±8.8 | 9.1°±8.5 | 10.1°±7.9 |
| Lumbar lordosis | 47.5°±7.4 | 40.4°±15.4 | 44.7°±10.3 |
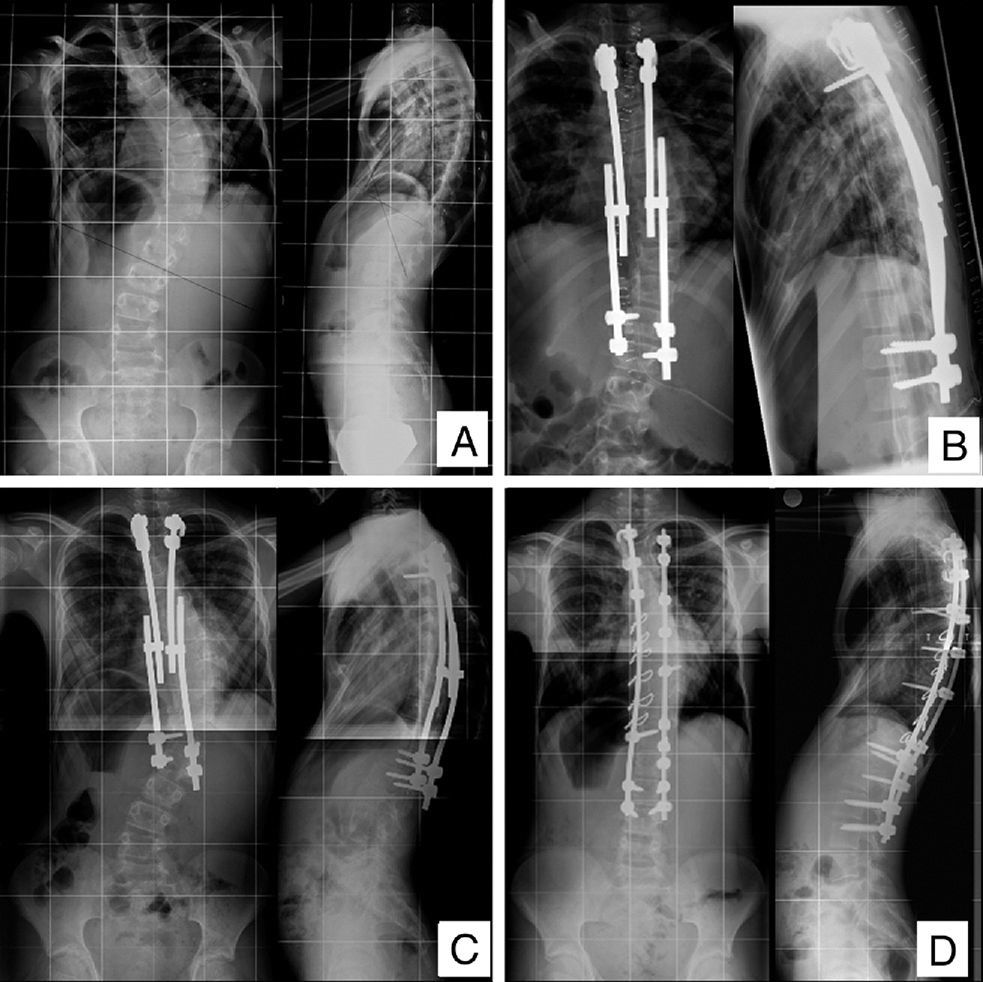
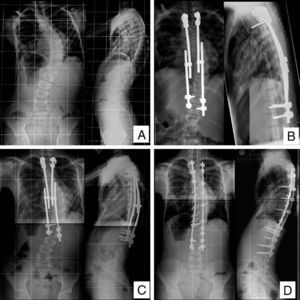
We recorded several complications associated with the instrumentation. In the 2 patients treated with unilateral rods, the rods broke and were replaced by bilateral rods. One patient suffered loosening of the proximal hooks and required extension to a proximal level. One patient presented distal adding-on (Fig. 1), which required descent to a distal level neutral to the final fusion. Only 2 patients suffered a superficial wound infection and both were successfully treated with antibiotics and conservative treatment. There were no deep wound infections or dehiscence, or any cases of unacceptable scarring.
(A) Child aged 9.8 years with idiopathic scoliosis and pectus excavatum, with severe pulmonary restriction. He presented progressive right thoracic scoliosis of 64°, a T1–L1 length of 19cm and skeletal immaturity. (B) The patient was treated with bilateral growing rods with an initial coronal correction of 53%. The first elongation took place after 14 months and the second elongation after a further 8 months. (C) The control radiograph before the definitive fusion shows the progression of the curve and a distal adding-on phenomenon. (D) Two years after the definitive posterior fusion, with a final coronal correction of 75%, a final T1–L1 length of 25cm and resolved adding-on.
Lung development and growth of the spine and the thorax mainly take place in the first 8 years of life. Thus thoracic deformity may affect lung maturation and the formation of the rib cage.3,13 Early onset scoliosis has been shown to inhibit the development of lung and alveolar tissue, which can lead to chest insufficiency syndrome.14 Early spinal fusion in these patients decreases the height of the thoracic spine, which correlates with a decrease in forced vital capacity.1
Growth takes place over successive acceleration and deceleration phases comprising 3 periods. In a healthy child, growth of the longitudinal spine takes place at a high rate for the first 5 years, with the T1–S1 distance increasing by 2cm/year on average. A resting phase takes place between the ages of 5 and 10 years, followed by a slow progression in longitudinal growth, estimated at 1cm/year, which then increases to 1.8cm/year during adolescence.3 A T1–T12 distance less than 18cm at maturity is associated with decreased lung function (less than 45% prediction value).1,10 Therefore, the objective of treating early onset scoliosis is to control the deformity of the spine while allowing the thorax to grow, thus improving the volume of the rib cage and the lung, at least until lung maturity is reached.
One way of stabilizing and controlling these deformities is through the growing rods technique.4 After a firm proximal and distal anchoring, longitudinal growth is allowed by serial elongations when the rods are distracted through tandem connectors. With this non-fusion technique, consecutive elongations allow vertebral growth until skeletal maturity is reached and final fusion can be performed. So far, good results have been reported with this technique in very immature patients with early onset scoliosis, and ages between 4 and 6 years,4,8,11,12 when growth was in the acceleration phase. At this age, the T1–T12 segment normally grows by 1.3cm/year.3 However, this procedure forces patients to undergo repeated interventions, which may lead to potential and frequent complications, such as wound infections and dehiscence, unacceptable scarring and negative psychological consequences.9,10 The goal of the surgeon is to achieve a balance between spinal fusion induced by immobilization secondary to instrumentation and the possible complications which may be caused by repeated interventions. The risk of complications associated to growing rods increases by 24% for each additional surgical procedure performed on these patients.15
An annual growth of about 1.0–1.7cm has been reported in patients with early-onset scoliosis treated with growing rods. The initial surgery reaches the greatest distraction of 5cm on average for T1–S1 or 2.5cm for T1–T12, as well as the greatest coronal correction (51–58%).4,5,8,11,12 To achieve this, frequent elongations are recommended,5 with a 6 month period between elongations being the most commonly recommended.6,8 However, it seems that the effectiveness of repeated elongations decreases over time due to a process of rigidity or “autofusion” of the spine caused by prolonged immobilization generated by the implanted device.8 This explains why some authors recommend delaying the initial surgery if the deformity and conservative treatment allow it, and reducing the number of elongations once the improvements begin to diminish.12,15
In patients with juvenile scoliosis (5–10 years old), there is a slowdown of 0.7cm/year in T1–T12 thoracic growth.3 At 5 years, chest volume is only 30% of its final size and the trunk is only 66% of its final height.3 It has been reported that a thoracic spine height of 18–22cm or more is required to prevent severe respiratory failure.1 Therefore, patients with a significant curve in this quiescent juvenile phase still need to be treated, and could also benefit from non-fusion techniques which help in the final stages of lung and chest growth and development, before the final growth spurt of adolescence takes place. These “older” immature patients are difficult to treat with casts, and the final fusion may result in a short trunk, a certain degree of breathing failure1 or crankshaft phenomenon.16 There is very scarce literature on the management of juvenile scoliosis in immature patients.17
This study analyzes the technique of growing rods in patients with juvenile scoliosis. Logically, the initial surgery was delayed compared to publications about early onset scoliosis (with a mean age of 5 years4,8,11,12). The mean age of our patients was 9.4 years (range: 6.5–11 years), but they were still skeletally immature (Risser 0 and open triradiate cartilage). The initial correction was of 57% and this was maintained but did not improve with additional elongations. This fact has also been described in younger patients.4,8,11,12 The mean preoperative T1–T12 length was 20cm, a “dangerous” thoracic length range according to Karol,1 and the initial intervention obtained a mean increase of 3.5cm. Elongations were also necessary in our “older” patients, as all the parameters worsened progressively during follow-up and required restoration through additional surgical procedures. However, in order to avoid possible complications, we did not adhere to the “6-month rule” between elongations strictly. The frequency of elongations depended exclusively on the following clinical criteria: progression of the curve, coronal or sagittal decompensation, or deformity with clinically evident deterioration detected during each clinical review conducted every 6 months. The mean period between distractions was finally 15.7 months (range: 7–36 months). The mean period until the first distraction was 17.4 months and the mean period until the second distraction was 14 months. A mean total of 2 distractions were required per patient, probably because these patients were at the quiescent stage of growth. Even with this low rate of elongation, we still managed to extend the thorax by a mean 5.2cm (approximately 1.07cm/year, a similar growth rate to that of healthy children), reaching a final length of 26cm (far exceeding the “dangerous” limit proposed by Karol1). A risk of proximal junctional kyphosis and progressive kyphosis with additional distractions has been reported with different non-fusion techniques among patients with early onset scoliosis.10,12,15 Our study showed a sustained preoperative kyphosis at the end of the follow-up period and a discreet change in the PJK angle of 2.5°. It is possible that this outcome was favored by the low rate of elongations. Complications due to the instrumentation were similar to those reported in the treatment of early onset scoliosis,9,15 but only 2 superficial wound infections were identified and successfully treated with conservative measures. No cases of deep wound infections, wound dehiscence and unacceptable scarring were found.
This study has several limitations. Firstly, we only examined 8 cases and they had different diagnoses, thus making it impossible to generalize the results. However, due to the low incidence of juvenile scoliosis, the literature does not contain long series of homogeneous patients. Secondly, the retrospective nature of this study lacks a prospective random assignment of subjects and does not allow comparison of the clinical outcomes of patients undergoing other treatments. There are obvious difficulties in gathering prospective data from patients whose treatment and follow-up require such a long period of time. Thirdly, we did not have a comparative monitoring cohort undergoing regular elongations every 6 months. Nevertheless, we have attempted to compare our results with reports from series of early onset scoliosis, as there are no reports on series of juvenile scoliosis. Lastly, we have worked with patients suffering “less severe” juvenile scoliosis, with mean Cobb magnitudes of 56.5°±8.1°. Considering these limitations, our results should be rigorously evaluated in a large population sample including controlled prospective comparison groups.
ConclusionIn patients with “less severe” forms of juvenile scoliosis treated with growing rods, it is possible that spacing elongations over 1 year could reduce the number of interventions, whilst at the same time controlling the deformity and allowing longitudinal thoracic growth.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Pizones J, Rodríguez-López T, Zúñiga L, Sánchez-Mariscal F, Álvarez-González P, Izquierdo E. Tratamiento de la escoliosis juvenil: aumentar el tiempo entre alargamientos con la técnica de barras de crecimiento no debe comprometer necesariamente el crecimiento torácico. Rev Esp Cir Ortop Traumatol. 2014;58:297–302.