To evaluate the accuracy of ultrasonography for the diagnosis of acute appendicitis in adults, to calculate the negative appendicectomy rate in operated patients and the accuracy of pre-defined diagnostic categories and to identify statistically significant signs and symptoms of acute appendicitis in ultrasonography.
Material and methodsDescriptive prospective study in which we collected the findings of the urgent ultrasonographies ordered in a one-year period for adult patients with pain in the right iliac fossa (RIF), along with their symptoms. We classified them in five different diagnostic categories presented in the radiological report: normal appendix, non-visible appendix and no secondary signs, non-conclusive, probable appendicitis, certain appendicitis. By mean of the Stata14 software descriptive analysis, T-test and Chi-square were performed and the data were compared with the final pathological report.
ResultsPopulation: 139 patients (45% men, 55% women), mean age: 32.68 (15–84). Prevalence of acute appendicitis: 50.35% (70/139). Negative appendicectomy rate: 0%. Negative predictive value for the categories 1, 2 and 3 taken together: 9078%. Positive predictive value for the categories 4 and 5 taken together: 100%. Ultrasound sensibility and specificity 90% and 100%, respectively. Statistically significant signs and symptoms (p<0.05): RIF pain, fever, leukocytosis, left shift, visible appendix, non-compressibility, hyperechogenic fat, appendicolith and free fluid.
ConclusionUltrasound is very accurate for the diagnosis of acute appendicitis in adults.
Evaluar la fiabilidad de la ecografía para el diagnóstico de la apendicitis aguda en los adultos, calcular la tasa de apendicectomías negativas en los pacientes intervenidos, calcular el valor predictivo de las categorías diagnósticas predefinidas e identificar los signos y síntomas significativos para apendicitis aguda.
Material y métodosEstudio descriptivo prospectivo en que se recogieron los hallazgos de las ecografías urgentes solicitadas en un año para pacientes adultos con dolor en la fosa ilíaca derecha (FID), juntos con sus síntomas. Se clasificaron en 5 categorías diagnósticas reflejadas en el informe radiológico: apéndice normal, apéndice no visible y ausencia de signos secundarios, no concluyente, apendicitis probable, apendicitis segura. Con el programa Stata14 se realizaron el análisis descriptivo, el T-test y el Chi cuadrado y los datos se compararon con el diagnóstico anatomopatológico final posquirúrgico.
ResultadosPoblación: 139 pacientes (45% hombres, 55% mujeres), edad media: 32,68 (15-84). Prevalencia de apendicitis aguda: 50,35% (70/139). Tasa de apendicectomías negativas: 0%. Valor predictivo negativo de los grupos 1, 2 y 3 conjuntamente: 90,78%. Valor predictivo positivo de los grupos 4 y 5 conjuntamente: 100%. Sensibilidad y especificidad de la ecografía: 90% y 100% respectivamente. Signos y síntomas significativos para apendicitis aguda (p<0.05): dolor en la FID, fiebre, leucocitosis, desviación izquierda, apéndice visible, apéndice no compresible, grasa hiperecogénica, apendicolito, líquido libre.
ConclusionesLa ecografía es muy fiable para diagnosticar apendicitis aguda en los adultos.
Acute appendicitis is an abdominal emergency. It is highly prevalent in the western world and is more frequently associated with non-elective abdominal surgery than any other condition. According to the literature, its lifetime incidence is estimated at between 7% and 12% in the general population, with peak prevalence in the second and third decades of life.1–3
Diagnostic suspicion of acute appendicitis is traditionally clinical,4 and several patient stratification systems based on physical examination and complementary tests have been proposed in recent years. The most widely used is the Alvarado scoring system, which includes several variables, the most important being pain in the right iliac fossa (RIF) and leukocytosis of more than 10,000/mm3. However, several studies have shown the system to have limited negative predictive value (NPV), especially in patients with an intermediate score5,6 and it correlates poorly with imaging tests.7 For this reason, imaging studies are usually requested in most cases to confirm or rule out the diagnosis of acute appendicitis.
The aims of this study are: (a) to evaluate the usefulness, sensitivity and specificity of ultrasound to diagnose acute appendicitis in adults in our hospital; (b) to calculate the incidence of negative appendectomies in operated patients with an ultrasound diagnosis of acute appendicitis; (c) to calculate the predictive value of predefined presumptive diagnosis categories; and (d) to identify the most significant ultrasound signs and clinical variables for acute appendicitis.
Material and methodsWe performed a prospective, descriptive study of all emergency ultrasound scans of adult patients (older than 15 years) with RIF pain and suspicion of acute appendicitis performed by the radiodiagnosis department on request from the emergency department between April 2015 and April 2016. We did not include indication criteria for ultrasound, since this is the initial diagnostic imaging test in all patients.
The study was approved by our hospital's independent ethics committee. No informed consent was required since the study variables collected do not include any personal patient data.
The patients were evaluated by the hospital's emergency department doctors, and all the clinical and analytical variables were recorded in the medical record, which can be immediately accessed by the radiodiagnosis department on the combined RIS (Radiology Information System) and online clinical record system used in our institution.
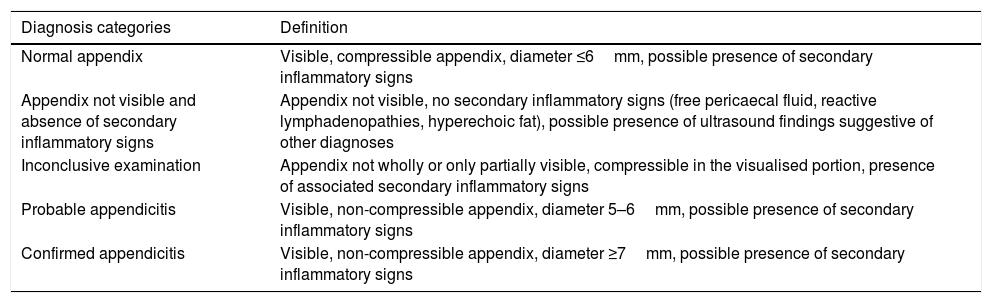
All the doctors and residents in our department were informed of the study and contributed to data collection. The test report, together with a description of the ultrasound findings, contained one of the presumptive diagnoses included in the five categories defined in Table 1: visible, normal appendix; non-visible appendix and absence of secondary inflammatory signs; inconclusive examination; probable appendicitis; and confirmed appendicitis. We defined the diagnostic categories for use in adult patients, based on our previous experience and on evidence in the medial literature.
Definition of presumptive diagnosis categories.
| Diagnosis categories | Definition |
|---|---|
| Normal appendix | Visible, compressible appendix, diameter ≤6mm, possible presence of secondary inflammatory signs |
| Appendix not visible and absence of secondary inflammatory signs | Appendix not visible, no secondary inflammatory signs (free pericaecal fluid, reactive lymphadenopathies, hyperechoic fat), possible presence of ultrasound findings suggestive of other diagnoses |
| Inconclusive examination | Appendix not wholly or only partially visible, compressible in the visualised portion, presence of associated secondary inflammatory signs |
| Probable appendicitis | Visible, non-compressible appendix, diameter 5–6mm, possible presence of secondary inflammatory signs |
| Confirmed appendicitis | Visible, non-compressible appendix, diameter ≥7mm, possible presence of secondary inflammatory signs |
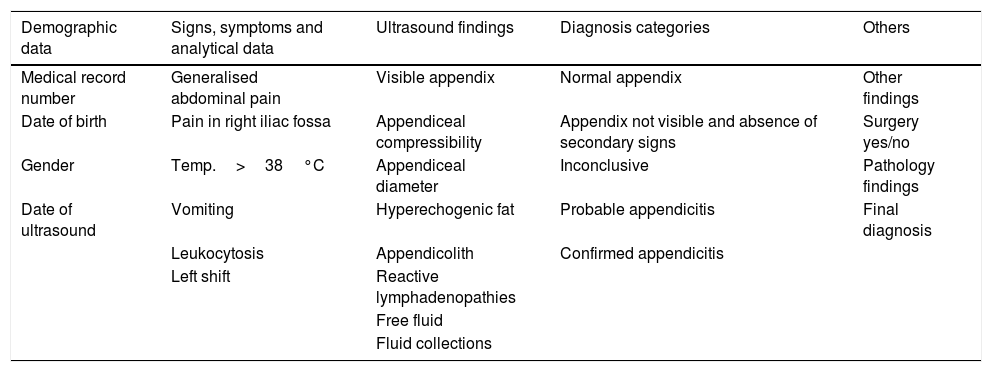
Once the ultrasound was completed, the corresponding data were entered in an Excel spreadsheet (Table 2). The ultrasound findings collected were: visibility of the appendix, compressibility, appendiceal diameter, hyperechoic fat, presence of appendicolith, reactive lymphadenopathy, free fluid, fluid collections or other relevant findings, and the patient's diagnostic category. A small amount of free fluid in a woman of childbearing age was considered a physiological finding.
Study variables, classified by groups.
| Demographic data | Signs, symptoms and analytical data | Ultrasound findings | Diagnosis categories | Others |
|---|---|---|---|---|
| Medical record number | Generalised abdominal pain | Visible appendix | Normal appendix | Other findings |
| Date of birth | Pain in right iliac fossa | Appendiceal compressibility | Appendix not visible and absence of secondary signs | Surgery yes/no |
| Gender | Temp.>38°C | Appendiceal diameter | Inconclusive | Pathology findings |
| Date of ultrasound | Vomiting | Hyperechogenic fat | Probable appendicitis | Final diagnosis |
| Leukocytosis | Appendicolith | Confirmed appendicitis | ||
| Left shift | Reactive lymphadenopathies | |||
| Free fluid | ||||
| Fluid collections |
After determining the patient's diagnostic category, the management strategy was agreed with the hospital's emergency and general and gastrointestinal surgery departments, and consisted of:
- 1.
Clinical follow-up or discharge with another diagnosis (categories 1 and 2).
- 2.
Completion of the study with computed tomography (CT) of the abdomen, either contrast-enhanced during the portal phase, or without contrast in the case of renal failure or allergy, using 5-mm slices. For this purpose, a Toshiba Aquilion 64 (Toshiba Medical Systems Corporation, Otawara, Japan) CT system was used. In other cases, the patient was kept under observation for 24h, and the ultrasound study was repeated, depending on the clinical or analytical evolution (category 3).
- 3.
Surgery (categories 4 and 5).
Ultrasound studies were performed with a Philips Affiniti 70G system (Philips Medical Systems, Eindhoven, The Netherlands). First, an overall study of the abdomen was performed using a 5-MHz convex transducer, then a 12-MHz linear transducer was used to examine the RIF, particularly at the point of maximum pain reported by the patient, using the graded-compression technique originally described by Puylaert8 to displace intestinal gas and thus prevent artefacts. In all cases in which the appendix was not easily visualised, a maximum of 20min was assigned to RIF study.
In patients who underwent surgery, the pathological findings were reviewed and added to the data collection spreadsheet once they were available in the electronic medical record.
All patients with an alternative diagnosis were considered negative for acute appendicitis and their data was followed up in the hospital's computer system to confirm that they had not received a diagnosis of acute appendicitis in the month immediately after discharge.
The data were analysed using the statistical programme Stata14 (Stata Corporation, College Station, TX). We performed a descriptive analysis, calculating the NPV of the no appendicitis, visualised appendix and absence of indirect signs, and inconclusive examination categories; calculating the positive predictive value (PPV) of the probable and confirmed appendicitis categories; calculating the sensitivity and specificity of ultrasound for the diagnosis of acute appendicitis; and using the χ2 test with contingency tables to test dichotomous variables, and the Student's t test for the appendiceal diameter.
ResultsThe study population consisted of 139 patients with a mean age of 32.68 years (range 15–84 years), 76 women (54.68%) and 63 men (45.32%). The prevalence of acute appendicitis in our sample, confirmed by pathological findings, was 50.35% (70 out of 139).
The sensitivity and specificity of ultrasound for the diagnosis of acute appendicitis in adults in our study was 90% and 100%, respectively.
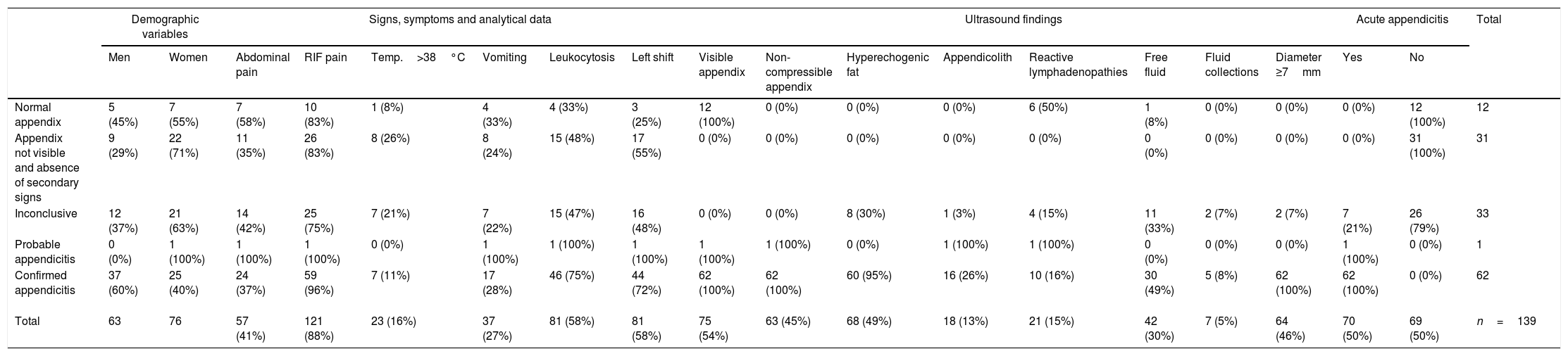
Table 3 shows the analytical data, signs and symptoms, and ultrasound findings, arranged according to diagnostic category.
Results by diagnosis category (percentages in parentheses).
| Demographic variables | Signs, symptoms and analytical data | Ultrasound findings | Acute appendicitis | Total | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Abdominal pain | RIF pain | Temp.>38°C | Vomiting | Leukocytosis | Left shift | Visible appendix | Non-compressible appendix | Hyperechogenic fat | Appendicolith | Reactive lymphadenopathies | Free fluid | Fluid collections | Diameter ≥7mm | Yes | No | ||
| Normal appendix | 5 (45%) | 7 (55%) | 7 (58%) | 10 (83%) | 1 (8%) | 4 (33%) | 4 (33%) | 3 (25%) | 12 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 6 (50%) | 1 (8%) | 0 (0%) | 0 (0%) | 0 (0%) | 12 (100%) | 12 |
| Appendix not visible and absence of secondary signs | 9 (29%) | 22 (71%) | 11 (35%) | 26 (83%) | 8 (26%) | 8 (24%) | 15 (48%) | 17 (55%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 31 (100%) | 31 |
| Inconclusive | 12 (37%) | 21 (63%) | 14 (42%) | 25 (75%) | 7 (21%) | 7 (22%) | 15 (47%) | 16 (48%) | 0 (0%) | 0 (0%) | 8 (30%) | 1 (3%) | 4 (15%) | 11 (33%) | 2 (7%) | 2 (7%) | 7 (21%) | 26 (79%) | 33 |
| Probable appendicitis | 0 (0%) | 1 (100%) | 1 (100%) | 1 (100%) | 0 (0%) | 1 (100%) | 1 (100%) | 1 (100%) | 1 (100%) | 1 (100%) | 0 (0%) | 1 (100%) | 1 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | 0 (0%) | 1 |
| Confirmed appendicitis | 37 (60%) | 25 (40%) | 24 (37%) | 59 (96%) | 7 (11%) | 17 (28%) | 46 (75%) | 44 (72%) | 62 (100%) | 62 (100%) | 60 (95%) | 16 (26%) | 10 (16%) | 30 (49%) | 5 (8%) | 62 (100%) | 62 (100%) | 0 (0%) | 62 |
| Total | 63 | 76 | 57 (41%) | 121 (88%) | 23 (16%) | 37 (27%) | 81 (58%) | 81 (58%) | 75 (54%) | 63 (45%) | 68 (49%) | 18 (13%) | 21 (15%) | 42 (30%) | 7 (5%) | 64 (46%) | 70 (50%) | 69 (50%) | n=139 |
RIF: right iliac fossa.
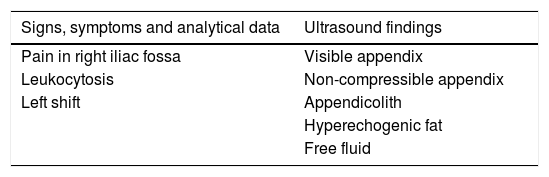
With regard to signs, symptoms and analytical data, most patients presented RIF pain (88.49%) and leukocytosis (58.27%); both these variables, together with left shift in the leucocyte count, were statistically significant for the final diagnosis of acute appendicitis (p<0.05) (Table 4).
Of the total number of patients with suspected acute appendicitis (n=139), the appendix was visualised in 75 (53.95%), and was non-compressible in 63 (84%) cases. In seven of the 64 patients in whom the appendix could not be visualised, the final diagnosis was acute appendicitis; therefore, no visualisation of appendix had an NPV of 89% in our sample.
Hyperechoic fat in the RIF was found in 68 patients (48.92%), and free fluid in 42 (30.21%). In 18 cases (12.94%), an appendicolith obstructed the appendiceal lumen. All the foregoing ultrasound findings were statistically significant (p<0.05) for the final diagnosis of acute appendicitis (Table 4).
The ultrasound findings of non-compressible appendix and hyperechoic fat in the RIF are both sensitive and specific for acute appendicitis, with a PPV of 93% and 87%, respectively, and an NPV of 85% and 86%.
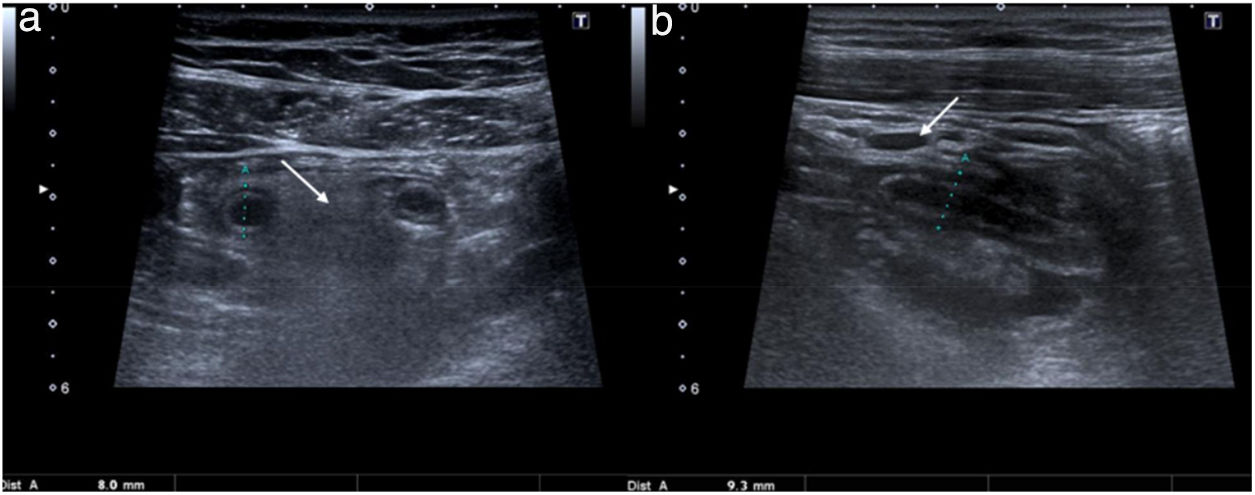
Mean appendiceal diameter in patients without appendicitis (n=12) was 4.77mm, and for confirmed cases of acute appendicitis (n=63) the average diameter was 9.48mm (Fig. 1). This variable was significant on the Student's t test (p<0.01), although the difference between means varied from 3.33 to 6.10mm (95% confidence interval [CI]).
All patients included in categories 4 and 5 (n=63) underwent surgery; there were 0 cases of negative appendectomy.
For practical purposes, category 3 (inconclusive examination) was considered negative for acute appendicitis; therefore, the pooled NPV for categories 1, 2 and 3 was 90.78%.
The NPV of categories 1 and 2 was 100%.
The pooled PPV of categories 4 and 5 was 100%.
The classification of patients according to their preliminary diagnostic category (Table 1) was as follows: 12 (8.63%) patients in category 1 (normal appendix), 31 (22.30%) in category 2 (non-visible appendix and absence of secondary inflammatory signs), 33 (23.74%) in category 3 (inconclusive), 1 (0.70%) in category 4 (probable appendicitis) and finally, 62 (44.60%) patients in category 5 (confirmed appendicitis).
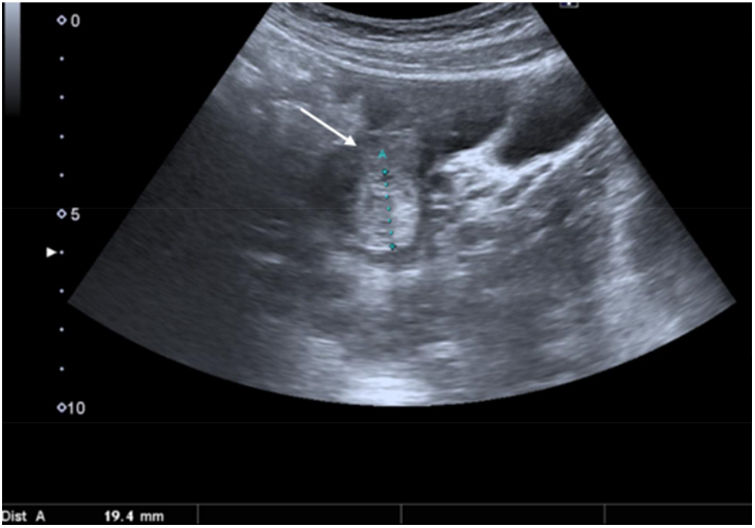
Category 1 (Fig. 2): all 12 patients were either discharged without further complications or the alternative condition diagnosed was treated and recorded in the hospital discharge report (nonspecific abdominal pain, acute gastroenteritis, renal colic, urinary tract infection, biliary colic, pelvic inflammatory disease, mesenteric lymphadenitis). In one case, free fluid was observed in the pelvis but was considered physiological (woman of reproductive age), and in six cases reactive lymphadenopathies were observed (final diagnosis of mesenteric lymphadenitis).
Category 2: alternative diagnoses in this category were nonspecific abdominal pain, acute gastroenteritis, urinary tract infection, biliary colic and renal colic.
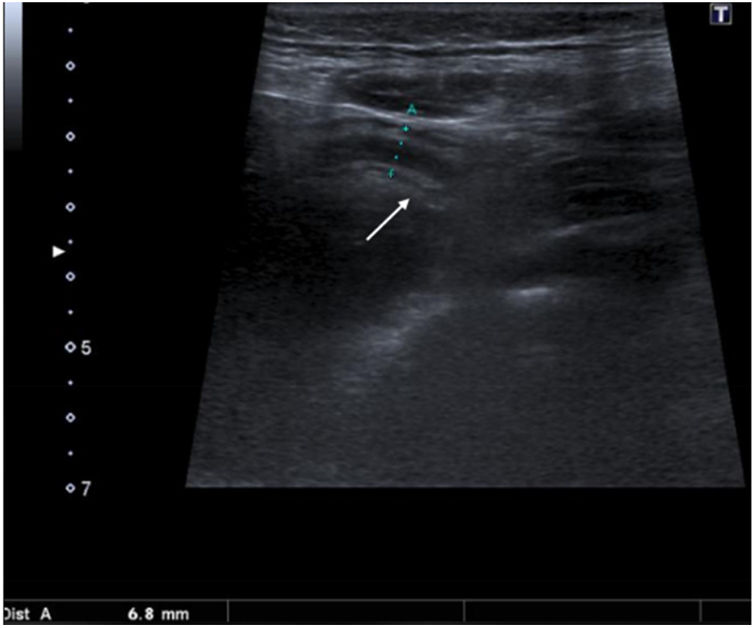
Category 3: two women included in this category had hyperechogenic free fluid in the region of the right adnexa (Fig. 3). In one case it was due to haemoperitoneum secondary to rupture of a haemorrhagic follicular cyst in an anticoagulated patient, and in the other it was due to rupture of a haemorrhagic follicular cyst. In another four patients of childbearing age, who were discharged after observation, small amounts of anechoic fluid observed around the right adnexa were considered physiological. In 23 of the 33 patients in this category (Fig. 4), the radiological study was completed with ultrasound at 24h (n=7) or with a CT scan of the abdomen (n=16); acute appendicitis was diagnosed in seven cases (Fig. 5) and alternative conditions in eight (perforated right diverticulitis, perforated duodenal ulcer, probable pelvic inflammatory disease, renal colic, acute diverticulitis, omental infarction, typhlitis). The remaining patients were discharged after confirming significant clinical–analytical improvement after 24hours of observation (nonspecific abdominal pain, urinary tract infection). In this category, a comparison of patients with a final diagnosis of acute appendicitis vs no acute appendicitis found no statistically significant differences in ultrasound findings that could lead to greater diagnostic accuracy.
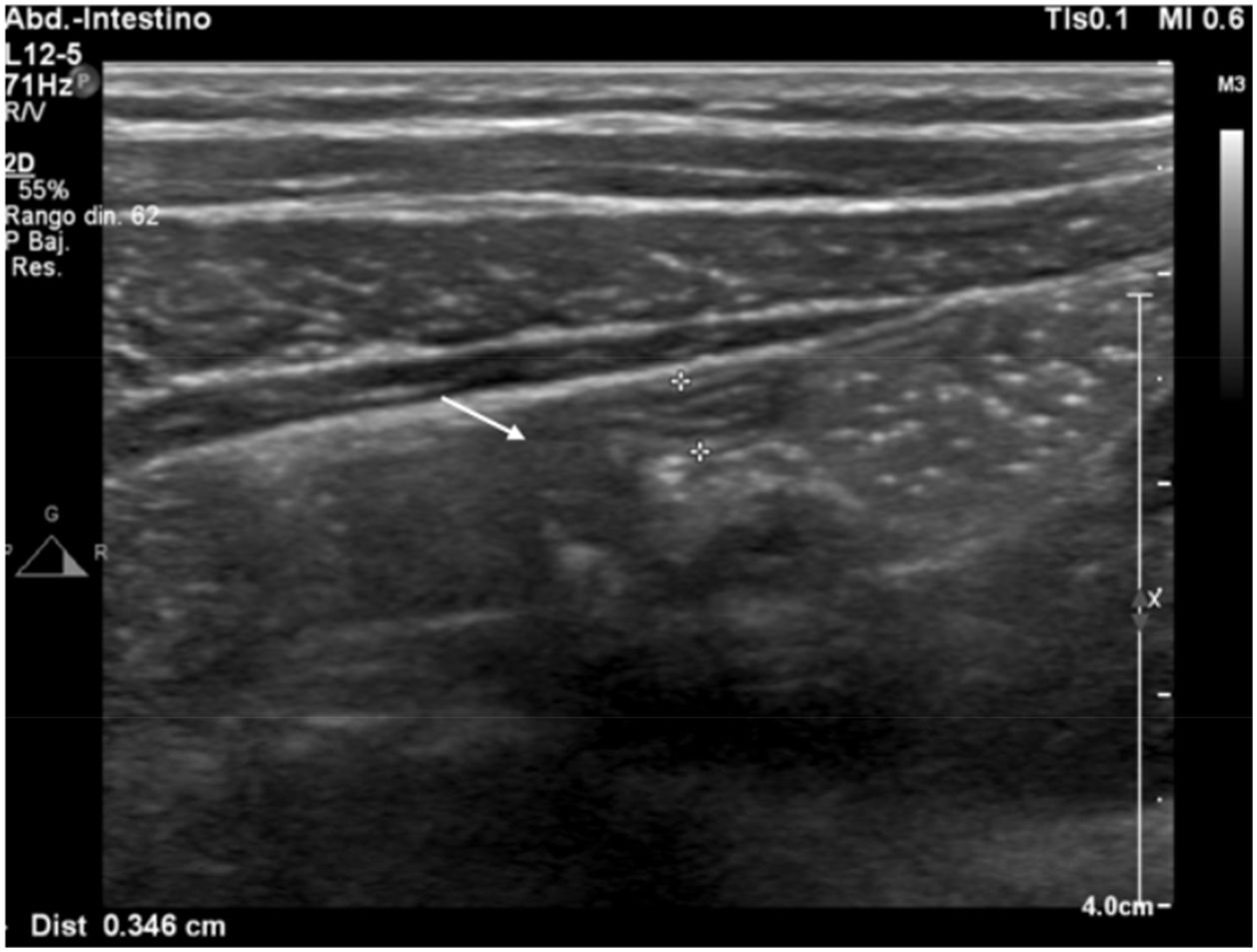
Ultrasound. Transversal view of the right iliac fossa. Segment of enlarged, but compressible, appendix (between markers). It was not possible to visualise the entire appendix, and it was also associated with hyperechogenic fat (arrow), so it was included in category 3 (inconclusive). Follow-up ultrasound at 24h showed an increase in diameter and the patient underwent surgery (final diagnosis of acute appendicitis).
Category 4: this category included one patient who, despite symptoms, ultrasound findings (non-compressible appendix, appendicolith and reactive lymphadenopathies) and laboratory results highly suggestive of acute appendicitis, presented an appendix with a diameter of 6mm. Despite this, the patient underwent surgery and the final diagnosis of acute appendicitis was confirmed.
Category 5 (Fig. 6): all 62 patients underwent surgery and the diagnosis of acute appendicitis was confirmed with the pathological study. In one case, the condition was associated with obstruction of the appendiceal lumen by a carcinoid tumour of the base of the appendix.
DiscussionUltrasound should be the first-choice imaging study in patients with acute RIF pain. The technique is inexpensive, widely available and free from ionising radiation, which makes it particularly suitable for children and women of childbearing age. It is also an interactive, dynamic examination that can evaluate the area of maximum pain in real time, and provides valuable information on, for example, vascular abnormalities and intestinal peristalsis. However, ultrasound is highly operator-dependent and is of little use in obese patients, in cases of retrocaecal appendix or in patients with severe pain that prevents compression with the transducer. Therefore, if diagnosis is inconclusive, the ultrasound study can be complemented with abdominal CT.9 The disadvantages of CT are ionising radiation and the risk of iodinated contrast-induced nephrotoxicity. However, unlike ultrasound, image acquisition is not operator-dependent and can be evaluated by a more experienced radiologist at a later date, if necessary.10
During ultrasound study, the operator can, and should, look for alternative causes of RIF pain if the examination is inconclusive for acute appendicitis. It is always important to bear in mind the broad differential diagnosis of this symptom, which includes diverticulitis in the right colon or in a redundant sigmoid colon, typhlitis, tumour, terminal ileitis of different aetiology, mesenteric lymphadenitis, complicated Meckel diverticulum, colitis, right renal colic, epiploic appendagitis, omental infarction, and acute gynaecological pathology (rupture of a follicular or haemorrhagic cyst, ovarian torsion or torsion of a pedunculated myoma, pelvic inflammatory disease, ectopic pregnancy).11
The diagnostic yield of ultrasound in acute appendicitis has been studied for years, reaching a peak of publications between 1980 and 2000. The technique is now well established for this indication, and in the hands of expert operators has a sensitivity and specificity of 85% and 90%, respectively12 figures which are corroborated by many studies, including systematic reviews.13,14 Other authors evaluating the diagnostic yield of ultrasound, however, have reported less favourable results, particularly in studies published in the United States or the United Kingdom, in which the sensitivity of ultrasound can be as low as 50%, with a 15% rate of negative appendectomies.15 Several factors can explain these differences; for example, in English-speaking countries ultrasounds are performed by a sonographer, and the captured images are later interpreted by a radiologist. In these countries, attempts have been made to reduce the negative appendectomy rate by stratifying patients using ultrasound finding scales combined with clinical scoring systems. Reddy et al. reported an 8% reduction in the negative appendectomy rate when this approach was used.16 However, it is difficult to understand why, after more than 20 years of scientific evidence validating its efficacy and results similar to CT, ultrasound has yet to be implemented across the board for the diagnosis of RIF pain, particularly in suspicion of acute appendicitis, in both in adults and children.10
Some years ago, a series of studies by authors from fields unrelated to radiology evaluated the diagnostic yield of ultrasound performed by non-radiologists, for example surgeons, to confirm suspected acute appendicitis.17 The studies found no statistically significant differences between surgeon-performed and radiologist-performed examinations. Although combining clinical and ultrasound examination in the same physician can improve overall accuracy in the diagnosis of acute appendicitis, the contribution made by the radiologist in searching for alternative diagnoses would be lost.
The results of our study are similar to those obtained by others who also evaluated the diagnostic yield of ultrasound performed by radiologists.
The clinical signs and symptoms and analytical data that showed a statistically significant correlation with the diagnosis of acute appendicitis in our study (RIF pain, left shift leukocytosis) are highly sensitive but not very specific, while the ultrasound findings that were statistically significant (visible appendix, free fluid and appendicolith) are more specific and less sensitive. Although various definitions of diagnostic categories can be found in studies that stratify patients according to ultrasound findings, most are focussed on paediatric patients.18,19 This is because most similar studies in adult patients evaluate clinical–analytical pretest scoring systems.20 Post-test ultrasound classification of patients into diagnostic categories gives optimum levels of sensitivity (90%), specificity (100%), NPV (90.78%) and PPV (100%), demonstrating its usefulness in both adults and children. Indeed, most efforts to prove the effectiveness of ultrasound and thus reduce the radiation dose received from a complementary CT scan have so far been focussed on children. Furthermore, the system is reproducible, it can be used as a basis for a standardised report and provides the clarity and immediacy needed by clinicians to reach an accurate diagnosis without having to interpret the radiological report themselves.
It is interesting to note that no visualisation of appendix and indirect inflammatory signs in the RIF (category 2) and normal appendix (category 1) achieved an NPV of 100%. In our study, in other words, no visualisation of appendix and no indirect inflammatory signs in the RIF had the same value as a normal appendix to rule out a diagnosis of acute appendicitis.
Thirty-three patients from our series (23.74%) met the criteria for category 3 (inconclusive examination). Of these, only 21.21% (5.03% of the total) received a diagnosis of acute appendicitis after additional imaging studies (second ultrasound or abdominal CT). This category should be reserved for patients in whom no visualisation or incomplete visualisation of the appendix together with a number of secondary inflammatory signs cannot completely rule out or confirm a diagnosis of acute appendicitis, or raises the suspicion of another condition. In this case, the ultrasound study should be used to classify the patient in another category, if feasible. In the case of an inconclusive examination, the report should suggest how the clinician should proceed: complete the study with abdominal CT or consider repeating the ultrasound after 24h of observation. In 2016, a consensus document on the diagnostic and therapeutic management of patients with suspected acute appendicitis was published following the World Society of Emergency Surgery conference. These guidelines also recommend stratifying patients into diagnostic categories (in this case on the basis of pretest probability) and performing CT only after an inconclusive ultrasound study.21
The number of negative appendectomies in our study was 0, whereas the false positive rate in the published studies that we reviewed varies between 2.8% and 18%. This could be due to several factors: adequate screening of patients with suspected acute appendicitis in the emergency department, ultrasound performed by expert radiologists or by supervised residents, and most importantly, close collaboration and smooth communication between hospital departments. The performance of additional imaging tests (follow-up ultrasound or CT) in most inconclusive cases was also a determining factor, although only one in every six patients underwent additional studies.
The percentage of appendices visualised (54%) is slightly higher than the overall figure in the literature, where only 50% or less are visualised. This is probably due to our study design, which allocated up to 20min to identify the appendix – this is longer than the 5min traditionally used in this type of study for ultrasound examination of the RIF. An interesting recent study published by Lin et al. concludes that when the appendix is not visualised with ultrasound in the RIF using a linear probe, the operator must systematically search for it in the posteromedial quadrant of the ileocaecal valve in the transverse plane, or above the iliac crest, using a sector transducer of at least 6MHz.22
Regarding the appendiceal diameter, although the difference in means between a normal and pathological appendix was statistically significant in our series, the difference in diameters between the two varies greatly. In our population, the diameters of normal and pathological appendices overlap by more than two central quartiles, particularly in the case of normal appendices that appear enlarged. Therefore, basing diagnosis exclusively on the criterion of appendiceal diameter would increase the number of false positives. The traditionally accepted upper limit of 6mm in diameter for a normal appendix is, in our experience, too sensitive, since our study has shown that a diameter of 7mm or more has a good PPV.
A number of recent articles have described how the use of colour and spectral Doppler to evaluate parietal hyperaemia of the appendix can provide additional information, especially in cases of appendiceal diameters between 6mm and 8mm. The results of these studies indicate that a continuous intramural colour Doppler signal measuring more than 3mm in length is very specific (94.9%), though not very sensitive (57.1%) for acute appendicitis.23 Similarly, peak systolic velocity rates of more than 10cm/s and resistive indices of over 0.65 have, respectively, a specificity of 94.7% and 96.5%, and a sensitivity of 88.9% and 63.9% for the diagnosis of acute appendicitis.24 These studies add an interesting new factor to consider in the case of inconclusive ultrasound findings, and introduce the spectral Doppler study as a novel field of research.
Our study has some limitations: it is descriptive, with a small number of cases, and we only analysed data from the first ultrasound imaging test, even though the diagnostic study was completed with CT in most cases where ultrasound was inconclusive. Furthermore, knowing in advance that they were participating in a study could have encouraged the radiologists to maximise care and attention when performing the ultrasound.
In conclusion, this study has contributed more evidence to the literature, advocating the use of ultrasound in suspected acute appendicitis in adults, and we have confirmed the satisfactory yield of this diagnostic technique in our hospital, since no negative appendectomies were reported during the study period. Our presumptive diagnosis categories are based on objective ultrasound findings, are reproducible and have shown good predictive values. They can help to reduce the number of inconclusive ultrasounds and the subsequent dose of radiation received from complementary CT scans, particularly in cases where no signs of pericaecal inflammation were observed, even though the appendix was not visualised. In this respect, note that in our study, 95% of patients with confirmed appendicitis manifested at least one of these signs of secondary inflammation. Furthermore, in our experience, RIF pain, leukocytosis and left shift can help clarify inconclusive studies, since they have shown significant correlation with the final diagnosis of acute appendicitis.
Authorship- 1.
Person responsible for the integrity of the study: GB and MDFP.
- 2.
Conception of the study: GB, MDFP and ALS.
- 3.
Study design: GB, MDFP and ALS.
- 4.
Data acquisition: GB, MDFP and ALS.
- 5.
Analysis and interpretation of data: GB and MDFP.
- 6.
Statistical processing: GB and MDFP.
- 7.
Literature search: GB.
- 8.
Writing: GB and ALS.
- 9.
Critical review of the manuscript with intellectually relevant contributions: MDFP.
- 10.
Approval of the final version: GB, MDFP and ALS.
The authors declare that they have no conflicts of interest.
Please cite this article as: Benedetto G, Ferrer Puchol MD, Llavata Solaz A. Sospecha de apendicitis aguda en adultos. El valor de la ecografía en nuestro hospital. Radiología. 2019;61:51–59.