Endoscopic ultrasound fine-needle aspiration (EUS-FNA) plays a major role in gastrointestinal neoplasia staging. It also proved to be an effective technique in the differential diagnosis of pancreatic lesions allowing tissue sampling for pathology evaluation.1
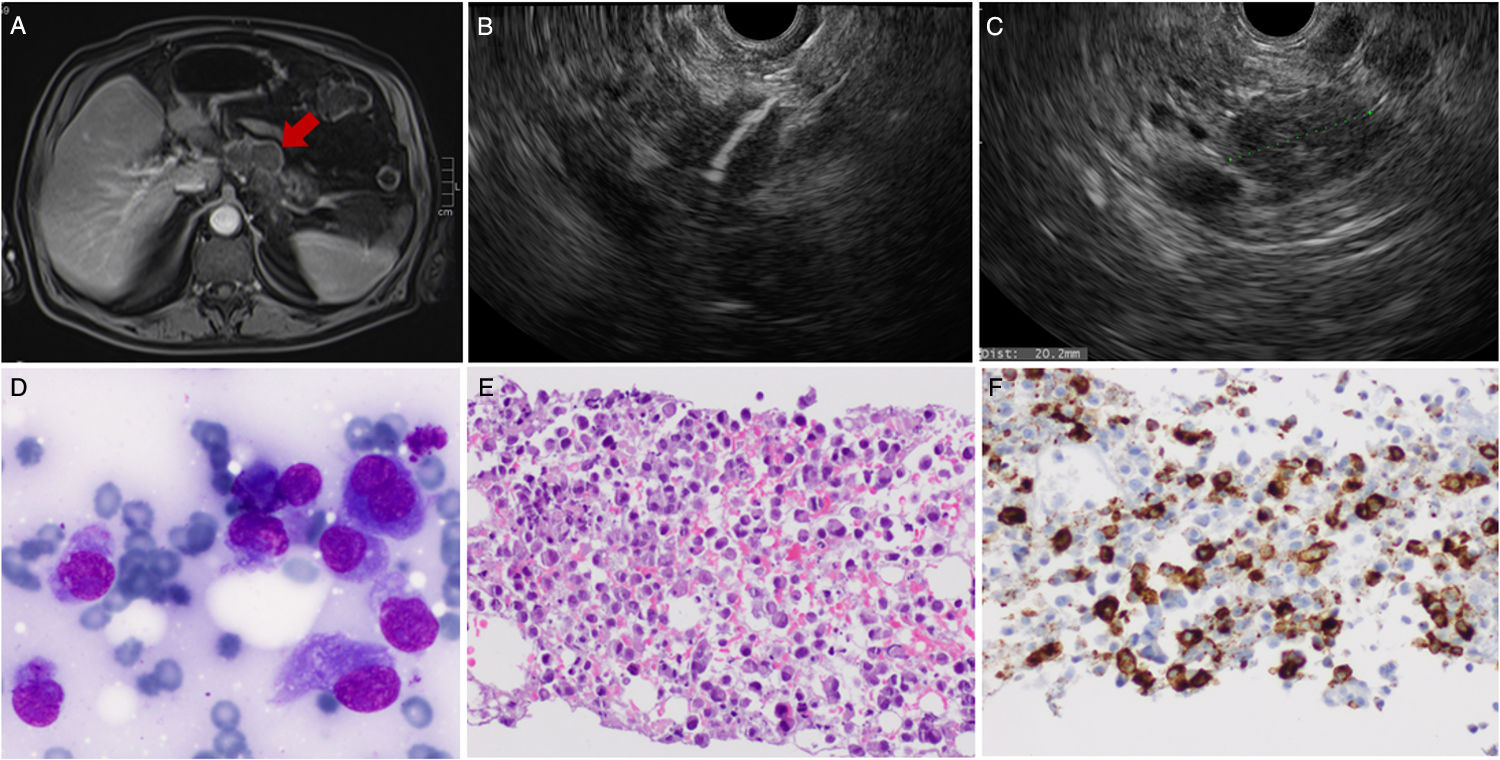
The authors report a 74 year-old male, admitted due to epigastric pain, weight loss and vomiting. His past medical history included ischaemic heart disease, hypertension, diabetes mellitus, chronic renal failure and prostatic cancer. No alcohol consumption or previous episodes of acute pancreatitis were present. The patient underwent an abdominal magnetic resonance which revealed a large, ill-defined, contrast-enhanced pancreatic neck-body mass with diffusion restriction (Fig. 1A). Laboratory evaluation was unremarkable except for mild anaemia. Serum amylase and CA19.9 was normal. Gastroenterology consultation was required and the patient was scheduled for an EUS. A 20mm heterogeneous eccentric pancreatic body mass extending to the retroperitoneum was observed. The lesion displayed positive Doppler sign (fine flow) with celiac trunk abutment although without evidence for vascular invasion. FNA through the stomach using a 25 gauge needle (two passes) was performed with air-suction aspiration (10cc and 5cc) (Fig. 1B and C). No lymph nodes were noted. Cytopathology identified cells with large granular cytoplasm and peripheral nuclei with prominent round nucleolus. Immunohistochemistry was positive for CD34, CD68, vimentin and CD71, being negative for myeloperoxidase (MPO) and for the usual epithelial and neuroendocrine markers (Fig. 1D–F). The diagnosis of a primary pancreatic MS was assumed. Acute myeloid leukaemia/bone marrow infiltration was excluded. After haematology consultation the patient was proposed for chemotherapy but died few weeks after the diagnosis due to rapid disease progression and decompensation of his medical comorbidities.
Heterogeneous mass arising from the pancreatic body and extending to the retroperitoneum, observed in abdominal magnetic resonance (A) and EUS (B). The lesion was punctured through EUS-FNA (25G). Cytopathology showed cells with large granular cytoplasm and prominent nuclei (A+B). Immunohistochemistry was strongly positive for CD 34 (C) but also for CD 68, vimentin and CD 71. These findings allowed the diagnosis of myeloid sarcoma.
Myeloid sarcoma (MS), also known as granulocytic sarcoma or chloroma, is a solid haematological neoplasia composed by immature myeloid progenitors located outside the bone marrow. This rare condition may occur simultaneously with acute myeloid leukaemia as an extramedullary disease manifestation in 2–10% of the cases, although it may precede its diagnosis or be observed when the disease relapse after treatment. Isolated MS is atypical, being characterized by absence of bone barrow and peripheral blood involvement. It may affect the digestive system leading to common misdiagnosis.2,3
The first case of pancreatic MS was described in 1987. Actually, these pancreatic lesions are extremely rare with approximately 17 cases reported in literature and only 7 presenting as an isolated condition. Clinical manifestations are usually unspecific and radiological features often mimic pancreatitis or pancreatic adenocarcinoma. Normal tumour markers and routine blood tests are usual. MS diagnosis remains challenging and pathological analysis with immunohistochemistry is crucial to differentiate MS from other pancreatic neoplasms, often requiring an expert pathologist. Positive immunostaining for MPO, CD 68, CD 45, CD 34 and/or CD 43 is common. Although MPO has a high sensitivity and specificity for myeloid cells, being an important marker for MS diagnosis, some authors reported its expression only in 66% of the cases, which is also dependent on the type of sampling and the differentiation of neoplastic cells.2–5
Chemotherapy and radiotherapy are valid therapies however, the prognosis is generally poor.4
In previous described cases of pancreatic MS, diagnosis was suspected by radiologic imaging and in some patients only performed after surgical resection. To the best of our knowledge, a definite diagnosis through EUS-FNA had never been accomplished. This case report describes the EUS features of this uncommon disease and proves the accuracy of the cytopathological diagnosis in this clinical setting. The routine preoperative characterization of solid pancreatic lesions through EUS-FNA must be considered aiming to avoid useless surgeries and futile therapeutic interventions.
Financial supportNot applicable.
Conflicts of interestThere are no financial or other conflicts of interest regarding this article.