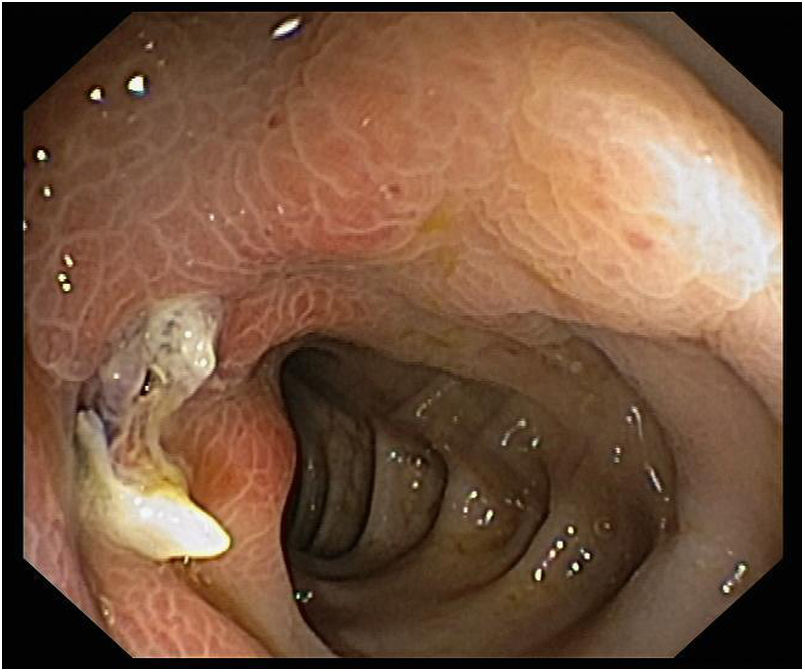
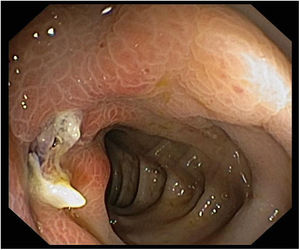
A 63 years-old female presented to the emergency department with severe left lower quadrant abdominal pain and nausea. She denied diarrhea, bloody stools or fever. Previous medical history included atrial fibrillation and dyslipidemia, and she was medicated with rivaroxaban 20mg, bisoprolol 5mg, propafenone 150mg and rosuvastatin. On physical examination, she was afebrile, and her vital signs were stable; abdominal palpation showed tenderness in the left lower quadrant. Laboratory evalutation revealed increased inflamatory parameters (leukocytes 13.9×109/L, C-reactive protein 83.4mg/L). On computed tomography scan, a segmental thickening of the descending colon with intense mucosal enhancement and pericolonic fat stranding were observed and interpreted as segmental ischemic colitis. Rare diverticula were identified. The patient underwent colonoscopy, which showed at 40cm of anal verge a short inflamed segment with edema and erythema, where a pus-draining diverticulum was identified (Fig. 1). The findings were consistent with acute diverticulitis. The patient received medical treatment and she recovered uneventfully.
The diagnosis of acute diverticulitis is often suspected in patients with lower abdominal pain and elevated inflammatory parameters.1 Computed tomography scan is helpful to confirm the diagnosis.1 When other diagnoses seem more likely, colonoscopy may be performed. We describe a patient in whom diverticulitis was diagnosed by colonoscopy.
Conflict of interest statementNo conflicts of interest to declare.