Introduction
Pharyngitis, along with rhinitis, is the most common reason for being seen by a primary care doctor in
Spain.1 It is also one of the most common reasons for prescribing antibiotics in our country, with an estimated prescription rate of 80%1-3; despite this, only 50% of pharyngitis in children and 15%-25% of adults is of bacterial origin.2-4 It should be systematically treated with antibiotics as, according to meta-analyses carried out, most pharyngitis is cured without antibiotics being given.5 Only infections caused by Streptococcus pyogenes or group A beta-haemolytic Streptococcus (GABHS) require the use of an antibiotic, as it stops the transmission and spreading of S pyogenes in the community, reduces the symptomatology compared to the non-treated group in a mean of 16 hours, and because it prevents suppurative complications. According to the Cochrane review, for every 100 patients treated with antibiotics compared to the group assigned to the placebo it produces 1 case less of rheumatic fever, 2 cases less of acute otitis media, and 3 cases less of peritonsillar abscess.5,6 However, the majority of studies included in this review were carried out in the 1950's and 60's, and the incidence of complications is much less in the last 20 years or so than in the period when these clinical studies were performed.7 A paper was recently published in the United Kingdom confirmed that the decrease in prescribing antibiotics for the treatment of pharyngitis in the last few years is not accompanied by a greater number of cases of rheumatic fever or peritonsillar abscesses.8 Acute pharyngitis creates problems for the primary care doctor, since it is difficult to clinically differentiate the aetiology due to GABHS from that of nonstreptococcal origin. Its diagnostic standard is still the pharyngeal culture, but this has significant limitations, such as the delay in obtaining the results and, also, it does not help in distinguishing between acute infection and a carrier state.
Clinical criteria are normaly used in practice to identify patients who need to be treated with antibiotics. In this case, the most well-known are the 4 criteria proposed by Centor9: presence or history of fever, tonsillar exudate, painful lateral cervical lymph nodes, and absence of cough. Later, McIsaac also included age, with an age less than 15 years being considered as another criterion.10 In the last few years, new rapid antigen techniques (RAT) have been developed for the diagnosis of acute pharyngeal tonsillitis caused by GABHS, with improved sensitivity and specificity than those of the 1990's. In this study we aim to assess the validity of the Genzyme OSOM StrepA in patients with 2 or more Centor criteria.
Methods
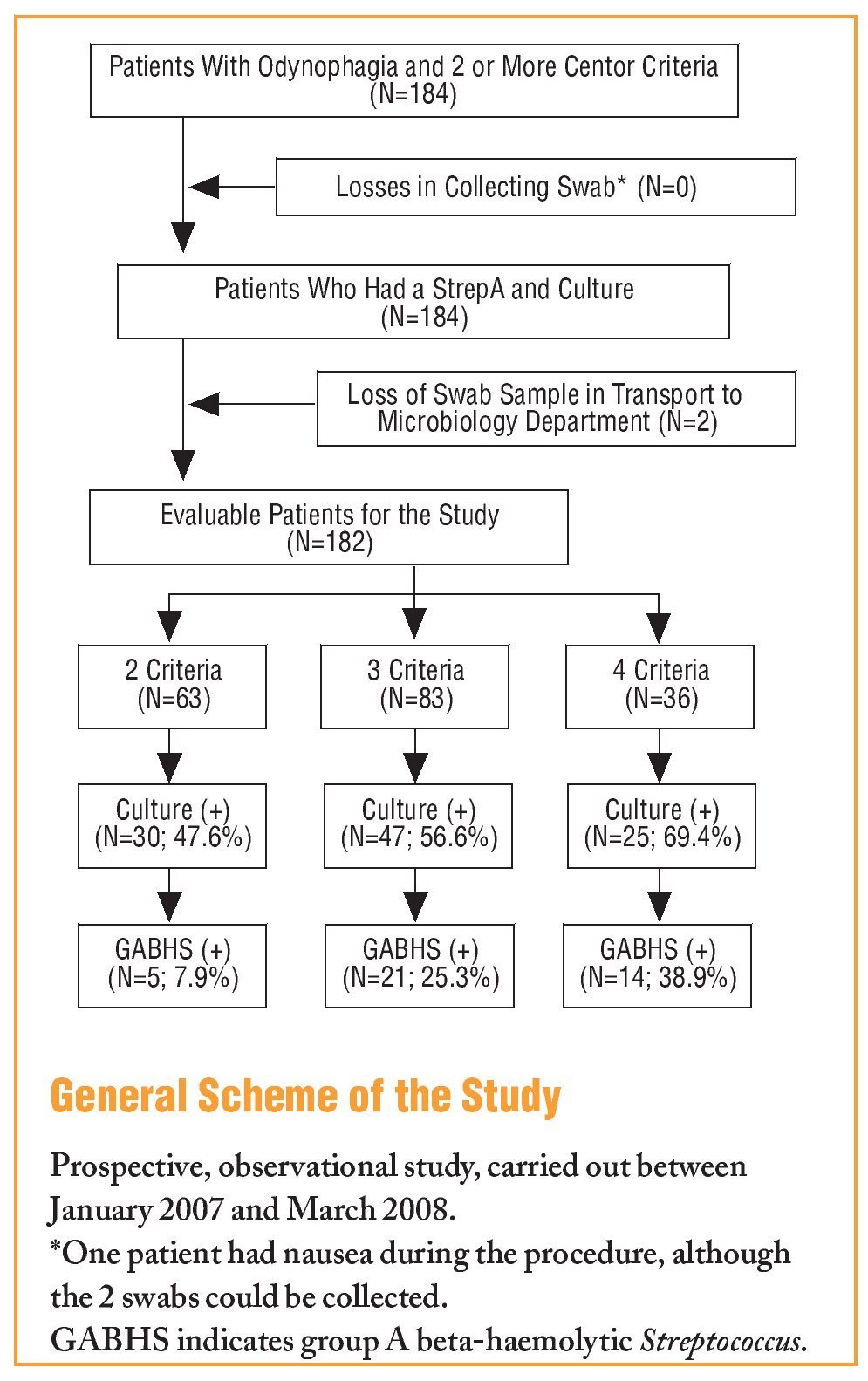
This was a prospective observational study carried out between January 2007 and March 2008. Patients over 14 years old seen in 6 clinics in our health centre were consecutively include if they had clinical symptoms of odynophagia and 2 or more of Centor criteria: tonsillopharyngeal exudate, painful lateral cervical lymph nodes, absence of cough, and/or presence or history of fever (>38oC). Patients were excluded if they had received antibiotic treatment in the previous 2 weeks and if a swab could not be collected. The sample size was calculated to be 170 subjects for a precision of 6% and expected proportion of 20%, with a 95% confidence interval (95% CI). A data report form was prepared which contained, age, sex, presence of these 4 criteria and whether the infection was recurrent (less than 2 months since the last episode) or non-recurrent.Two samples were taken for the culture from each patient for this study, by swabbing the tonsils and/or posterior wall of the pharynx with a swab, without touching the tongue, teeth or gums. The samples were taken by the 6 family doctors who had been previously trained to carry out the correct technique. OSOM StrepA (Laboratorio Genzyme) following the manufacturers instructions, was performed on one of the samples. The other swab, using an AMIES type transport medium (Copan Innovation Italy), was sent to the Microbiology Department of the Joan XXIII Hospital, Tarragona, Spain. It was cultivated on a blood agar plate and incubated at a temperature of 37oC in a 5% CO2 atmosphere for 48 hours. The culture was considered positive for S pyogenes if there was, growth of any number beta-haemolytic colonies, a positive Gram stain with streptococcal morphology, and a negative catalase test, with subsequent identification using a WIDER automated screen (Francisco Soria Melguizo) for Gram positive cocci. The results were then confirmed by serotyping using the Streptococcal Grouping Kit (Oxford, United Kingdom). The culture was considered negative if there were no beta-haemolytic colonies seen after 48 hours incubation.
For the statistical analysis, the c2 test was used for the analysis of the qualitative variables and the Student-Fisher t test was used for comparing the means. The sensitivity, specificity, the positive predictive value, and the negative predictive value were calculated for the different Centor criteria and for the RAT. Values of P<.05 were considered to be statistically significant differences.
Results Results
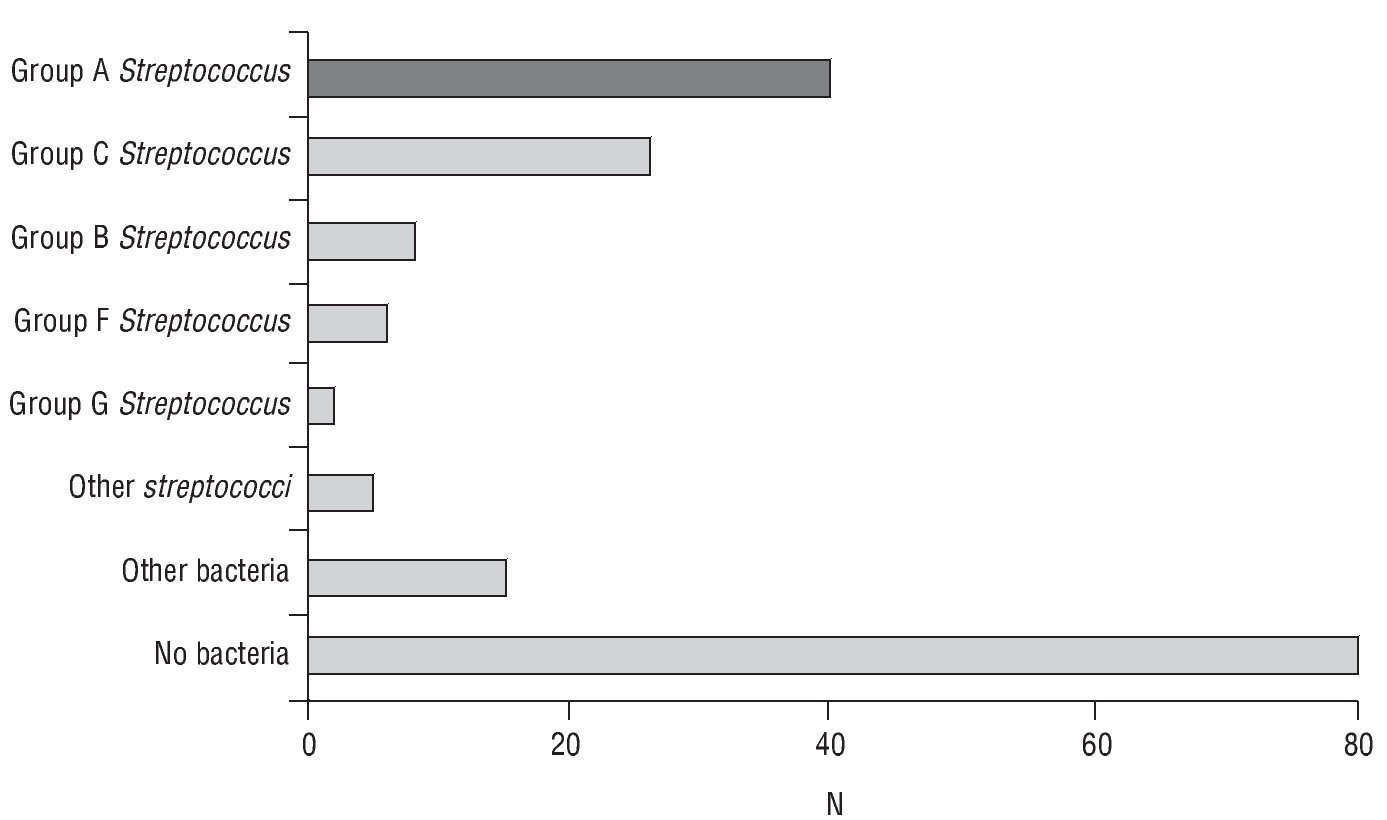
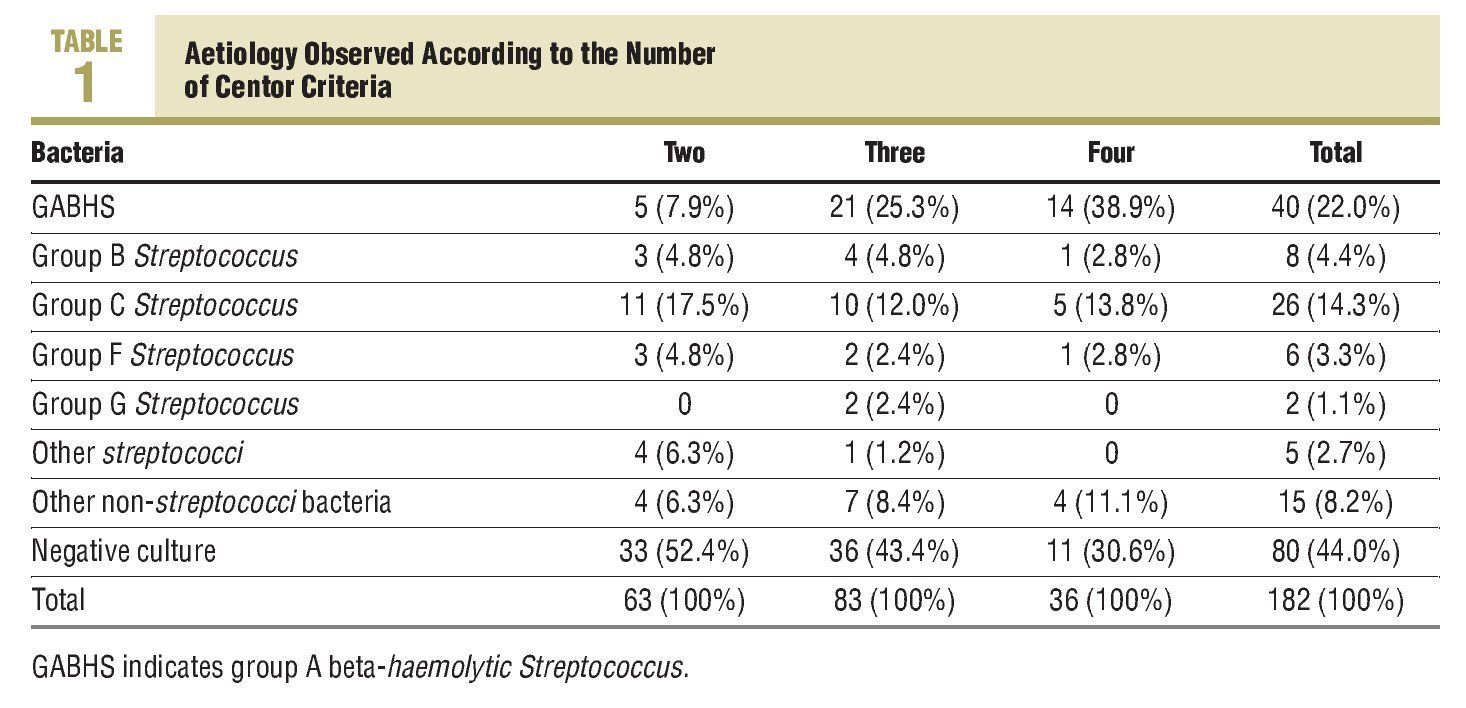
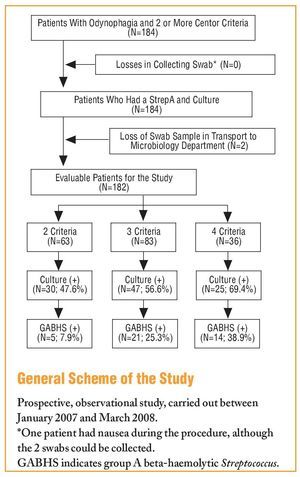
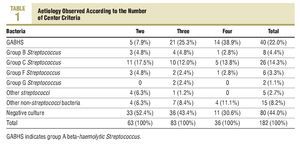
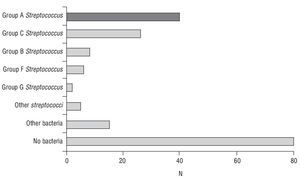
The study included 184 consecutive patients with pharyngitis symptoms and at least 2 Centor criteria, and as 2 swabs were lost in transport to the Microbiology Department, there were 182 evaluable cases (see the General Scheme of the Study). The mean age was 30.6±12.1 years, with 116 females (63.7%). A total of 63 patients had 2 Centor criteria, 83 had 3 criteria, and 36 patients with 4 criteria. The Centor criteria most often seen in the patients was, tonsillopharyngeal exudate (158 cases; 86.8%), followed by a history of fever (140 cases; 76.9%); while the least frequent was the presence of painful lateral cervical lymph nodes (89 cases; 48.9%). The culture was positive for any microorganism in 102 cases (56%), and was more common among those who had 4 criteria (25 cases; 69.4%), with no statistically significant differences seen with the other patient groups. Table 1 shows the aetiology according to the number of Centor criteria, and the different aetiological agents isolated in the cultures are shown in Figure 1.
FIGURE 1 Aetiology observed in the pharyngeal cultures.
No statistically significant differences were observed between sex and the incidence of streptococcal tonsillopharyngitis. The mean age of those with positive GABHS was slightly lower than those who had negative cultures, although no statistically significant differences were seen (29.7±11 compared to 30.9±12.3 years). The incidence of GABHS infection was significantly higher among those with 4 Centor criteria, followed by the patients with 3 criteria and then those who had only 2 criteria (P>.001).
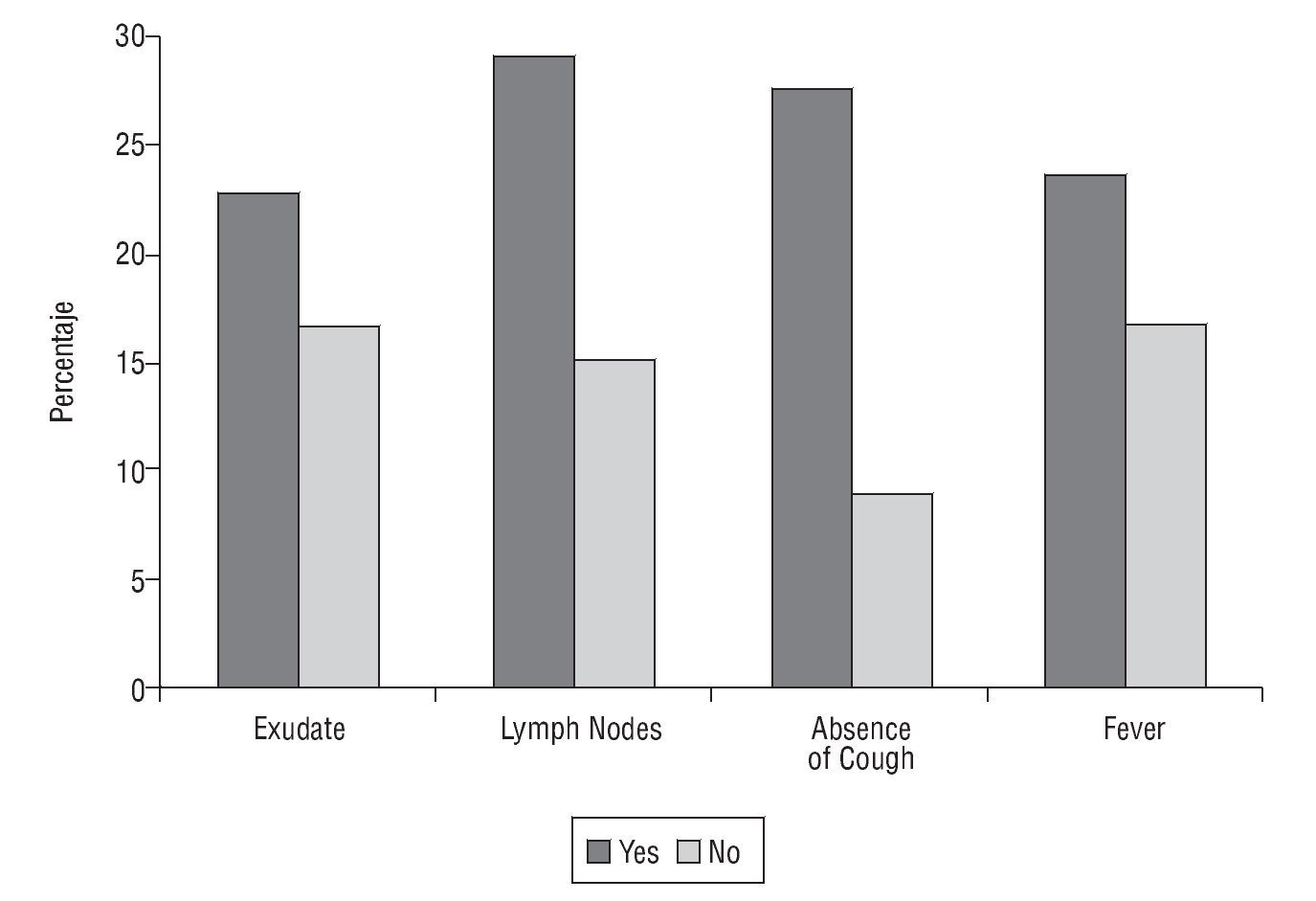
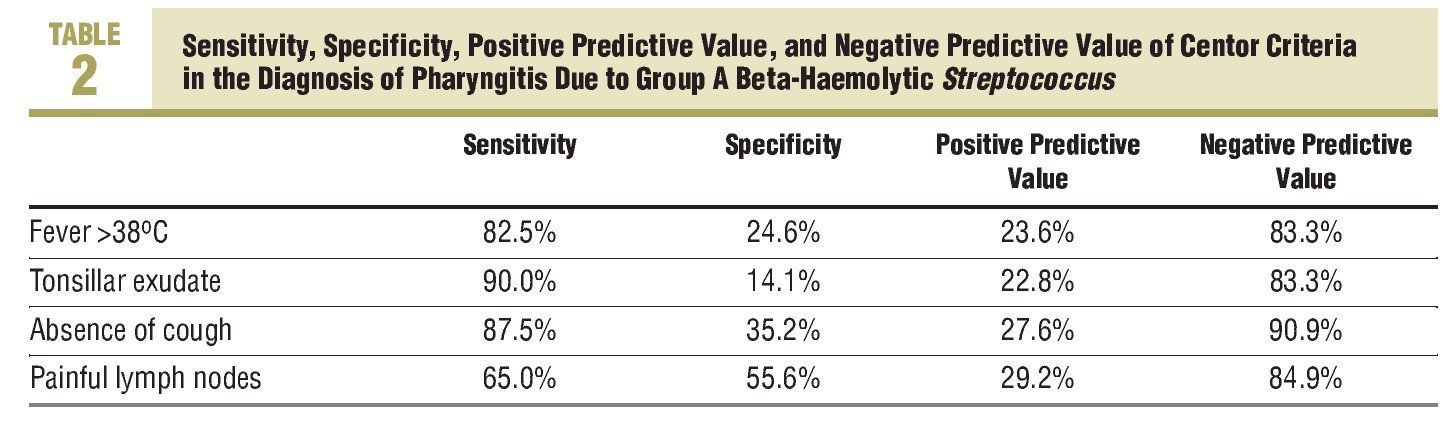
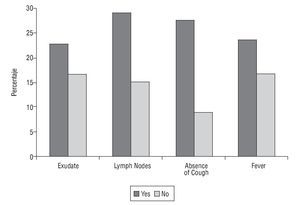
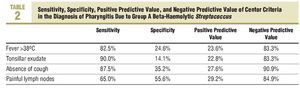
The Centor criteria associated with a higher frequency of infection due to GABHS was the absence of cough and the presence of painful lateral-cervical lymph nodes. Thus, GABHS was isolated in 27.6% of patients who did not have a cough, a significantly higher percentage than that observed among subjects who did have a cough (9.1%; P<.01). GABHS infection is seen more often among patients who have painful lateral-cervical lymph nodes (29.2% compared to 15.1% in those who do not; P<.05). Infection due to GABHS is also more frequent among those who have or had a history of fever (23.6% vs 16.7%) and among those with tonsillopharyngeal exudate (22.8% vs 16.7%). However, no statistically significant differences were observed in these 2 cases (Figure 2). Table 2 describes the validity of the Centor criteria in the diagnosis of pharyngitis due to GABHS.
FIGURE 2 Confirmed group A beta-haemolytic Streptococcus infection according to the presence or absence of Centor criteria.
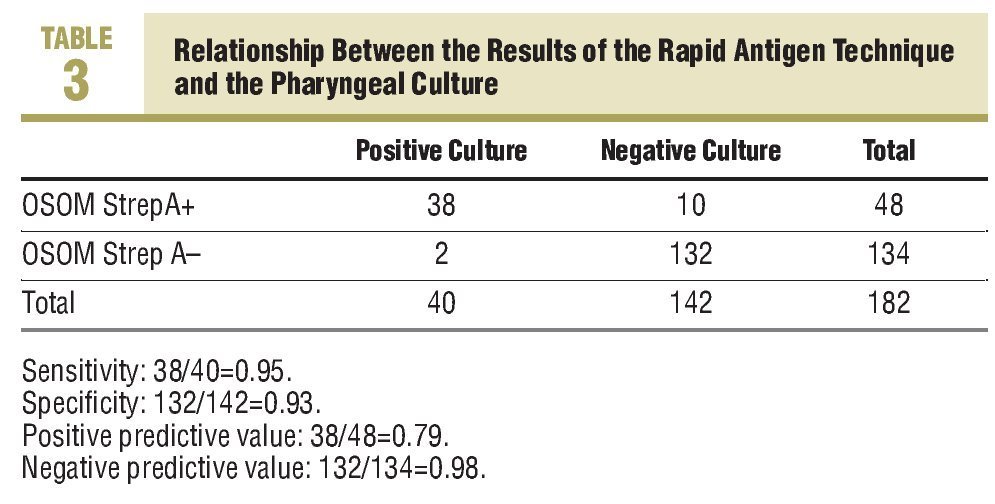
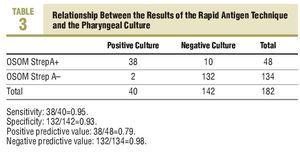
The RAT was positive in 48 cases and negative in the remaining 134 determinations (Table 3). The sensitivity observed with this technique was 0.95 and the specificity, 0.93. There were 10 false positives and 2 false negatives. The positive predictive value was 0.79 and the negative predictive value, 0.98.
Discussion
The sensitivity and specificity achieved (greater than 90%) with the RAT used, along with the high negative predictive value (98.5% in our study), make this test a very helpful diagnostic tool for the family doctor. Before discussing the results we should mention the points where our study differs compared to others. We have included patients with clinical symptoms of pharyngitis with a suspected streptococcal aetiology; that is to say, those with 2 or more of the Centor criteria. Even so, the observed incidence of GABHS was 22%. In other studies published in this journal, the inclusion criteria were wider, and this, without a doubt, is one of the reasons for having found more favourable results in our study.11-13
Only the study by Díaz-Berenguer showed validity values similar to ours, although the positive predictive value of the RAT was somewhat lower in that one, which was due to a lower prevalence of GABHS.12
It would be wrong to compare the results of current RAT with those obtained at the beginning of the 1990´s, since the current RAT kits are more sensitive. Neither can the microbiology study be compared, as, for example, in the study by Díaz-Berenguer, bacitracin disks were used, and also because this method is not used nowadays, as it produced a high rate of false negatives.12
Another of the conclusions of our study, already documented in other studies, is the low reliability of the clinical criteria for the diagnosis of streptococcal pharyngitis.
Even among patients with all the Centor criteria, the probability of having a streptococcal infection was less than 40%. In our study, the presence of any of these criteria makes a streptococcal aetiology more likely, as has been observed in other studies, and of these criteria, the fundamental ones are painful laterocervical lymph nodes and absence of cough.11,12,14 Only these criteria were significantly more prevalent among patients with GABHS infection. On the other hand, no statistically significant differences have been seen with the presence of an exudate or with the presence of a fever. This same data have been observed in other studies. In the study by Lindæk et al, the prevalence of GABHS was even higher among patients who did not have an exudate.14
In a study recently published in this journal by Marin et al,13 it mentioned that the clinical score system obtained a higher negative predictive value and a specificity that allowed nonstreptococcal pharyngitis to be diagnosed with sufficient certainty. However, in our study the probability of infection due to another microorganism other than GABHS was greater than 60% among patients who had 4 criteria and over 70% among those who had 3 criteria. The use of clinical criteria to rule out streptococcal pharyngitis may be useful in developing countries, but in these cases it has been seen that the combination of other criteria, besides the Centor, may be more useful.15 However, in Spain, with the very significant use of antibiotics to treat this infection, it is essential to change habits and use RATs. Only in this way will a reduction in antibiotic prescriptions be achieved, just as was observed in a clinical trial carried out in Canada.16
One aspect of great concern to the doctor who sees a patient with supposedly streptococcal pharyngitis is the reliability of the negative result. In our study, the doctors were free to use antibiotic treatment regardless of the RAT result. The guides indicate that if results are found to be negative, particularly in pharyngitis with all the Centor criteria, they should be confirmed by means of a culture.6 However, this practice is not usually implemented, since the result takes between 24 and 48 hours. In our study, only 2 patients with a negative result (the 2 cases with 3 Centor criteria) actually had a GABHS infection. Also, in another study carried out in Spain, the usefulness of RAT has also been shown, up to the point of considering the culture unnecessary in negative cases.17 Mostov,18 in a recent review, does not recommend it either. A line of research that could be followed in the future is the high observed incidence of infections due to group C beta-haemolytic Streptococcus, 14.3% in our country. The pathogenic role of this bacteria is currently being discussed, since Zwart et al19 observed that penicillin could reduce, although marginally, the duration of the symptoms of pharyngitis due to group C beta-haemolytic Streptococcus. It has virulence factors similar to those of S pyogenes and could cause the same type of infections. It has been associated with outbreaks of pharyngitis with a clinical picture similar to that produced by GABHS, but the non-suppurative after effects are much less common.
In conclusion, we believe that all primary care centres should be provided with RAT for the diagnosis of GABHS infections. RAT is easy to perform, it requires no technical support or specialist staff and is rapid. A RAT determination cost between 2 and 3 euros depending on the different manufacturers, a price that is offset by the cost of a box of amoxicillin, penicillin V, or amoxicillinclavulanic acid. Anyway, this not so much an economic problem than one of health care quality.
Acknowledgement
We would like to thank Laboratorio Leti for its generosity in providing the Genzyme OSOM StrepA strips free of charge, whenever we needed them for the smooth running of this study.
What Is Known About the Subject
• Beta-haemolyticStreptococcusis the cause of 15%-25% of acute pharyngotonsillitis in adults and its incidence increases the more Centor criteria the patient has: tonsillar/pharyngeal exudate, history or presence of fever, absence of cough, and/or presence of painful lateral-cervical lymph nodes.
• The use of clinical criteria to diagnose streptococcal pharyngitis is of no use. Even in patients with all the Centor criteria the incidence of streptococcal pharyngitis is less than 50%.
What This Study Contributes
•The rapid antigen technique is an ideal method for diagnosing pharyngitis due toS pyogenesin the community, since its determination is easy and rapid, and has a sensitivity and specificity of over 90%.
•The high negative predictive value of the rapid antigen technique (with a negative result aetiology due to GABHS is ruled out) means there is no need to carry out a subsequent culture.
•The use of these rapid antigen techniques should be taken considered, particularly in patients with more than 2 Centor criteria.
•The incidence of pharyngitis caused by Group C beta-haemolytic Streptococcus, around 15% in our population, opens an interesting line of investigation, since there is currently no clear consensus on its treatment.
Spanish version available www.elsevier.es/270.210
A commentary follow this article (page. 495)
Correspondence: C. Llor. Foixarda, 95. 43008 Tarragona. España.
E-mail: carles.llor@urv.cat
Manuscript received March 26, 2008.
Accepted for publication April 28, 2008.