Schizophrenia is a complex and multifaceted mental disorder characterized by cognitive, emotional, and behavioral dysfunctions that significantly impact the patients’ daily lives. Premorbid adjustment (PA) is a multidimensional framework, the severity of which has been associated with more severe phenotypic traits and unfavorable outcomes, offering insights into the development of this disorder. This study aims to characterize a group of first-episode schizophrenia (FES) patients based on academic (PAA) and social (PSA) PA, explore the overlap across these dimensions, and examine their associations with early clinical, environmental, and epigenetic factors, through methylation profile scores (MPS).
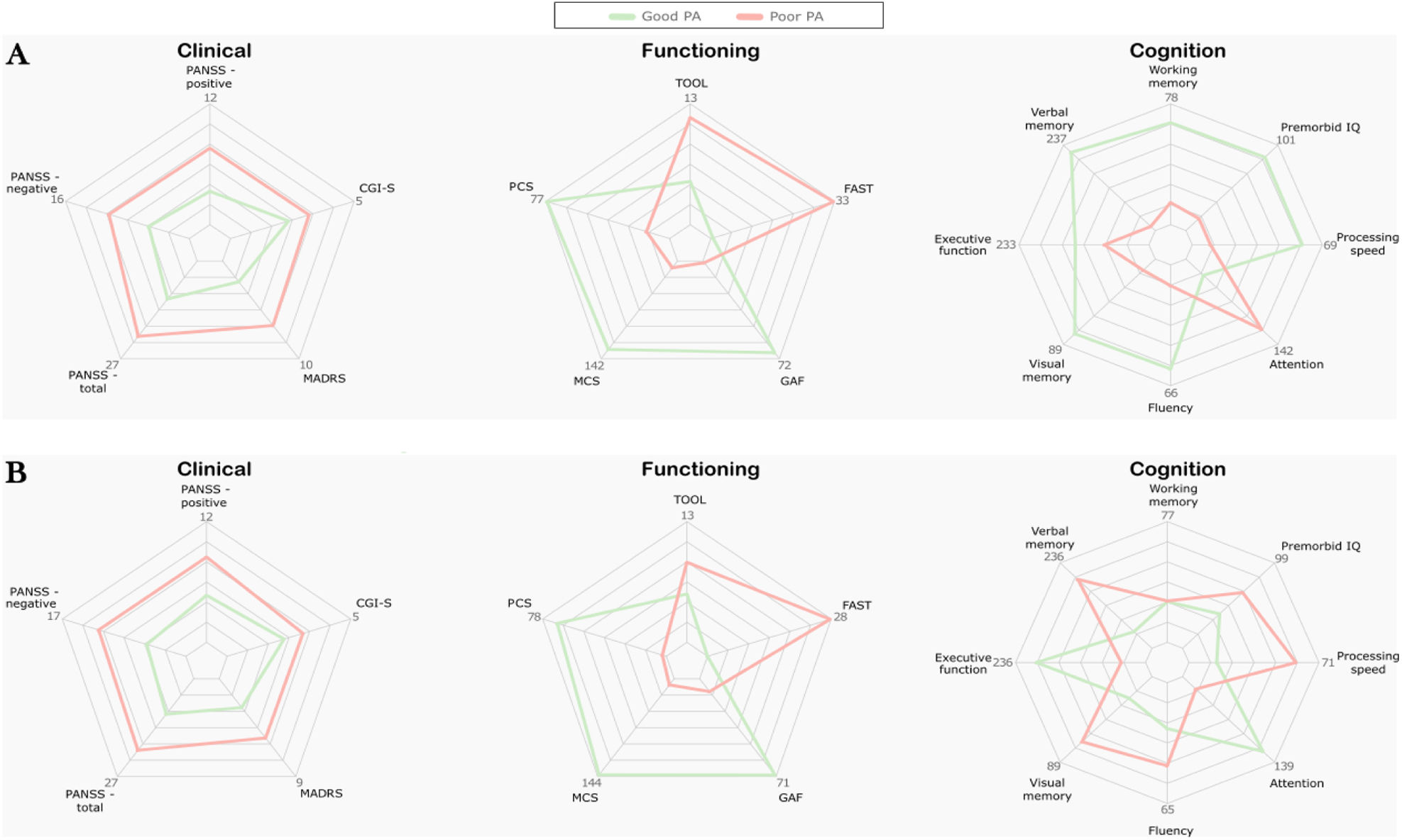
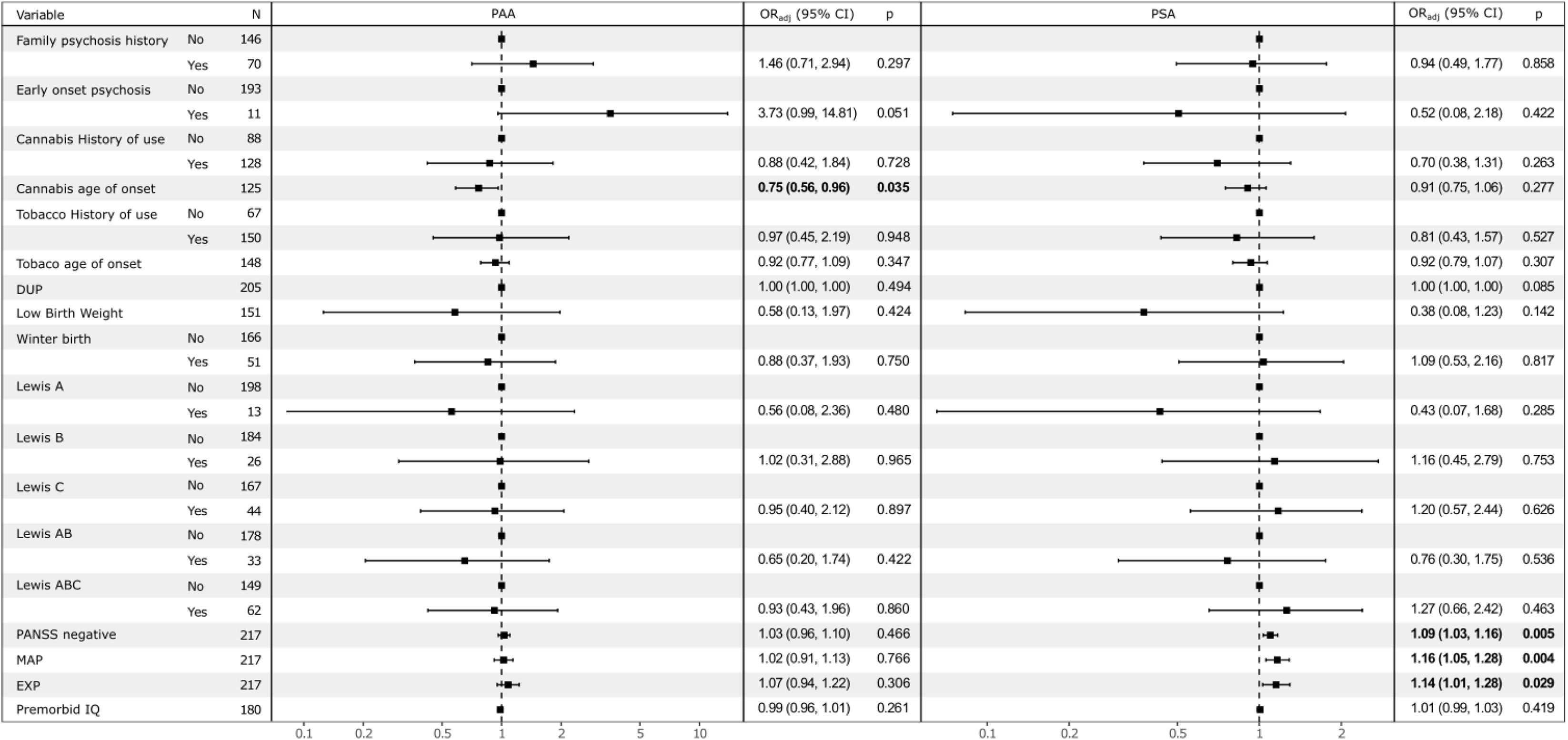
Material and methodsA total of 218 FES subjects were included. K-means clustering identified “poor” and “good” groups for PAA and PSA. Clusters overlaps were explored using multiple correspondence analysis and were characterized by sociodemographic, clinical, functional, and cognitive features. Associations with clinical, environmental factors and MPS were examined using multivariable models adjusted for key covariates.
ResultsPoor-PAA individuals showed worse cognitive performance (working memory, attention, and executive function), lower educational level, and higher cannabis use. Poor-PSA individuals had more severe negative symptoms. MPS for early-life adversity and cannabis use were associated with PSA clusters, while MPS for birth weight and tobacco use were linked to PAA clusters.
ConclusionsPAA and PSA dimensions show distinct clinical, cognitive, functional, and epigenetic profiles. These findings support the use of premorbid functioning subtypes for identifying early markers and tailoring interventions.
Article
(Sociedad Española de Psiquiatría y Salud Mental)
Diríjase al área de socios de la web de la SEPSM, (https://sepsm.org/revista/) y autentifíquese.