A case of a male patient of 19 years 3 months of age is reported. The chief complaint was having discomfort in the jaw. The diagnosis was a hyperdivergent skeletal class III, bilateral molar and canine class III with proclined upper incisors, bilateral anterior and posterior cross-bite, upper and lower crowding with a lower dental midline deviation. The patient also had a maxillary collapse. The patient did not refer any habit. Treatment was conducted in three phases: a pre-surgical phase: alignment, leveling, dental decompensation, tripodism (occlusal stability), transverse expansion. Surgical Phase: Mandibular LeFort I Surgery: 5mm advancement. Post-surgical phase: Detailing, retention. Active treatment time was 4 years 4 months. Removable upper and lower Hawley retainers and fixed canine to canine both in the upper and lower arch were used. Treatment outcome was successful, obtaining bilateral canine and molar Class I, normal overjet and overbite, coincident midlines, adequate intercuspation and a harmonic facial profile.
Se reporta un caso de un paciente masculino de 19 años 3 meses, cuyo motivo de consulta fue «tener molestias en la mandíbula». Es clase III esquelética, hiperdiveregente, clase III molar bilateral, clase III canina bilateral, con los incisivos superiores proclinados, la mordida cruzada anterior y posterior bilateral, tiene apiñamiento superior e inferior, con la línea media dental inferior desviada, presenta colapso maxilar, el tercer molar inferior izquiero en formación, el paciente no refiere ningún hábito. El tratamiento se realizó en tres fases, fase prequirúrgica: alineación, nivelación, descompensación dental, tripodismo (estabilidad oclusal), expansión transversal. Fase quirúrgica: cirugía mandibular Le Fort I: avance: 5mm, Fase postquirúrgica: detallado y retención. Tiempo de tratamiento activo 4 años 4 meses. Se utilizaron retenedores removibles Hawley superior e inferior y fijos de caninos a caninos tanto en superior como en inferior. El resultado del tratamiento fue exitoso, con la obtención de clases I caninas y molares bilaterales, sobremordida horizontal y vertical adecuadas, lineas medias coincidentes, correcta intercuspidación y un perfil facial armónico. Tiempo de 4 años y 4 meses.
Approximately 4% of the population has a dentofacial deformity that requires orthodontic – surgical treatment to correct it. The most common indications for surgical treatment are severe skeletal class II and III malocclusions and vertical skeletal discrepancies in patients who are no longer in a growth period.1 Skeletal class III patients represent a large proportion of those who are seeking surgical-orthodontic treatment. Proffit et al.2 reported that from patients with orthodontic-surgical treatment, 20% have a mandibular excess, 17% have maxillary deficiencies and 10% have both. Skeletal class III patients are more likely to seek clinical evaluation than skeletal class II patients.3 The majority of people with class III malocclusions have dentoalveolar and skeletal problems and only the minority of cases could be treated only with orthodontics. Patients with severe class III skeletal discrepancies are often treated with maxillary, mandibular or bimaxillary orthognathic surgery in combination with orthodontic treatment.4 Few studies have examined the factors that influence the decision between conventional orthodontic treatment and orthodontic-surgical treatment. Kerr et al reported that patients with ANB angles of less than -4° and mandibular incisors with inclinations of less than 83° are more likely to undergo orthodontic-surgical treatment.5
A more recent study concluded that surgical patients could be distinguished from the non-surgical ones based on the Wits appraisal measurements, the maxillo/mandibular length ratio, the gonial angle and the distance sella-nasion.6 On the other hand, circumpuberal growth is complete, or almost complete, in patients with ages between 15 years for girls and 17 years for boys. Although some mandibular growth can occur up to 20 years of age, an investigation of more than 300 orthodontists reported that the earliest ages to start the orthognathic surgery treatment were 14.9 years for girls and 16.5 years for boys.7,8 Treatment for an adult patient with a skeletal class III malocclusion requires dentoalveolar decompensation and combined procedures of orthodontics and surgery with the aim of achieving a normal occlusion and improve facial aesthetics.9–12 One of the main objectives of the pre-surgical orthodontics phase is correcting the incisors inclinations to normal or to place them within the alveolar bone in order to allow maximum surgical correction.13,14 The main objectives of the orthodontic-surgical treatment are: to normalise the facial profile, to correct within a range of normal values the main dento-skeletal parameters and to achieve a proper occlusion and function.15 When planning a conventional treatment with orthognathic surgery, the anteroposterior discrepancies are corrected through the advancement or retroposition of the jaws along the existing occlusal plane. When a vertical change of the maxilla is required, the mandible will self-rotate; forwards and upwards; as a consequence of this rotation, the mandibular plane angle will be altered. When a change of the occlusal plane is required for aesthetic considerations, the maxilla and the mandible should rotate together according to the newly defined occlusal plane.16 Reykene et al, established that when a patient needs a change of the occlusal plane of more than 2°, the situation is significant enough to be considered as a case of intentional rotation, in a clockwise or counter-clockwise direction. This treatment design is also known as a modification of the occlusal plane or rotation of the maxillomandibular complex and is often indicated in patients who have a severely low (hypodivergent) or high (hyperdivergent) mandibular plane angle.16 The clockwise rotation of the maxillomandibular complex is used in the case of patients with a hypodivergent growth pattern. It provides good maxillary incisor exposure, an excellent arch curvature during smile and improves the patient's facial balance.17
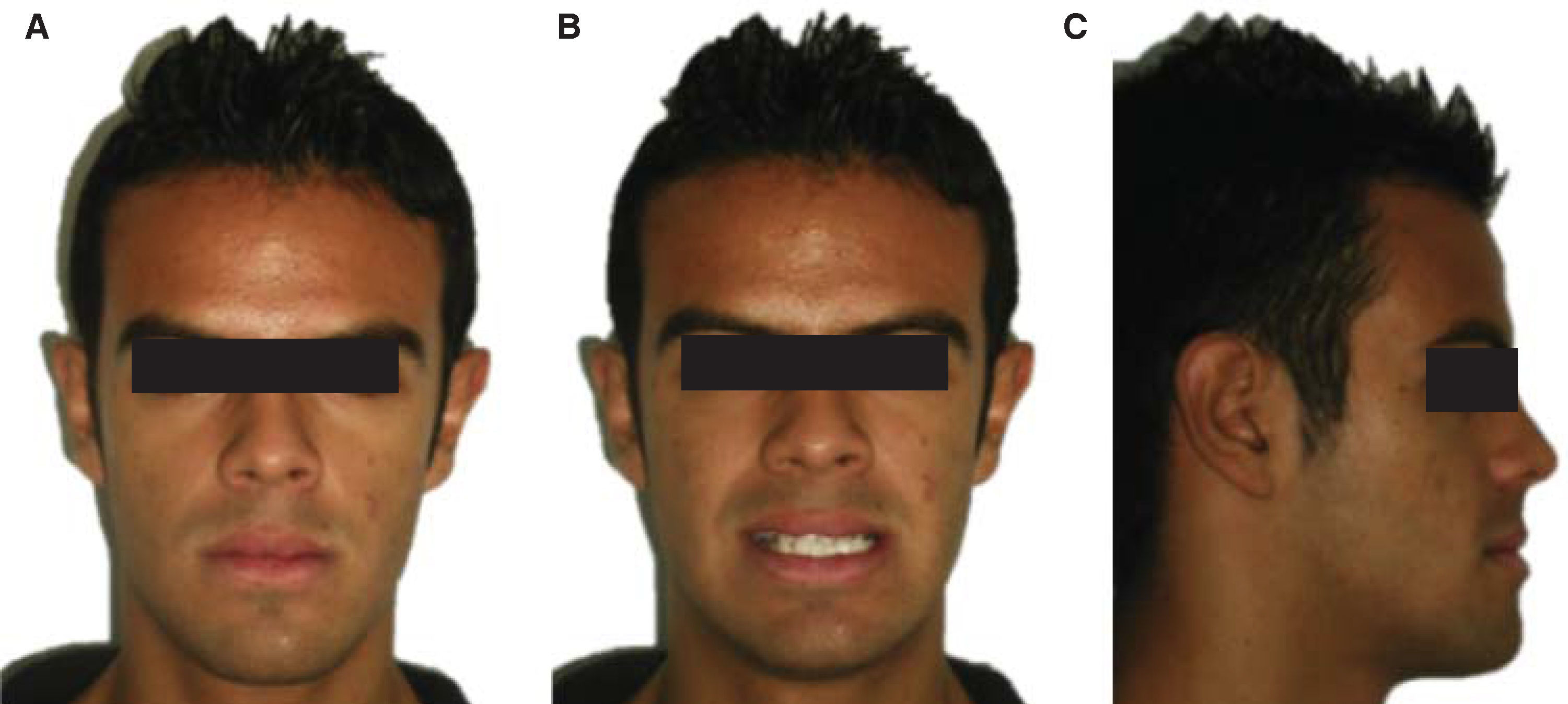
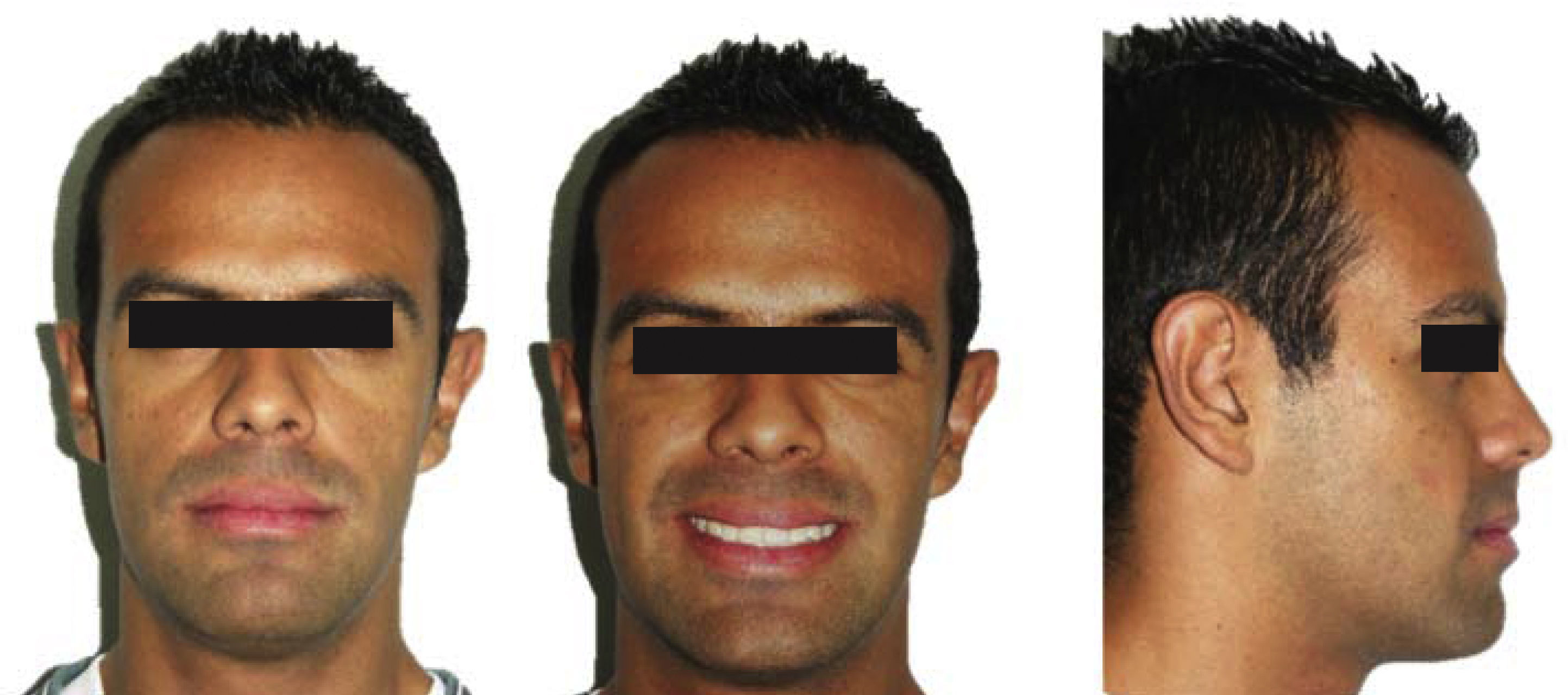
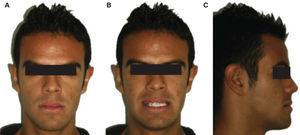
MATERIAL AND METHODSMale patient, 19 years and 3 months of age, whose chief complaint was «discomfort in the jaw». The patient did not report to have any habit. Upon facial clinical examination, in the frontal photograph (Figure 1A) he was diagnosed as a brachifacial patient. In the smile photograph, a 2mm lower dental midline deviation to the left was observed (Figure 1B). The profile photograph shows a hyperdivergent growth pattern and a slightly concave profile (Figure 1C).
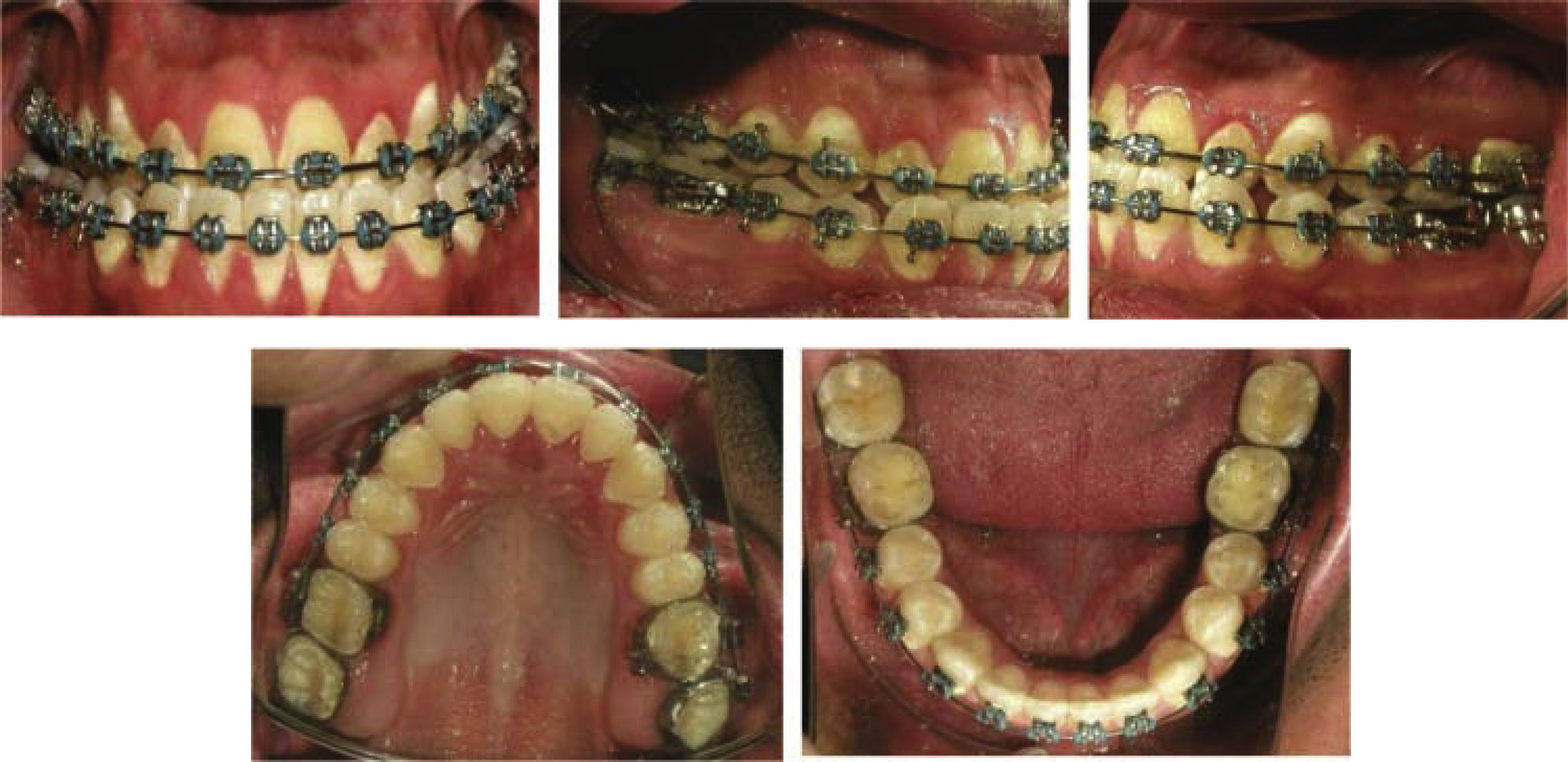
In the initial intraoral assessment, a 2mm deviation to the left of the lower dental midline was observed, as well as anterior cross bite, 4mm of negative overjet and overbite reversed in 40% and also dental fluorosis. In the intraoral lateral photographs a bilateral canine and molar class III was observed, anterior and posterior crossbite. In the upper ocw sal pothograph maxillary hypoplastia and oval arch were observed. In the lower arch, a light anterior crowding was observed (Figure 2).
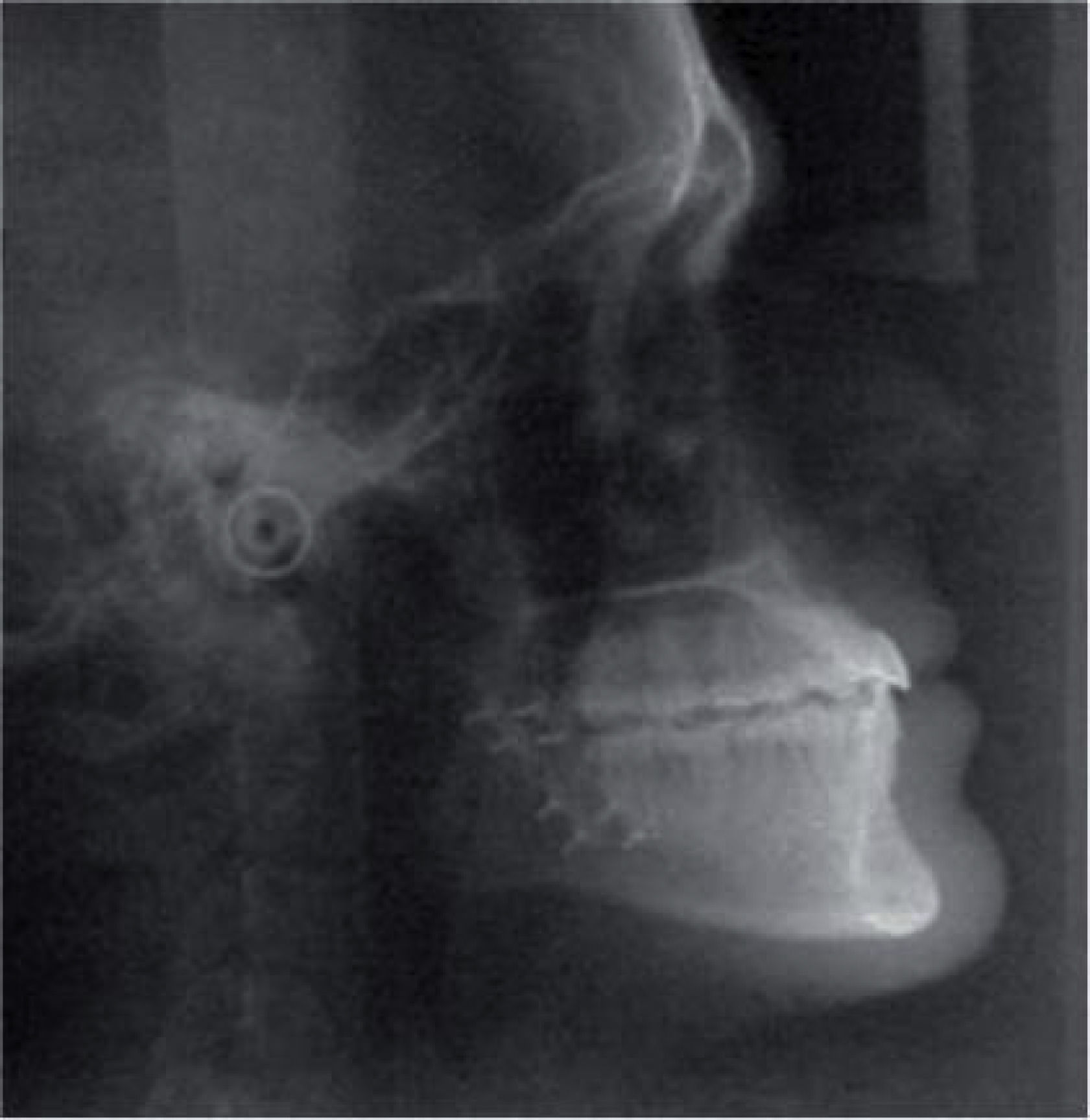
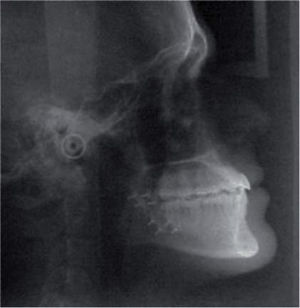
In the initial lateral headfilm, the skeletal class III, the hyperdivergent growth pattern and the upper and lower incisor inclinations are observed (Figure 3).
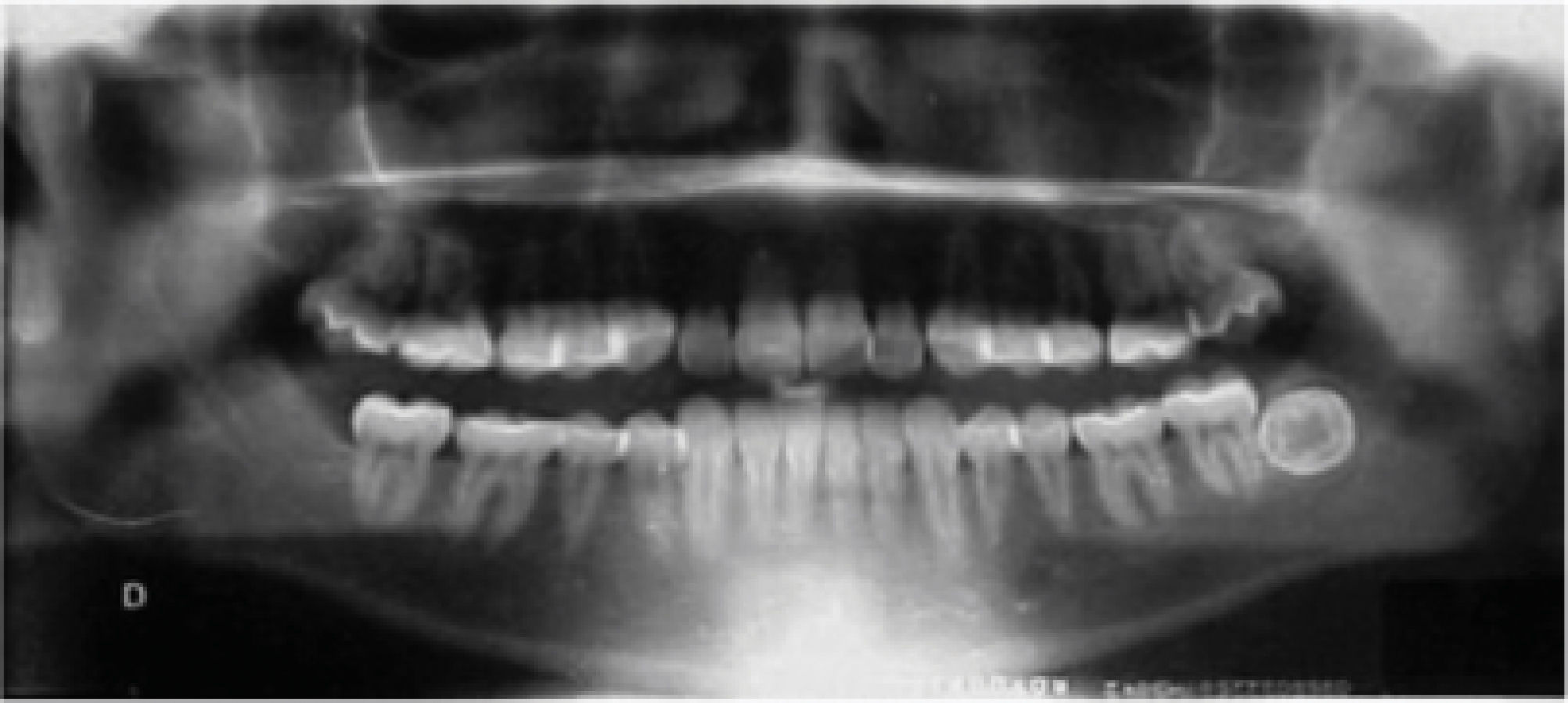
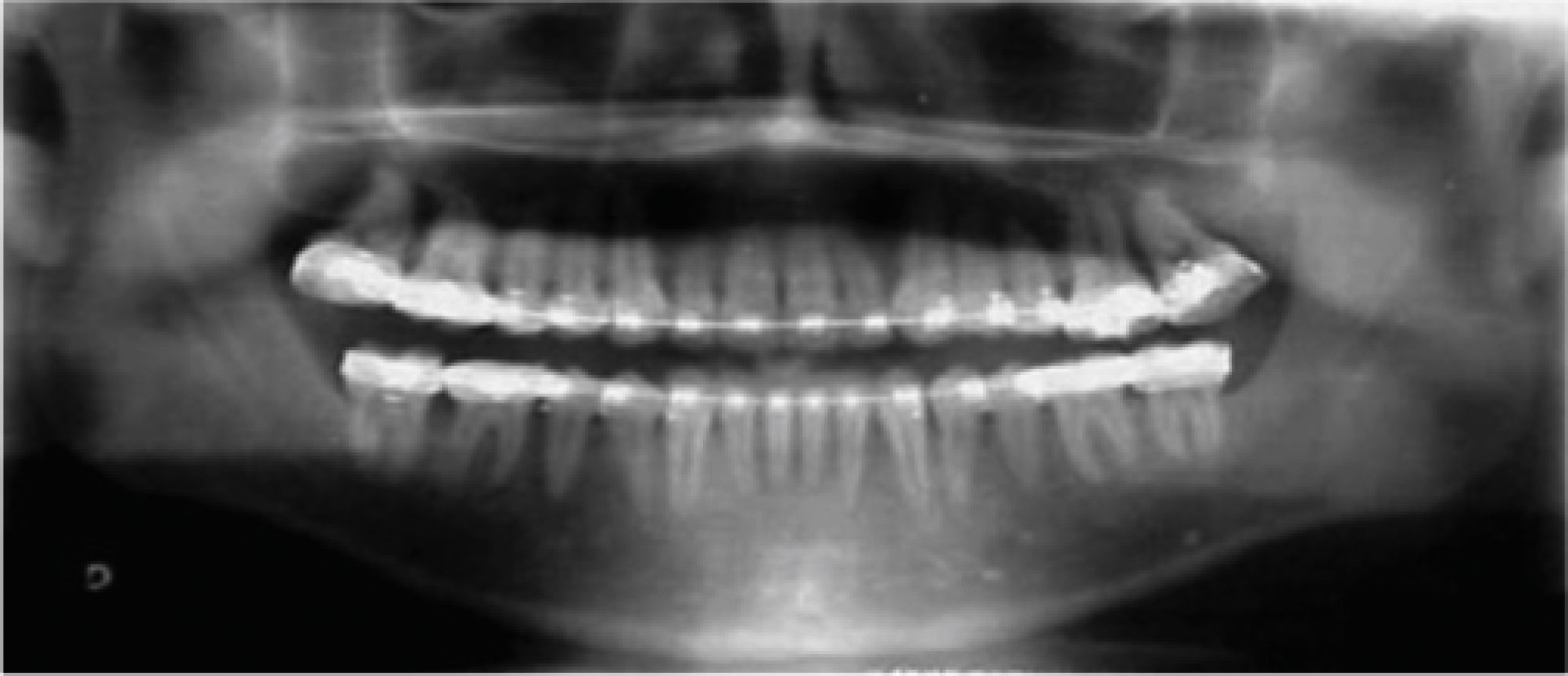
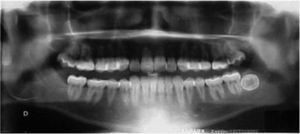
In the initial panoramic radiograph 29 teeth are observed, among them, the lower left third molar and an adequate crown-root ratio as well (Figure 4).
The treatment objectives were: to correct the skeletal relationship, the maxillary hypoplasia, the facial profile, the transverse maxillary collapse, the mild mandibular crowding and the deviated lower dental midline; to achieve tripodism (occlusal stability), to obtain molar and canine bilateral class I, to correct the anterior and posterior bilateral crossbite, to obtain an adequate overbite and overjet, as well as to achieve maximum intercuspation, with canine and incisor dysocclusion guidance and improve periodontal health.
The treatment plan was carried out in the CESO and was conducted in three phases. In the pre-surgical phase, alignment and levelling were performed (dental decompensation), obtaining tripodism (occlusal stability) and maxillary lateral expansion, through brackets Roth 0.022” x 0.028” prescription, 2 mm- length surgical hooks and 0.022” x 0.028” bands in first and second molars. The surgical phase consisted in maxillary surgery (Le Fort I osteotomy with 5mm advancement). In the post-surgical phase, detailing was performed and for retention, upper and lower Hawley plates were placed.
In the patient's facial assessment of treatment progress, performed 3 years after the beginning of treatment, the lower dental midline presented a 3mm deflection to the left with regard to the facial midline, the hyperdivergent growth pattern and the slightly concave profile were maintained (Figure 5).
In the intraoral assessment of treatment progress, the 3mm deviation of the lower dental midline to the left remains, the patient presents a -4mm overjet and an improvement in the overbite, which is still decreased. The right and left side intraoral photographs confirm the bilateral canine class III and molar class III. In the upper occlusal photograph an oval arch form is observed and the transverse maxillary expansion (Figure 6). In the lower occlusal photograph, the oval shape of the lower dental arch is noted as well as the correction of the mild crowding.
In the treatment progress lateral headfilm, a decrease in the upper and lower incisors retroclination may be observed due to the leveling and dental decompensation thus placing the upper and lower incisors centered in their basal bone (Figure 7).
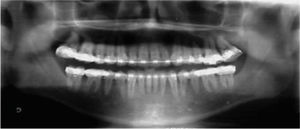
In the panoramic radiograph, bone remodeling is noticeable in the extraction site of the lower left third molar. Also, it may be observed that the crown-root ratio has been maintained (Figure 8).
RESULTSThree years after treatment started, the objectives stated at the beginning of treatment were achieved. The facial examination revealed that the skeletal relationship was corrected as well was the maxillary hypoplasia thanks to the Le Fort I osteotomy for maxillary advancement; the mandible experienced self-rotation in a forward and upward manner. A balanced face and an adequate profile were obtained with a wide smile and buccal corridors (Figure 9).
In the final intraoral assessment, an adequate overjet and overbite, alignment and leveling were obtained. Intraoral lateral photographs revealed a bilateral molar and canine class I, correction of the bilateral posterior cross-bite and maximum intercuspation (Figure 10).
Orthodontic-surgical treatment provided the patient with an appropriate facial profile by maxillary impaction and advancement, a reduction genioplasty of the chin and the correction of the left dentoalveolar asymmetry. The anterior and posterior crossbite were corrected, bilateral canine and molar class I were obtained and aligned dental midlines. Root parallelism was achieved as was also a canine and incisal guidance. An adequate maxillary incisor display at smile and a facial good balance were obtained (Figure 11). The patient responded well physiologically and psychologically and was very satisfied with the treatment results.
For retention and treatment stability as well as maintaining inter-canine width, fixed retainers were placed in the upper and lower arch (Figure 12).
In the final cephalogram it may be observed a skeletal class I relationship with a 0° ANB angle, hyperdivergency and normal inclinations of the upper and lower incisors (Figure 13).
In the final panoramic radiograph, evidence of the orthognathic surgery may be observed and the 28 dental organs with a good root parallelism (Figure 14).
DISCUSSIONAuthors such as Bailey and Johnston mentioned that historically, skeletal class III malocclusions have been treated only with mandibular retrusion, however, several recent studies indicate that bimaxillary surgical procedures have become more frequent.14–18 Kwon recognizes that skeletal class III malocclusions are often combined with a vertical discrepancy. The nature of the anomaly provides instructions for performing the surgical repositioning in order to achieve facial harmony. It has been reported that vertical changes may affect the amount of mandibular relapse.18,19 Bothur and Proffit et al, mentioned that there are numerous studies on post-sugical stability in the literature.20,21 Jakobsone, Moldez, Costa and Proffit stated that several studies have established that stability has been maintained after vertical changes in the position of the maxilla.22–25 Phillips, Johnston and Tompach reported that orthodontic–surgical treatment in skeletal class III patients involves a pre-surgical orthodontic phase with decompensation of the dental malocclusion followed by a surgical phase where the required surgical procedures are performed and subsequently, the orthodontic post-surgical phase that includes orthodontic finishing and detailing.
The typical dental decompensation consists in retraction or retroclination of the proclined maxillary incisors and proclination of the retroclined mandibular incisors into a more normal axial inclination. This increases the severity of the dental class III malocclusion and often results in a less aesthetic facial profile prior to surgery.13,14,26 Pre-surgical dental decompensation determines the magnitude of the surgical changes and is the main factor in treatment success. The absence of an optimal dental decompensation compromises the quality and quantity of the orthodontic correction.26,27 Proffit, in 1987 reported that within the hierarchy of stability of orthognathic surgery procedures impaction is the more stable maxillary procedure and its retention with rigid internal fixation or with wire has no influence on the stability of the impaction.27 On the other hand, our results coincide with Reyneke and Chemello, who established that, in patients treated with surgical impaction with Le Fort I osteotomy, in addition to the rotation of the maxillomandibular complex, conventional orthodontic treatment produced a stable occlusion and adequate skeletal relations, with good long-term stability.16,28 Proffit mentions with regard to the time scale of post-surgical changes that the majority of changes, both skeletal and dentoalveolar, occur within the first six months after surgery29 as they were seen in the case hereby reported. It is of the utmost importance that orthodontic appliances remain placed in the mouth in patients who have had dental decompensation during some months after orthognathic surgery to achieve stability of the skeletal and dentoalveolar structures and a completely harmonic result.
CONCLUSIONSIn clinical practice, the choice between several surgical procedures is based on clinical examination and cephalometric evaluation. One of the main concerns of both orthodontists and maxillofacial surgeons in the diagnosis and treatment planning of surgical patients is the final aesthetic appearance of the soft tissue profile. In order to achieve an optimal post-surgical profile, the balance of the soft tissue contours and the anteroposterior relative positions of the nose, lips and chin should be assessed.
Despite the fact that most of the skeletal relapse occurs during the first six months after surgery the patient showed skeletal stability. He was benefited from the stability gained by the maxillary advancement and impaction and from the dental decompensation which contributed to occlusal stability. This fact highlights the importance of the post-surgical orthodontic phase including detailing and retention.
This case report shows that the counter-clockwise rotation of the maxillomandibular complex may be satisfactory in patients with a skeletal class III malocclusion, facial asymmetry and hyperdivergent growth pattern.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia
Second-year resident of the Masters Program of Orthodontics and Maxilofacial Orthopedics at the Center of Higher Studies of Orthodontics (CESO).