Class III malocclusion is a growth alteration of the maxilla and mandible. According to some studies it can be present in 4% (of us citizens) to 50% in Japanese and Korean populations. Its main feature is the anteroposterior growth of the mandible, accompanied by its dental organs, giving a clear Angle’s class III occlusion with a negative overjet. This anomaly shows an evident cosmetic defect due to fact that a prominent jaw gives a sunk and blurred appearance of the facial middle third, giving anadust expression to the face, sometimes accompanied by depression. This article reports the results of an orthognathic surgery (oblique ramus osteotomy) on a 21-year-old female patient that presented a class III malocclusion caused by an increase in mandibular growth, who came to the Orthodontics Specialty Clinic at UNAM FES Iztacala and presented a concave profile, skeletal class III, skeletal maxillary biprotrusion, prognathism, Angle’s class III malocclusion and anterior and posterior crossbite. The purposes of the reduction of prognathism by a ramus oblique osteotomy (subsigmoid) with an extra oral approach were: to improve her profile and skeletal and dental alignment; to obtain an adequate overbite; to maintain the dental midline; to achieve left and right molar class I; and obtain left and right canine class I. After nearly two years of treatment, the results were very satisfying, as can be seen in this report.
La maloclusión clase III es una alteración de crecimiento del maxilar y mandíbula. De acuerdo con algunos estudios ésta puede presentarse en un 4% (estadounidenses), hasta un 50% en poblaciones japonesas y coreanas. Su característica principal es el aumento del tamaño mandibular en sentido anteroposterior, acompañado de los órganos dentarios, dando una clara oclusión clase III de Angle con un overjet negativo. Esta anomalía trae consigo un defecto estético muy evidente, ya que la mandíbula prominente da la apariencia del tercio medio de la cara hundido y desdibujado da una expresión de cara dura, acompañada en algunas ocasiones de depresión. En este artículo se reportan los resultados de una cirugía ortognática (osteotomía oblicua de la rama), en la apariencia de una paciente que presentaba maloclusión clase III por aumento de crecimiento mandibular, la cual acudió a la Clínica de Especialización en Ortodoncia perteneciente a la FES Iztacala UNAM, de sexo femenino, de 21 años de edad que presentaba perfil cóncavo, clase III esqueletal, biprotrusión maxilar esqueletal, prognatismo, maloclusión clase III de Angle, mordida cruzada anterior y posterior. El propósito del tratamiento fue mejorar el perfil y alineación esqueletal y dental ideal para obtener una buena sobremordida, mantener la línea media dental, lograr la clase I molar derecha e izquierda y obtener la clase I canina derecha e izquierda por medio de una reducción del prognatismo, mediante una osteotomía oblicua de la rama (subsigmoidea) por medio de un abordaje extra bucal. Después de casi dos años de tratamiento los resultados son muy satisfactorios, como se puede apreciar en este reporte.
The attractiveness of a smile has been considered a standard of satisfaction at the end of an orthodontic treatment for both the specialist and the patient. Therefore it is important to assess the patient’s smile and profile at the initial diagnosis where we can identify all the characteristics of the structures that can be affected thus providing a facial disharmony.
Prognathism is one of the most frequent anomalies that causes facial disharmony. It is considered amaxillary growth anomaly and its main characteristics the increased size of the mandibular corpus, the ramus, or both, mainly in an anteroposterior direction, that makes the mandible appear obviously thrown forward and downward. The lower dental organs follow this growth giving a full Angle’s class III malocclusion with a negative overjet.
This anomaly shows a very obvious cosmetic defect due to the fact that a prominent mandible gives the facial middle third a sunka and faded appearance, thereby giving the impression of anadust and aggressive face, which is reinforced by a sad look in the eyes. Sometimes, when there is a severe prognathism, the patient may present lip incompetence which makes lip contact at rest virtually impossible. This may condition the patient to mouth-breathing, because air enters more easily through open lips than the nose, especially while sleeping. Also, the lower lip is contracted when the patient tries to close, affecting the mandible and the chin muscles, and changing even more the patient’s profile, because it moves the chin over the mentolabial fold. The protruded mandibular position allows a more comfortable and forward position of the tongue that simulates, most of the times, a non existant macroglossia. Studies on individuals with class III malocclusion have established that between 42 to 63% of patients with skeletal class III maloclussion have a retrusive maxilla or a combination of a retruded maxilla and normal or average mandible.1–8
These cases can be successfully treated with major changes in the facial profile harmony through orthognathic surgery. Robinson (1956) and Hinds (1957) suggested performing the osteotomy in an oblique angle toward the maxilla beginning slightly behind the deepest part of the sigmoid notch and finishing behind the angle. This procedure is called oblique ramus osteotomy.7,9–12
In this case report we will be able to observe significant changes on the patient’s profile appearance that occur when performing an orthognathic surgery.
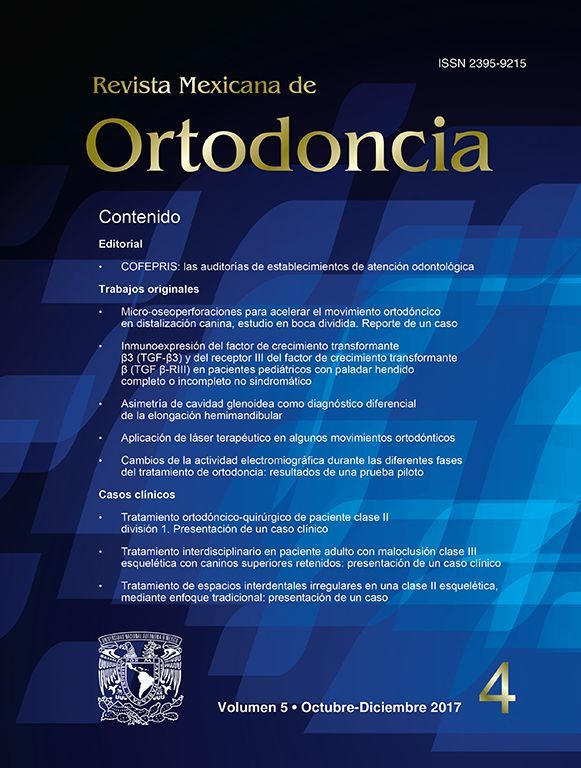
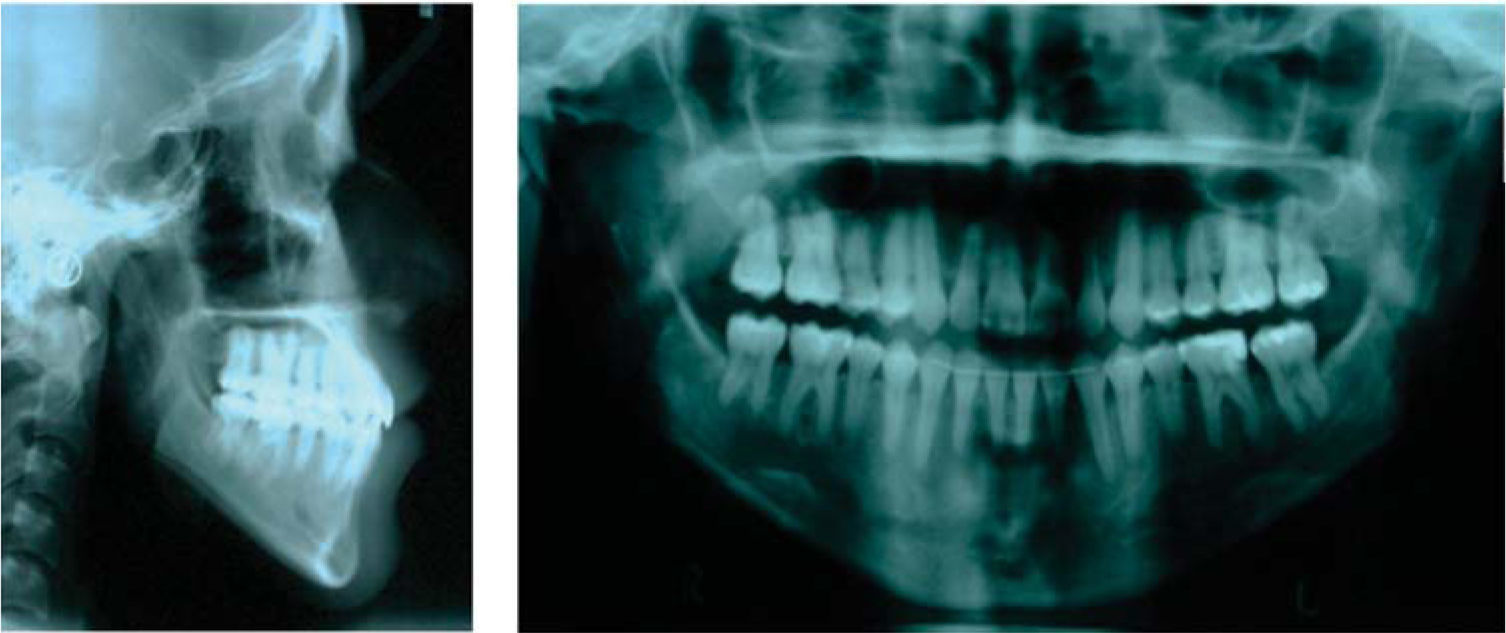
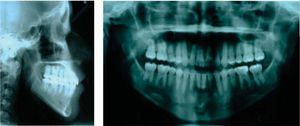
Diagnosis and etiology21-years-old Mexican female patient who, according to the analized photographs, models and panoramic radiographs, presents a concave profile; skeletal class III due to an advanced position of the mandible; right posterior crossbite and anterior crossbite; brachifacial biotype; vertical growth tendency; Angle’s class III; retroclined and retrusive upper incisors; retroclined and retrusive lower incisors; a -3.5mm upper arch discrepancy; 5mm overbite; and -5.5mm overjet.
The clinical chart does not reveal any contraindication for receiving a pre-surgical and subsequently surgical treatment.
After the photographic and radiographic analysis, it is determined that the best solution for her facial appearance is an oblique ramus osteotomy (Figures 1 to 3).
Treatment goals- •
To achieve a harmonic profile by reducing the mandibular protrusion.
- •
To improve the occlusion.
- •
To correct the anterior crossbite and right posterior crossbite by obtaining an adecuate overbite and overjet.
- •
To achieve molar class I.
- •
To keep the midlines aligned.
The treatment plan was based on the implementation of orthodontics pre-surgical procedures, where Roth .018 fixed appliances were placed with tubes in first and second molars, to achieve alignment and leveling of the case. Subsequently, the surgery was performed (oblique ramus osteotomy), followed by post-surgical orthodontics for third order movements and at the end, retention is placed.10,13–16
Treatment progressTreatment began by placing .016 upper and lower NiTi arches with elastic modules to achieve dental alignment. By August the arches were changed by ones of the same caliber, but in stainless steel, in order to avoid pronunciation of the curve of Spee. To continue with the alignment interproximal stripping was made from dental organs # 32 to # 42 and an open coil was placed between 32 and 33 (Figure 4).
During September and October.018 NiTi upper and lower arches were used with elastic modules and slight stripping was performed between dental organs # 33 and # 32. The stainless steel arches were changed for a .018 in the second half of October.
In November it was decided to place.016×.016 of NiTi arches for fifteen days; at the end the arches were changed by .016×.022 NiTi rectangular arches during November and December. In January the arches were changed by others of the same caliber, but in stainless steel.
At this stage a good dental alignment had already been achieved, but there were interproximal spaces between canines and premolars. Impressions were taken to determine if it was possible to perform the surgery; the study models revealed premature contact points in the upper molars, so a .016×.022 Blue Elgiloy archwire with intrusion loops was placed. These arches remained during January, February and part of March.
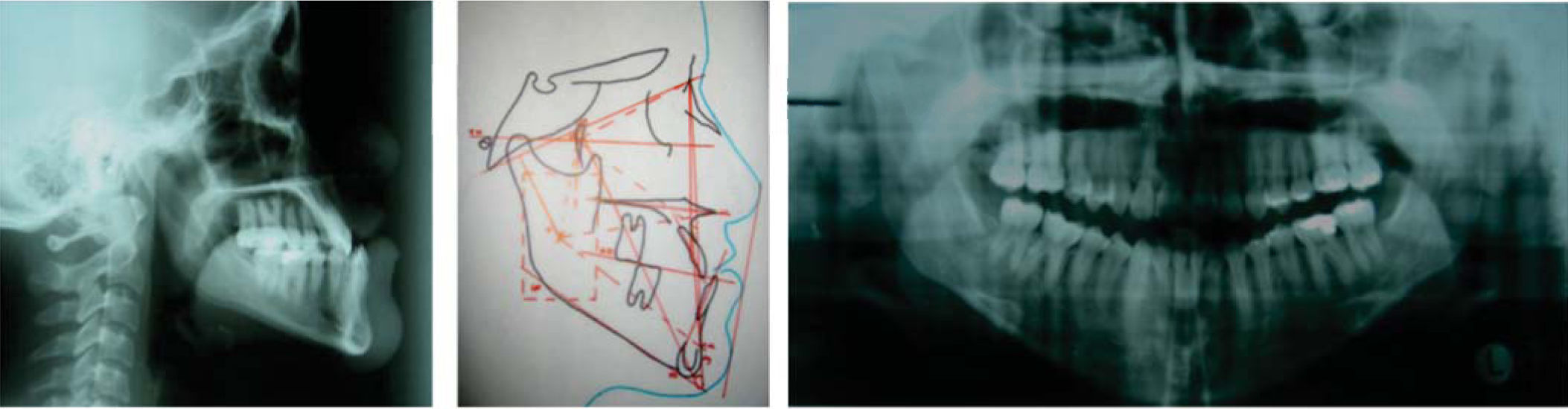
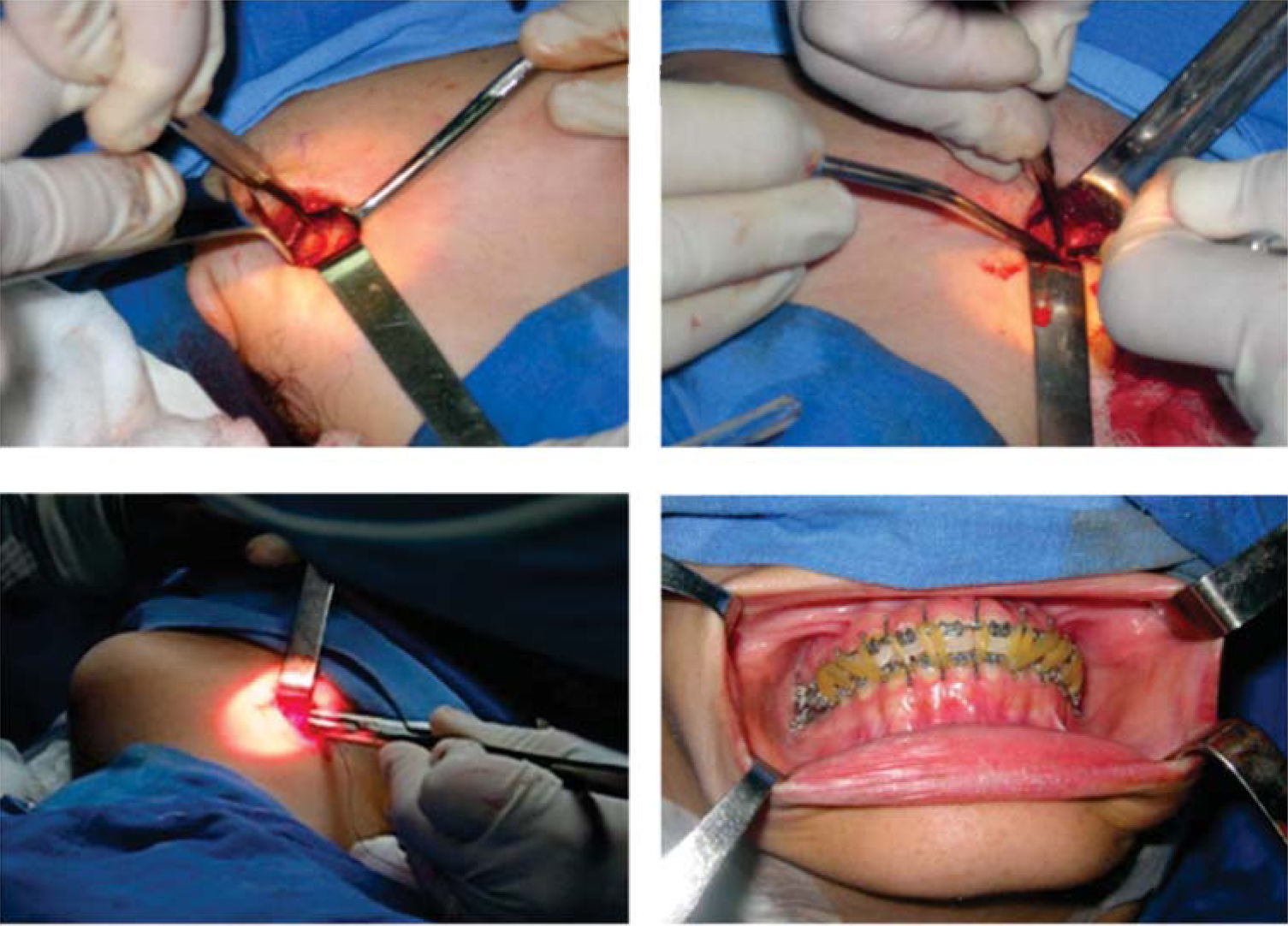
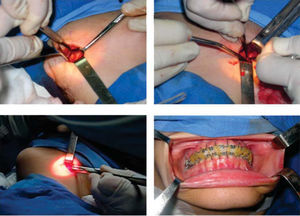
In March of 2004 once the goals of the previous stages had been achieved, .017×.025 stainless steel archwires with surgical hooks were placed(Figure 5). At this moment, study models and radiographs were sent with the Maxillofacial Surgeon, José Luis Chain Anguiano to plan the surgery, which was performed successfully on March 31 2005 at «La Raza» Medical Center (Figures 6and7).
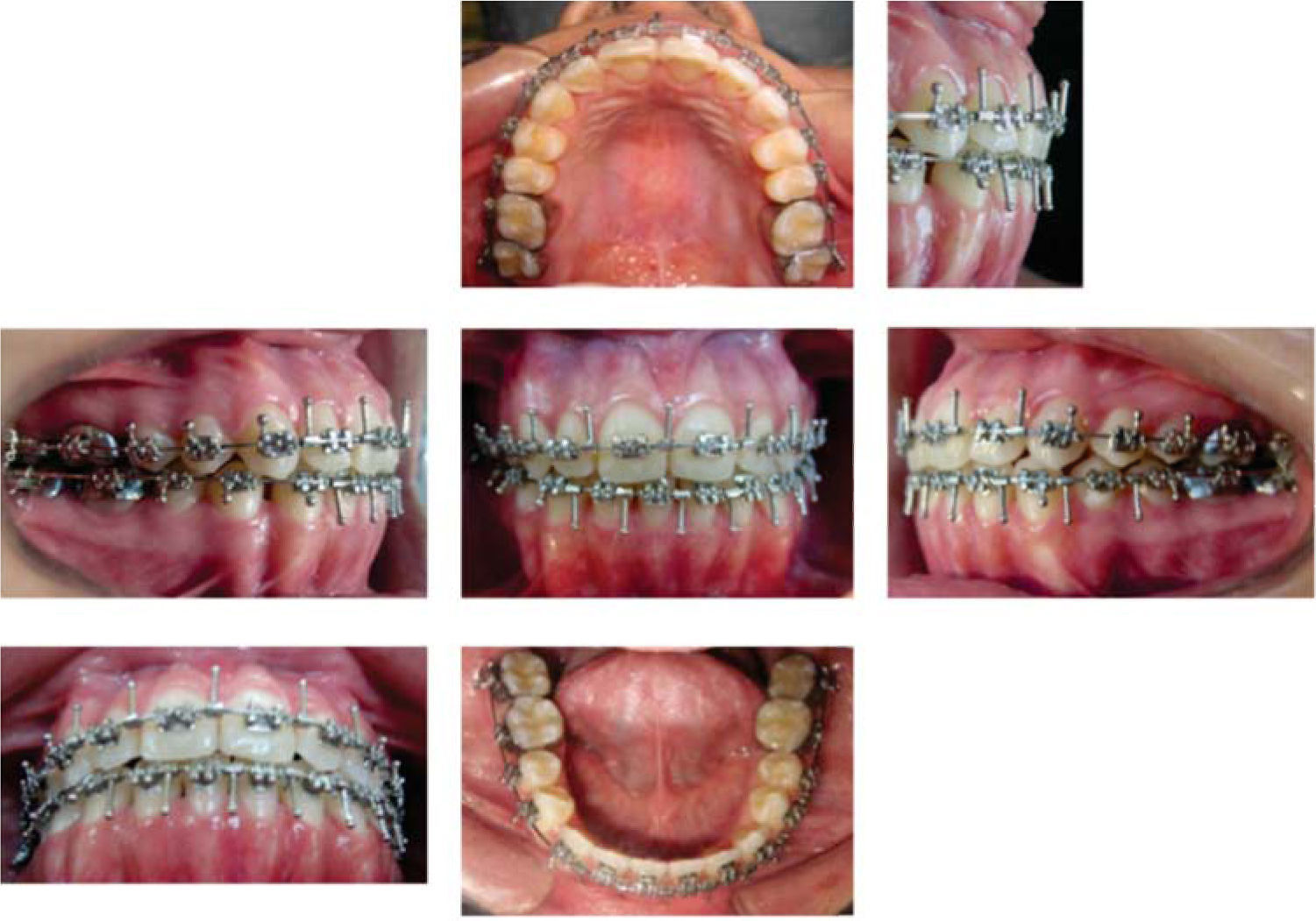
During the following two months after the surgery the patient remained with intermaxillary fixation with intraoral elastics, that is why on June 2, 2005 orthodontic movements were resumed. By indication of the above mentioned specialist, the surgical hooks archwires were withdrawn and .017×.022 NiTi arches were placed. Treatment continued with these arches but with zigzag intermaxillary elastics in the posterior segment and anterior cross elastics until August. Brackets were repositioned for detailing and root alignment. The archwires were changed for .016×.016, with right class III elastics and class II on the left and anterior cross elastics from tooth 12 to 32. At the end of the treatment, which lasted 18 months, photographs, models, and panoramic and lateral head films were taken to compare the initial values with the finals and observe any significant change (Figures 8 to 10).
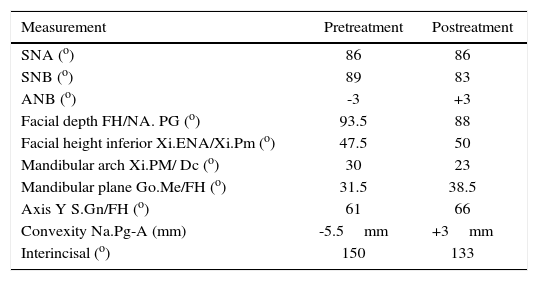
Treatment resultsFacial harmony, a charming smile and a proper occlusion were achieved. A correct class I molar relationship, an adequate overbite and overjet and significantchangessuch asan ANBincrease that went from -3o to 3o thus achieving a class I skeletal were also obtained. The patient was fully satisfied with the treatment results (Table I).
Cephalometric measurements before and after treatment.
| Measurement | Pretreatment | Postreatment |
|---|---|---|
| SNA (o) | 86 | 86 |
| SNB (o) | 89 | 83 |
| ANB (o) | -3 | +3 |
| Facial depth FH/NA. PG (o) | 93.5 | 88 |
| Facial height inferior Xi.ENA/Xi.Pm (o) | 47.5 | 50 |
| Mandibular arch Xi.PM/ Dc (o) | 30 | 23 |
| Mandibular plane Go.Me/FH (o) | 31.5 | 38.5 |
| Axis Y S.Gn/FH (o) | 61 | 66 |
| Convexity Na.Pg-A (mm) | -5.5mm | +3mm |
| Interincisal (o) | 150 | 133 |
On this treatment, it is important to clarify that in the oblique ramus osteotomy (subsigmoid) the extraoral approach and the intermaxillary fixation with elastics (orthodontic appliances) were chosen due to the type of growth that the patient had and to the obtuse goniac angles that she presented. However Mc. Carthy in his book «Plastic surgery- the face» refers to the use of this surgical technique because of its main advantage which is the ease of implementation as it provides better visibility for identifying the outer surface of the ramus and the sigmoid notch. Another advantage when performing the osteotomy is to avoid any injury to the lower alveolar nerve due to the fact that the osteotomy is performed quite far from the mandibular foramen. The author mentions that through continuous traction of the external pterygoid muscles and the internal pterygoid insertions that favor the adduction of the condyle and its propensity to be in the glenoid fossa, it is not necessary to use the interosseous wiring only intermaxillary fixation.1,10–12,17
In the surgical evolution, the scars are very faint and mandibular stability is present. Radiographically, remodeling and bone formation in the mandibular ramus is observed.
ConclusionsThe psychological change that occurs with these patients, especially in women, when they see the improvement in their profile, their smile and masticatory functionis very important. We must not forget that the first thing that patients present is their face and then the teeth, so the face is a letter of introduction to the society, that each day is more competitive and demanding.
The characteristics of a case that has a dentofacial disharmony and requires orthognathic surgery would be: make a good patients election, a thorough medical history, a complete clinical evaluation through cephalometric studies, photographs, and study models mounted in articulator in order to establish an individual diagnosis for that patient as well as the best treatment plan; a good surgical orthodontic treatment with ideal appliance placement so that once it is time for surgery, the patient continues with periodic reviews and as soon as a problem is identified an immediate solution might be applied.1,14,15
It is a moral and ethical obligation to allow the patient to take important decisions about the therapy that will be accepted and currently there is also a legal obligation. Orthodontic treatment and orthognathic surgery are elective treatments. Regardless of whether the doctor may think that a particular treatment is very convenient, currently, patients must have sufficient available information to make their own decisions.