The disabled population has increased worldwide, which has resulted in them being more included and equal in society. Orthodontic treatment is possible for patients with disabilities and with the correct selection of the case becomes a viable option for improving the quality of life, aesthetics and function. This research aims to review the literature on orthodontic treatment for patients with disabilities, focusing primarily on cognitive and psychosocial disabilities. It also analyzed, through a survey of 42% of pediatric dentists in Costa Rica, how often disabled patients are referred to for treatment, as well as the reasons these patients are referred and the most frequents interventions. The scientific context found in literature together with the results of the country help to identify the strengths and opportunities to continue working together for accessible health services.
La población con discapacidad se ha incrementado en el ámbito mundial y, actualmente, se procura crear una sociedad más inclusiva e igualitaria. El tratamiento ortodóntico es posible para pacientes con necesidades especiales y, con la correcta selección del caso, se convierte en una opción viable para la mejora de la calidad de vida, la estética y la función. Esta investigación revisa la literatura existente sobre el tratamiento ortodóntico en pacientes con discapacidad, enfocada principalmente en las áreas cognitiva y psicosocial. A la vez, por medio de una encuesta, se analiza al 42% de los odontopediatras de Costa Rica, la frecuencia con que los pacientes con discapacidad son referidos a este tratamiento, las razones por las cuales se refiere o no a un paciente, así como la intervención y el tipo de intervenciones más frecuentes. El contexto científico encontrado en la literatura, unido a los resultados del país, permite identificar las fortalezas y las oportunidades para continuar trabajando en conjunto en pro de servicios de salud accesibles.
The patient with disability or patient with special needs (PSN) is defined as the one child or adult whose physical or mental condition prevents him or her to join the normal activities of their age group.1
There are several classifications for the various disabilities. One of the most recognized is the subdivision into four groups: 1 Cognitive disabilities, 2 Physical or motor disabilities, 3 Sensory disabilities and 4, Psychosocial disabilities.
As background, it is estimated that 12 to 18% of the world's children have special needs, either cognitive or motor.2 In Costa Rica, according to the National Census of Population and Housing of 2011,3 persons with disabilities constitute a 10.5% of the total population, an estimated of 452,859; from them, a subgroup of 10% are children, or 47,358, who represent 4% of the child and adolescent population of the country, and of which 27% have intellectual or mental problems.
Modern medicine has significantly increased the survival of PSN, by which today they make up a greater percentage of the general population. With this demographic change comes a higher need for functional orthopaedic and/or orthodontic (TO) treatment, due to a general increase in the prevalence of malocclusions.1,4 Within the current problems we have found that the literature reports that orthodontics seems to be developing more quickly in other areas than in the treatment to the PSN.5 Therefore, it is necessary to review the main obstacles that prevent orthodontic treatment, as well as the different treatment modalities that can be performed for the management of the PSN, in addition to providing guides that enable orthodontists to help these patients.1
This research aims to analyze the characteristics and orthodontic and orthopedic treatment options in the PSN population, with emphasis on cognitive and psychosocial disabilities. To achieve this goal, a bibliographic review was made on the current trends in the management, diagnosis, and treatment of PSN. It also applied a survey to specialists in pediatric dentistry, considering that they were most likely to have the first contact with these patients. The purpose of this survey was to understand three dynamics in their entirety: the frequency with which they are referred, the reasons for which they are or are not referred, the performed intervention and its characteristics.
CONCEPTUAL FRAMEWORKOrthodontic treatment (OT) need in PSNDespite the motivation of parents to improve the quality of life of their children, PSN are less likely to receive orthodontic treatment, sometimes due to their behavior problems, to the lack of ability of their parents and caregivers to assess their oral condition or because the same patient does not express the desire to do so.1,4
Studies on the effects of dental appearance on people demonstrate that orthodontic treatment is of great importance, especially regarding facial esthetics. Apart from being a source of bullying among school classmates, it has an impact on individuals and their inclusion in society.1 Authors such as Waldman et al.6 highlight the relevance of orthodontic treatment since malocclusion affects the periodontal conditions in PSN together with poor oral hygiene and medications.
Decades ago, PSN used to live in an institutionalized manner, but now they are incorporated into their families, which are fighting for their acceptance, self- sufficiency, and even their employability; in this sense, the search for orthodontic treatment is more frequent and has the aim of achieving greater facial aesthetics.6
DIAGNOSISIt has been shown that malocclusion in PSN is more frequent, more severe, and more commonly skeletal than in the general population. In certain conditions, such as Down's syndrome, mental retardation and cerebral palsy, there is a greater prevalence of some dental anomalies.1,6
The high prevalence of malocclusion in PSN relates to different variables: habits such as tongue thrusting, digital sucking and oral breathing; the presence of caries as a cause of early loss of primary teeth and dentoalveolar discrepancies; pre- and postnatal care trauma; hereditary factors; poor muscular development; suction pattern; bruxism and neuromuscular control, as well as the impact of drugs.6 Vargervik et al.7 mentioned the role of diet, which, if it is too soft, does not stimulate chewing; they also point out the constant use of baby bottle. Oliveira et al.8 indicate, moreover, that the type of disability is associated with the type of malocclusion.
With regard to the genetic role of malocclusion in PSN and its diagnosis, the role of various genes has been described in syndromic and non-syndromic patients. In the field of orthodontics, genetic studies on the development of the teeth, cleft lip and/or cleft palate and craniofacial malformations have prevailed.9 However, it is considered that genetics is as important as environmental factors regarding orofacial manifestations and this includes orthodontic and orthopedic interventions; therefore treatment should not be decided based only on the genetic component, since environmental interventions have an important role and can be successful.9
Management and patient selectionOT is contraindicated in conditions of little cooperation from the patient and/or parents, because it is difficult to obtain a positive result, in addition, iatrogenic complications in the case of caries and gingival inflammation is likely.1 Therefore, oral hygiene is the crucial factor that determines whether or not to carry out treatment, because little manual dexterity accompanied by low muscle activity can be very harmful to the patient.1
According to Becker et al.,1 other common obstacles are general behavior, excessive movement of the extremities, low level of cooperation and altered nausea reflex. All the abovementioned conditions affect treatment in a negative way, from x-rays and impressions for appliances until treatment itself.
The orthodontist must win the confidence of the patient and parents, with the purpose of having an acceptable level of cooperation.1 During the first appointment, the level of trust within the dental environment must be raised to increase the level of compliance, from both from the patient and the parents, who will be responsible for hygiene, caries prevention and care of the appliance. Additionally, the clinician must evaluate the level of cooperation that the patient will have.1,6
Subsequently, parents must be educated to recognize biofilm and gingival inflammation and to correct brushing techniques. Prior to making a commitment to the patient, parents and caregivers should take full responsibility for the patient's oral hygiene, and constantly check the gingival tissue.1 In the event that there is a negative reply, the orthodontist may refuse to provide treatment.1 This involvement of parents in their children's oral hygiene will also help the patient get used to having instruments in his or her mouth, which is one of the main obstacles for treatment.1
The management of the patient will vary depending on the disorder that he or she presents. However, several studies have shown that PSN are three times more likely to require general anesthesia for dental treatments and seven times more likely to need physical restraint than a patient without special needs.2
Another option for PSN is the pharmacologic management, which can be with sedation in the form of drops, intravenous, or with general anesthesia. Both can be used to get the most time with the patient immobilized. Multiple procedures may be combined in one appointment; this requires an interdisciplinary team: periodontists, endodontists and oral surgeons.1
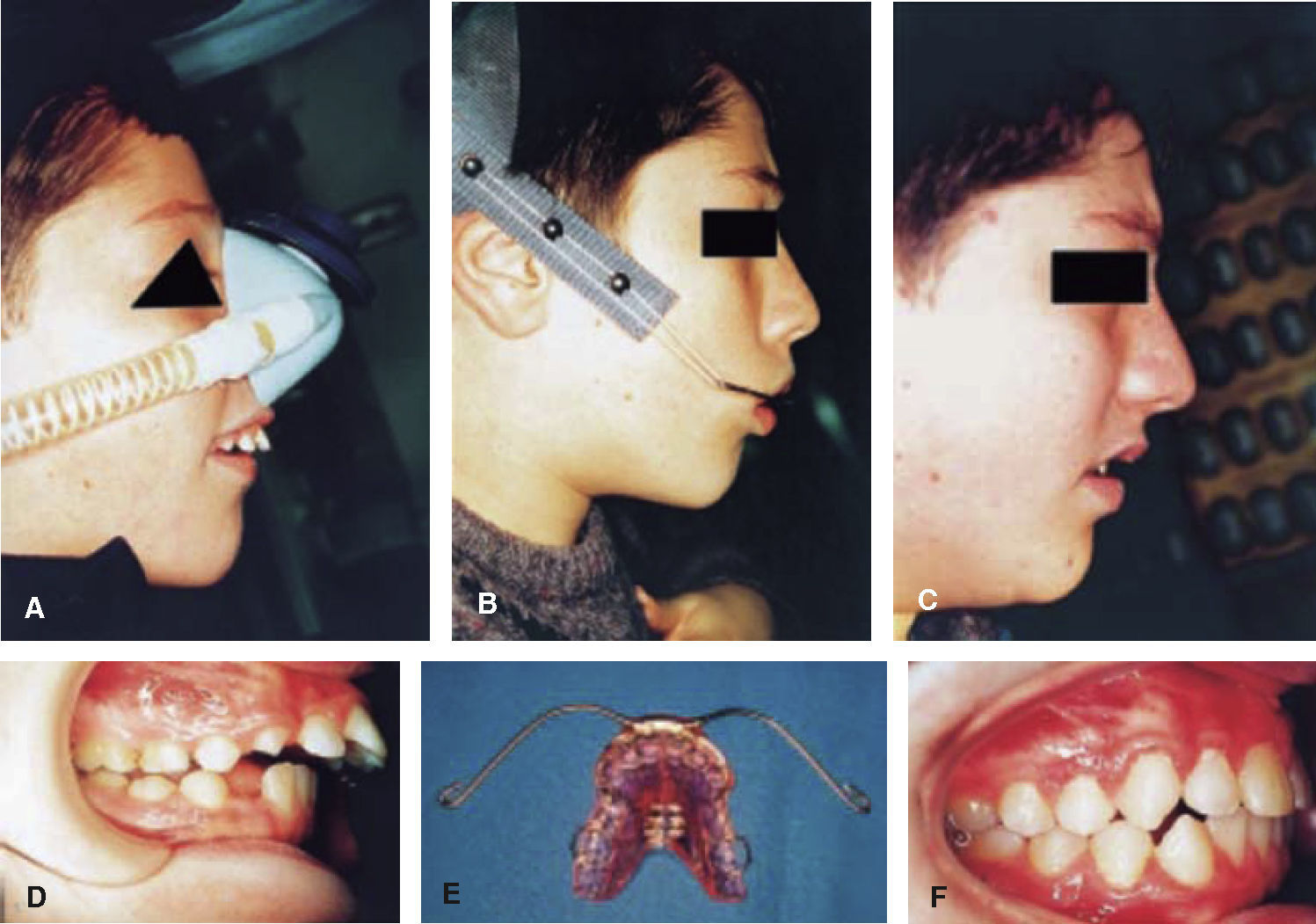
Sedation is very useful, has low risk of cardiovascular complication, is friendly with the patient and easy to operate in the private clinic. Its only disadvantage may be that it has a short effective time. General anesthesia (Figure 1) should be performed only in hospitals, as intra- and postoperative risks increase; this alternative raises the treatment cost.1
PNS in OT under general anesthesia. A. Expander placement. B. Lateral headfilm.
Source: Rada et al.10.
Chaushu et al.11 suggest taking into consideration five variables to decide if the patient can be treated without drugs for management behavior or if it is advisable to use them: nausea reflex, excessive salivation, uncontrollable movements, lack of ability to remain still, and the need to perform multiple procedures in the patient. On the other hand, Hennequin4 points out that its use is justified in the case of severe mental or behavior deficiency, failure after trying professional management or long interventions.
Once defined if the patient is candidate or not for orthodontic treatment, a general overview of treatment may be provided based on clinical examination, which demands advanced diagnostic skills on behalf of the orthodontist. Subsequently, initial records are taken. In this way, if the patient requires sedation, procedures such as impressions, X-rays, restorations, band placement and extractions, they can be performed all in one session, and if necessary the treatment plan.1
The type of disability will influence the management of the patient. In psychosocial disabilities, such as autism spectrum disorder (ASD), hypersensitivity to physical contact, difficulty for understanding social language, repetitive movements and their indifference to pain and temperature should be considered. Treatment should be based on familiar closeness, understanding the concerns and preferences of parents, the medical care of the patient, their behavior and needs.12
Patients with ASD include neurobehavioral disorders, such as autism, Asperger's syndrome, childhood disintegrative disorder and other neurodevelopmental disorders, whose prevalence in the United States is 1.1% of children. Orally, they often have a tendency to open bite, dental crowding or spacing, negative overbite and Class II molar relationship.12,13 Oral characteristics will be similar to regular patients of the orthodontic consultation (Figure 2).14 According to the specialist in orthodontics Dr. Timothy Truelove, within the main challenges in orthodontics is the management of hypersensitivity to the usual smells of a dental clinic or to flavors, such as the ones of dental materials, gloves or other objects, which increases the nausea reflex in addition to unexpected movements such as the dental chair or other.14 Some of the practices cited by Dr. Truelove are: to receive patients in a small room to talk, and not in the waiting room, surrounded by other people, or in the cubicle; observe the body language of the patient; ask the parents if the child writes well or not, and so we will know if he/she will be able to brush his/ her teeth by himself or herself or not.14 Once in clinical practice, apply the technique of Say, Show, Do, and emphasize routine. Therefore, it is recommended that their appointments are always at the same time, in the same office and with the same staff, and allow the child to bring from home some object that he or she trusts, such as a doll, a DVD, a blanket or other.14 In addition, Gandhi and Klein12 recommend visual pedagogy with books, social stories and modeling with videos.
1 Treatment performed on a patient with ASD. A and D. Initial records. B. Use of headgear to treat open bite. E. Removable appliance used to sustain the extraoral force. C and F. Final records.
Another group of PSE that will require orthodontic treatment are those with craniofacial anomalies (CA) which represent a group with diverse malformations that may or may not be accompanied by cognitive deficiencies at different levels.15 Because of the diversity of these malformations, interdisciplinary treatment is recommended and usually within a hospital environment, since patients with orofacial clefts; absence, malformation or bad position of parts of the head; lack of tissue; craniosynostosis or malformations in critical areas; impaired hearing and speech; unpredictable dental, skeletal and soft tissue development; and respiratory problems will attend the service. In these cases, the treatment goals should be very realistic and focused on improving the patient's quality of life.16 Orthodontic treatment will be indicated depending on the anomaly and the skeletal and dental development of the child,15 often accompanied by new techniques, such as distraction osteogenesis.
Prahl et al.15 points out that, in late childhood, puberty and adolescence, appearance becomes more relevant to the socialization processes and quality of life of patients with CA. To obtain treatment satisfaction, it is important the way in which the decision-making process is organized, the information available from the patient, his or her psychological condition, the establishment of risks and priorities, the ethical aspects of treatment, and the presence of realistic expectations, as well as the support of parents, schools, friends, and the health care system, which, together, will help to improve the patient's quality of life.
Within the group of patients with CA, those with craneosinostosis are relevant. Its prevalence is one out of every 2,000 births on a global scale. The multidisciplinary conference for these patients in 2010 emphasized the need for orthodontic care from infancy to adulthood, as a result of the abnormalities of shape and number, ectopic eruption and backwardness, dental crowding, maxillary hypoplasia and transverse discrepancies, which may require the joint planning of the orthognathic surgery.7
Then, as a health care professional, the orthodontist should, together with the interdisciplinary team, develop the skills and abilities required in order to provide access to orthodontic treatment for the PSN.
Treatment planOrthodontic treatment plan should be directed to improve alignment and occlusion, with very clear objectives, so as to improve their personal appearance. Although treatment need is very high and provides major benefits for the patient, currently it continues to be elective for these patients.1 It is recommended to begin treatment with a removable appliance, in order to confirm patient cooperation, hygiene and the ability to follow simple instructions; if the case allows, treatment may extend to the use of the removable appliance with or without extraoral force. The use of fixed appliances must be limited using devices with a wide range of action, which require less appointments and, in the case of fixed appliances, special auxiliaries and active bends.1
Becker et al.5 applied a survey to the parents of thirtyseven PSN who wore orthopedic appliances in order to understand the main disadvantages experienced by patients from the day of the placement until the end of treatment. The disabilities in this sample were: 40% mental retardation, 13% Down syndrome, 12% cerebral palsy and, to a lesser percentage, autism and neurological syndromes, such as Behr and Coffin Lowry. The two major orthodontic problems that the patients experienced were open bite and crowding.
This group of researchers found that 95% of the population accepted the appliance and achieved the treatment goal; 21% of the group tried to remove it in the first few days, but finally accepted it.5 For parents, the two major difficulties were the children's oral hygiene and taking them to the follow-up appointments; few of them mentioned the daily placement of the appliance. However, the researchers concluded that motivated parents cooperated in order to achieve the objectives and that institutionalized patients had greater difficulty for treatment.5 According to the parents, the use of fixed appliances was more complicated than that of removable ones. The researchers point out, moreover, that 5% of the patients discontinued treatment, a much lower figure than the number of patients without special needs who abandon their orthodontic treatments.5
As to the best appliances, certain criteria have been found in the literature. Becker et al.1 indicates that problems with fixed appliances tend to be more frequent than with removable appliances. For that reason, it is recommended to extend the first phase as far as possible, with the use of extraoral forces or without them, to shorten the second stage. Also, consideration should be given to the redesign of the appliances in order for them to be more patient- resistant and less patient-dependent.1 Abeleira et al.17 determined the opposite: parents of sixty PSN reported an excellent adaptation to fixed appliances, but poor adaptation to removable appliances.
Considering the abovementioned facts, appliance placement should ponder two important variables: isolation and proper placement. In the case of isolation, a rubber dam may be used as well as the best adhesive materials to prevent bracket debondingand the risk of it being swallowed by the patient; another useful option is the use of antisialogogues or specialized suction systems. Given the difficulty of rebonding brackets, a recommendation is to use indirect bonding, which shortens chair time with the patient and provides good accuracy.1
In extraction cases, the correction of anteroposterior and vertical discrepancies with removable extraoral orthopaedic appliances is highly recommended, and afterwards, begin the intraoral work. This protocol limits or eliminates the use of intermaxillary elastics, which decreases the need for cooperation of caregivers and patients in this regard.1
Becker et al.1 state that the PSN require more time and more appointments. In this aspect Taddei et al.,18 coincide. They compared PSN, specifically with CA, and patients without them, and they also found significant differences in the number of appointments, treatment time, age of onset or age of completion. On the other hand, performing a similar comparison, Blanck-Lubarsch et al.19 concluded that no more treatment time is needed nor more appointments, but that the duration of the appointments is larger.
With regard to the retention period, it may be that the etiology of the malocclusion is not resolved in its entirety in all patients. Thus, skeletal vertical problems or macroglosias may not achieve post-treatment stability. This must be communicated to the patient from the beginning and the retention period must be prolonged.1
A questionnaire applied to parents of PSN showed that, although the results did not comply with all the treatment goals, their perception of dental and facial changes was positive. They also noted improvement in oral functions such as swallowing, speech, and even chewing. Also, they noted that the PSN were aware of the improvement in their appearance, and this increased their self-esteem and confidence.1
MethodologyIn order to build the reference framework, a literature review was conducted in Science Direct, EBSCO, PubMed, Cochrane and in the search engines of the major journals of orthodontics and dentofacial orthopedics at global level. The following key words were used: «patients with special needs», «autism», «craniofacial abnormalities», accompanied by «orthodontic treatment», during the period from March to May 2016. No systematic reviews, meta-analysis, and randomized controlled trials or cohort studies were found. The selection of articles for inclusion in the reference framework was based on their scientific validity and their content related to the topic (Figure 3).
The information was completed with an observational, cross-sectional and descriptive study, in order to analyze the orthodontic and orthopedic treatment characteristics and options for the patient with special needs, mainly cognitive, and psychosocial. In order to do this, a survey of nine questions (Appendix 1), was applied either in person or sent by email to 75% of the pediatric dentistry specialists in the country. A one- month period to respond was provided. Response was obtained from thirty-two specialists, the equivalent of 42.6% of the specialists in the country.
The survey had the objective to determine the frequency with which they refer patients with special needs to orthopaedic and/or orthodontic treatment, the reasons for deciding to do it or not and the characteristics of such treatment in this population.
RESULTSThe response of the paediatric dentistry specialists was good, since answers were obtained from 42.6% of the specialists at national level during the five weeks of information gathering.
It can be observed that the referral level of PSN to orthodontic treatment is low: 70% of the specialists refer less than 10% of these patients to the orthodontist (Figure 4).
From the PSN referred to, the majority corresponds to the phase of fixed orthodontic appliances, brackets, as shown in figure 5.
With respect to the main reasons that incline pediatric dentists to refer PSN to orthodontic treatment, the most important thing for them is whether it is possible to achieve patient cooperation, followed by the cooperation of parents and, thirdly, the state of oral health (Figure 6). The deficiency of these three conditions, in that order, is the reason why they decide not to refer a PSN for OT; added to this is the compromised systemic health (Figure 7). When questioned, the pediatric dentists answered that the less decisive factor for referral would be visual capacity because the specialists believe that a patient with visual disabilities can cope with OT.
In relation to the types of disabilities that referred PSNs present, the main ones were: autism spectrum disorders and Down syndrome followed by mental retardation, and, to a lesser extent, cerebral palsy; the specialists mentioned, in addition, ectodermal dysplasia (Figure 8).
About the perception of treatment their PSN receive, 80% of pediatric dentists responded that the experience was positive, which increases if the orthodontist to whom the patient will be referred to is selected properly and also, if the patient is motivated. The specialists who reported regular to bad experiences found obstacles in the little cooperation and tolerance of parents with regard to prolonged treatments; at other times, the importance of the aesthetic and functional improvement of the special patients was belittled, by the orthodontist, the family, or both (Figure 9).
With regard to the appliances used, the pediatric dentists refer that mainly fixed orthodontic appliances with brackets were placed, followed by lingual arches and removable circumferential appliances, among others (Figure 10). In addition, they mentioned others than the given choices, such as expanders.
Finally, the specialists were asked how often they did consult their orthodontist on PSN cases. Almost 50% responded that they do so in 80% of the cases or more; it is the same frequency with which they consult with other specialties if the case requires it as well.
DISCUSSIONGenerally speaking, the results show that the specialist in pediatric dentistry detects malocclusion problems in their PSN and includes them in his or her list of problems, since the survey reveals that more than 50% performed interconsultation with their orthodontist for 80% of their PSN cases. However, when analyzing figure 4, only 20% of the specialists referred more than 50% of their PCNE for OT, and the majority (70%) refers less than 10% of them.
The reasons for this difference between consultation and reference can be related to the factors listed in Figures 6 and 7, where patient and parents cooperation is the first factor to decide if they refer the case for orthodontic treatment. However, there may be reasons not exposed in this investigation, such as if the patient is being seen in the health care system, public or private, or empathy with the orthodontist selected by the dentist to advocate for the treatment of PSN.
It should be noted that, in spite of the low referral rate, when it occurs, the pediatric dentists refer a positive experience in 80% of cases. This denotes a proper analysis for selecting the patients and a good conclusion of the case on behalf of both specialists.
The answers given by the specialists to this survey posed major challenges for the orthodontists and for the university curriculum. According to the results, 65% of the referred patients are sent for fixed orthodontic appliances, a result that may be related to the fact that pediatric specialists are trained to perform orthopedic treatments. For this reason, the orthodontist must possess the skill and the ability to perform indirect bonding, or a quick placement of brackets, in order to end the appointment quickly, which is an important aspect when treating PSN. In addition, the orthodontist should have the skill and knowledge of biomechanics to be able to propose amendments to the basic fixed and removable orthopaedic appliances in order to resolve with a single appliance the greatest amount of orthodontic and orthopedic problems. In this way, alginate impressions will be minimized and will avoid changing the appliances, since the latter will force the PSN to habituate back to something new in his or her mouth, which will not be easy.
Communication between the specialist and the parents will be key for the treatment to be perceived as successful, although not every treatment goal is achieved or even without good compliance from the patient.
With the aim of improving the equity of access to health services for patients with PSN, this kind of surveys may be conducted in other areas of dentistry. In this research, we selected pediatric dentists because, in Costa Rica, they tend to attend PSN in the first instance, both in public consultation and in private; in addition, by being a smaller group of specialists compared to the orthodontists, contact was easier and so was to obtain a representative sample. Other studies could include general dentists, or modify the survey to apply to specialists in orthodontics and functional orthopedics, as well as adding some questions to learn if the respondent works in the public or private sector and to be able to infer the needs of each sector.
CONCLUSIONSAesthetic requirements and egalitarian inclusion into society cause a greater search for orthodontic services on behalf of PSNs and their families. In this situation, it is necessary to educate all those people who live or work with PSNs, with regard to the possibility of orthodontic treatment and its benefits. The orthodontist, in addition, must know possibilities and changes in the traditional treatments of orthodontics and orthopedics to treat PSN cases, and communicate them to other areas of dentistry with the aim of increasing the access of these patients to health.
In Costa Rica, pediatric dentists conduct interconsultations for the orthodontic treatment for these patients in more than 80% of the cases, but only less than 10% receive treatment. This raises the need to analyze options and variations on the traditional treatment plan in order not to exclude this population of the benefits of orthodontic treatment, both in the public service as well as in the private sector, with the purpose of ensuring equality. The treatment that is performed the most is placement of fixed orthodontic appliances with brackets.
It is recommended to include this topic since the undergraduate career in dentistry, as well as in graduate studies of pediatric dentistry and orthodontics, which can contribute to conduct more research in this regard and with greater scientific validity than what is currently published. Equally, it is important to consider this way of working in all specialized dental services in the public sector with the aim of providing greater accessibility to this treatment, which, without a doubt, can improve the quality of life for those living with a disability.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia
Odontology Graduate, Universidad de Costa Rica. Specialist in Stomatology in Primary Care, Universidad Nacional Autónoma de México. Resident of the Orthodontics and Functional Orthopedics, Universidad Latinoamericana de Ciencia y Tecnología (ULACIT), San José, Costa Rica.