Patient treated in the clinic of Orthodontics of the Universidad Autonoma de Guadalajara, referring as reason for consultation «I can not eat comfortably and I feel ashamed of my facial appearance». A full dentofacial study was conducted. The patient was diagnosed with a skeletal class III malocclusion caused by maxillary hypoplasia and mandibular prognathism. Surgical-orthodontic treatment was determined. The patient and his parents were informed about the treatment, risks, benefits, advantages and disadvantages, duration of treatment, costs and post-operatory care. Once the treatment plan was accepted, the objectives were to achieve skeletal class I as well as bilateral canine class I and molar class II. 0.022 Roth appliance placement was indicated with upper 1st premolars extractions, going through the stages of alignment, leveling and space closure. We worked as a team with the Department of Surgery. A successful treatment of pre-surgical orthodontics and maxillofacial surgery (maxillary advancement and mandibular retroposition) was achieved thus obtaining as a result skeletal class I, canine class I and bilateral molar class II. The patient recovered his chewing function and self-esteem by being aesthetically accepted by society.
Paciente tratado en la Clínica de Ortodoncia de la Universidad Autónoma de Guadalajara, refiriendo como motivo de consulta «no puedo comer a gusto y siento pena por mi apariencia facial» se realizó estudio dentofacial completo. Se diagnosticó clase III esqueletal ocasionada por hipoplasia maxilar y prognatismo mandibular, se determinó tratamiento orto-quirúrgico. El paciente y sus padres fueron informados sobre el tratamiento, riesgos, beneficios, ventajas y desventajas, duración de tratamiento, costos y cuidados a seguir. Una vez aceptado el plan de tratamiento, los objetivos fueron lograr clase I esqueletal así como clase I canina y clase II molar bilateral, se indicó colocar Aparatología Roth 0.022”, se le realizaron extracciones de las primeras premolares superiores, así como las etapas de alineación, nivelación y cierre de espacios, se trabajó en equipo con el Departamento de Cirugía, se obtuvo un exitoso tratamiento de ortodoncia prequirúrgica y cirugía maxilofacial (avance maxilar y retroposición mandibular), obteniendo como resultados clase I esqueletal y clase I canina y clase II molar bilateral, devolviendo al paciente la función masticatoria y la seguridad en su persona por sentirse estéticamente aceptado ante la sociedad.
Angle's publication of the classification of malocclusions in the 1890's was a very important step in the development of orthodontics, since it did not only sub-classify the main types of malocclusion, but also described the first clear definition of normal occlusion. Angle postulated that the first upper molars were fundamental in the occlusion and that the upper and lower molars should be linked together so that the mesio-buccal cusp of the upper molar occludes with the buccal groove of the lower first molar. If the teeth were aligned in an evenly curved line of occlusion and this relationship between the molars exists, there would be a normal occlusion. Subsequently Angle described three types of malocclusion, based on the occlusal relationships of the first molars:
Class I: normal relationship of the molars, while the line of occlusion is incorrect by dental malposition, rotations or other causes.
Class II: lower molar located distally in to the upper, without specifying occlusion line.
Class III: lower molar located mesially in relation to the upper molar, without specifying the occlusion line.1
Graber describes class III as true dento-skeletal dysplasias, where an anteroposterior relationship of the jaws in relation to the cranial base is recognized, with or without teeth irregularities.2
In the decade of the 1930's radiographs clearly showed that many class II and class III malocclusions were due to anomalies in intermaxillary relations and not only to teeth malposition.3
Class III occlusal relationship seems to be particularly common in Asian population (12%) and comparatively less frequent in Europeans (1.5-5.3%) and Caucasians of North America (1-4%).4,5
The etiology is linked to hereditary factors influenced by the environment and according to their origin they are classified in skeletal, dental and/or functional.6
Class III malocclusions can often be present with mandibular prognathism, but these occlusal relations constitute only a part of a much larger syndrome. In fact, in class III patients almost any combination of poor growth of the maxilla and excessive development of the mandible can be found being the two equally probable.1,7
Ellis and McNamara found in his study that a combination of maxillary retrusion and mandibular protrusion was the most common skeletal relationship, with a prevalence of 30% in class III adult patients. Maxillary retrusion with normal mandible had 19.5% predominance and a normal maxilla with mandibular protrusion represented 19.1% of patients.7
Determinants of occlusion, such as interocclusal distance, mastication movement and tooth-to-tooth relations vary for the different kinds of occlusion. The class III patient is subjected to changes in occlusal patterns because occlusal morphology is determined by the length and size of the mandible. Therefore, prognathism may be a feature responsible for class III malocclusion.8
To perform a suitable cephalometric analysis is essential to confirm the presumptive diagnosis. Determining the actual origin of the anomaly allows us to formulate an appropriate treatment plan, surgical or non-surgical, that responds to the demands of the patient and the clinician.9
According to Proffit the orthodontist is usually the key person in deciding the appropriate time to begin treatment plans that are located within one of the following categories: orthodontic treatment only, orthopaedic and orthodontic treatment (growth modification) and orthodontic-surgical treatment.1
Indications for surgery are a problem too broad for orthodontics. The boundaries of orthodontic treatment vary in function of the required dental movement (teeth can move more in some directions than in others) and the patient's age (limits for dental movement vary little or nothing with age, but growth can be modified only during the phase of active growth). It should be borne in mind that the discrepancy sets the limits of the changes in the hard tissues toward an ideal occlusion; provided that other limits linked to the priority goals of treatment were not implemented. The limitations set by the soft tissues tend to be a very important factor in the choice between orthodontic treatment or an orthodontic-surgical one.1,9
Jakobsone, Stenvik and Espeland concluded in their study that bi-maxillary surgery (LeFort I and bilateral sagittal osteotomy) to correct skeletal class III malocclusions gives as a result the following aspects: 1. Good occlusal Stability, 2. The stability of the maxillae varies depending on the number and direction of the surgical movements, 3. The risk factors for the horizontal relapse of the mandible were the amount of retroposition and for the vertical relapse it was the posterior repositioning of the maxilla, 4. Dentoalveolar compensations contribute to the occlusal stability, hence the importance of orthodontic treatment after surgery and stabilization.10
There are reports in the literature about the negative effect that any facial disfigurement has on the mental and social well being of the individuals and this is clearly the reason why the majority of the patients are seeking orthodontic treatment. If improving facial appearance is the main goal of treatment, it makes sense that in addition to the jaws and teeth, changes in the nose and contours of the facial soft tissues should also be considered. It is therefore very important to provide counseling and psychological support to patients.1,11
NiMhurchadhaen, Bhamrah and Ahmad in their study show that surgical patients turn to the Internet for supplementing information on their proposed treatment. This may suggest a possible gap in the information provided by the clinician. However, it is evident that patients use Internet forums to seek additional information, support and comfort from persons who have undergone a similar treatment. So, it is necessary that the clinicians make sure that the patients have access to the adequate and pertinent Internet resources.
CASE REPORTDiagnosis and treatment planPatient of 15 years of age, male gender, without relevant medical history attended the clinic of Orthodontics at the Faculty of Odontology of the Autonomous University of Guadalajara referring as reason for consultation «I cannot eat comfortable and I feel ashamed of my appearance».
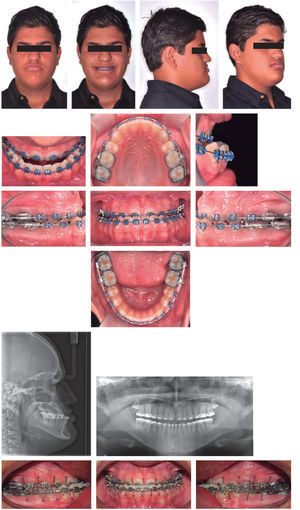
The patient had a brachifacial biotype, slightly increased facial lower third, the internal edge of the eyes coincided with the wings of the nose, mouth width matched the inter-iris distance, straight forehead, straight nasal septum, concave profile, augmented cervico-mental distance, decreased naso-labial and mento-labial angles, lip competence, thick lips, lips behind the aesthetic line, lower lip slightly everted and poor malar development (Figure 1).
At the intraoral analysis, he presented with an anterior crossbite, lower dental midline deviated with regard to the upper 2mm towards the right, overbite of -2mm overjet of -1mm, bilateral Class III molar relationship, bilateral canine class III, Ovoid upper and lower archform, mild crowding, rotations and a 3mm curve of Spee (Figure 2andTable I).
Discrepancy analysis for both arches.
| 1M | 2P | 1P | C | IL | IC | IC | IL | C | 1P | 2P | 1M | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Up | 10 | 7.5 | 7 | 8 | 7 | 8 | 8.5 | 7 | 7.5 | 7 | 7 | 10 | 94.5 |
| Low | 11 | 7.5 | 7 | 7 | 6.5 | 5.5 | 5 | 6 | 7 | 7 | 7 | 12 | 88.5 |
| Upper arch | Lower arch |
|---|---|
| Available space: 72 mm | Available space: 66 mm |
| Required space: 74.5 mm | Required space: 65.5 mm |
| Total discrepancy: -2.5 mm | Total discrepancy: +5 mm |
The panoramic radiograph evidenced the presence of the upper and lower third molars germs, apparently healthy alveolar ridges and good root length (Figure 2). The lateral headfilm was traced with Steiner cephalometric analysis resulting in a class III malocclusion cephalometric diagnosis due to a bimaxillary problem. The patient also presented a dental compensation through upper incisor proclination and lower incisor retroclination. The skeletal, dental and soft tissues characteristics provided the diagnosis of a skeletal class III patient due to a maxillary hypoplasia and mandibular prognathism (Table II).
Initial cephalometric values.
| Steiner cephalometric analysis | ||
|---|---|---|
| Angle | Normal value | Patient |
| SNA | 82° | 92 |
| SNB | 80° | 96 |
| ANB | 2 | -4 |
| GO-GN:S-N | 32 | 25 |
| OCCL:S-N | 14.1° | 2 |
| INTERINCISAL | 131 | 135 |
| ⊥ - N-A | 4mm | +4 mm |
| ⊥ N-A | 22° | 28 |
| T – N-B | 4mm | +3 mm |
| T N-B | 25° | 20 |
| T GO-GN (IMPA) | 93° | 78 |
| Others | ||
| Witts | H -1 mm | -7 mm |
| M 0 mm | ||
| ⊥ - Maxillary plane | 110 | 123 |
Treatment goals:
They were divided into three groups:
- •
Skeletal:
- -
Correct the class III by orthodontics and orthognathic surgery, and achieve skeletal class I.
- -
- •
Dental:
- -
Coordinate arches for surgery.
- -
Achieve bilateral canine class I.
- -
Procline lower incisors and retrocline upper incisors.
- -
Correct upper and lower crowding.
- -
Eliminate rotations.
- -
Correct midlines.
- -
- •
Soft tissues:
- -
Improve profile.
- -
Correct naso-labial and mento-lip angles.
- -
It consisted of placement of conventional appliances, Roth technique 0.022” slot with bands in first and second upper and lower molars as well as upper premolar extractions. The stages of alignment, leveling and space closure (by retraction of the upper anterior segment) were carried out; the pre-surgical evaluation was performed together with the maxillofacial surgeon and the maxillofacial surgery was planned. Once the patient was operated he was received again in the clinic of orthodontics to perform the final stages of detailed, settlement and retention.
Treatment progress:
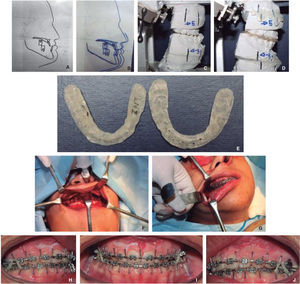
Treatment was initiated with Roth 0.022” slot conventional appliances placement with 0.014” NiTi arch wires in both arches, cinched only at the upper arch to avoid upper incisor proclination and left without cinching in the lower arch seeking proclination throughout the treatment (Figure 3).
After three months 0.016” NiTi arch wires were placed in both arches, with small loops (teeth #35-36 and 45-46) that worked as stops to leave the lower arch larger in the anterior zone and help proclination of the lower incisors. With these arches, the alignment stage was concluded. (Figure 4).
The patient was referred to perform the extractions of the first upper premolars on both sides (#14 and 24).
After two months, 0.016” × 0.016” stainless steel arch wires were placed in both arches, which performed the leveling and space closure stages. This last stage was carried out with the help of closed coils that were activated 2mm per month (Figure 5).
Initially, only the upper canines were distalized in order to achieve canine class I, afterwards the lower arch was changed for a 0.018” NiTi with loops again to continue with the proclination.
After three months, a lateral headfilm was obtained to assess the inclinations of the upper and lower incisors; the radiographs provided as a result that both the upper and lower incisor inclinations were within the normal values (Figure 6).
Retraction of the upper anterior segment was begun by placing hooks in the anterior zone so that aided by closed coils (14 oz/on each side), the upper extraction spaces were closed completely. In the lower arch, small diastemas created by the proclination were closed using elastic string. The patient was instructed to extract the lower third molars.
After two months the spaces of both arches were closed completely 0.016” × 0.022” NiTi arch wires were placed on both arches and impressions were taken to assess arch coordination which was very favorable (Figure 7).0.017” × 0.025” stainless steel arch wires were placed and the patient was referred to the maxillofacial surgeon for an assessment. After three months surgical arch wires were placed.
The maxillofacial surgeon instructed the patient to obtain full digital records (panoramic X-Rays, lateral headfi lm and intra and extra oral photographs) before the surgery (Figure 8).
Four days prior to the surgery, the soft tissue analysis (Bell), surgical prediction (5 mm maxillary advancement and 3 mm mandibular retrusion), models surgery and the elaboration of the two surgical splints (intermediate and fi nal) were all performed in conjunction with the maxillofacial surgeon.
After 16 months the orthognathic surgery was performed in which a 5mm maxillary advancement was made and a mandibular retrusion of 3mm (Figure 9). The patient was told to use intermaxillary elastics (1/8”, 3.5 oz squirrel), to overcome the muscular forces.
One month after the surgery, the patient attended the clinic of orthodontics, where the surgical arches were withdrawn and coaxial 0.019” × 0.025” stainless steel arch wires were placed, still with intermaxillary elastics in the posterior area to assist in the settlement of the occlusion. A panoramic X-Ray was indicated to evaluate root parallelism (Figure 10).
A 0.017” × 0.025” TMA arch wire was placed in the upper arch, the bracket of tooth #11 was repositioned and in lower arch, a 0.017” × 0.025” stainless steel arch wire was placed with progressive positive torque on the left side (teeth #33-37).
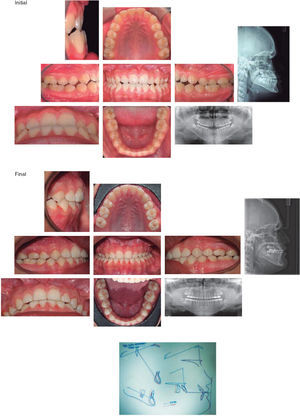
After three months 0.017” × 0.025” stainless steel arch wires were placed in both arches, cinched, and crossed intermaxillary elastics (1/8”, 3.5 oz) were indicated on the left side, to improve the posterior occlusion. Final panoramic radiograph and lateral heafilm were obtained (Figure 11).
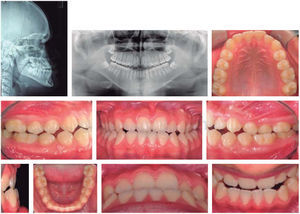
After 22 months of treatment and once the objectives were achieved, it was decided to remove the appliances. The patient was referred to the periodontist for prophylaxis and the retention stage started with a 3-3 lower fixed retainer and a removable circumferential retainer in the upper arch to help close the remaining spaces of the bands (Figure 12).
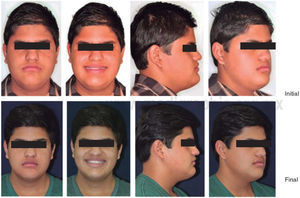
RESULTSA skeletal class I was obtained along with a canine class I and a molar class II, favorable inclinations of the upper and lower incisors, a normal overjet and overbite, midlines centered, straight profile, facial harmony, lips on the same plane, friendly smile, and an adequate masticatory function (Figure 13), as well as important changes in the cephalometric values (Table III).
Initial and final cephalometric values.
| Steiner's cephalometric analysis | |||
|---|---|---|---|
| Angle | Norm | Initial | Final |
| SNA | 82° | 92 | 94 |
| SNB | 80° | 96 | 93 |
| ANB | 2° | -4 | 1 |
| GO-GN: S-N | 32° | 25 | 26 |
| OCCL: S-N | 14.1° | 2 | 3 |
| Interincisal | 131° | 135 | 135 |
| ⊥ - N-A | 4 mm | +4 mm | +4mm |
| ⊥ y N-A | 22° | 28 | 23 |
| T - N-B | 4 mm | +3 mm | +2mm |
| T y N-B | 25° | 20 | 20 |
| T y GO-GN (IMPA) | 93° | 78 | 80 |
| Others | |||
| WITTS | H -1mm | -7 mm | -3mm |
| M 0mm | |||
| ⊥ -Maxillary plane | 110° | 123 | 119 |
Jakobsone, Stenvik and Espeland concluded in their study that the risk factors for horizontal mandibular relapse were the amount of retrusion and vertical and posterior repositioning of the maxilla. Stability increased in patients with little or no posterior impaction of the maxilla.10 In the case of the patient hereby presented, a 5mm maxillary advancement was conducted as well as a mandibular retroposition of 3mm. Seven months after surgery no sign of relapse has been found, the case has remained stable. These results support the study in that stability is due in part to the fact that maxillary impaction was not performed, but we also believe that it was due to a good surgical and orthodontic management.
We agree with the research of Dr. Cho in that the postsurgical occlusal results depend on the precision and stability of the surgery. Dentoalveolar compensations contribute to occlusal stability, stressing the importance of finishing with a postsurgical and stabilization orthodontic phase.12
Proffit, Jackson and Turvey argue in their study that the characteristics of patients who seek and accept orthognathic surgery appear to be changing in the twenty-first century. The percentage of class III patients increased from 35% to 54% and the percentage of class II patients was reduced from 59% to 41%, whereas the percentages of long face and asymmetry showed little change. The decrease in class II patients was an accentuation of a long-term trend; the increase in class III patients occurred only after the turn of the century.13
Nicodemus, Pereira and Ferreira concluded that female patients presented increased self-esteem and decreased depressive symptoms due to the surgical intervention; while male patients showed no alteration in their self-esteem and depression with the surgical intervention. In our clinical case, the patient showed positive changes in his behavior after the surgery.14
Ertas and Kilinc believe that the level of quality of life related to the oral condition of surgically treated patients, may reach those of individuals without a dentofacial deformity, once the effects of the treatment process have disappeared. The latter statement coincides with the changes that the patient hereby presented some time after surgery.15
At the start of treatment, it was suggested to perform surgery in both jaws, assess the results and if necessary, perform a second surgical intervention to retrude the chin and aesthetically achieve a more straight profile, but when the patient saw the final results he did not think it was necessary.
CONCLUSIONSWhen the orthodontic problems in adult patients are so serious that they were not modified during the growth stage, when it is demonstrated that it is a skeletal problem and not a dental one and that not even camouflage is a good solution, the only possible treatment is surgical realignment of the jaws and the relocation of the dentoalveolar segments.
In this kind of patients, orthognathic surgery is not a substitute for orthodontics, but rather an interdisciplinary complement where there must be coordination with other dental treatments in order to achieve overall acceptable results. Currently the spectacular advances in medical science have made it possible to combine these treatments to correct many serious problems with the best results.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia