Acupuncture is a traditional Chinese medicine tool used to harmonize human body physiology, restore impaired functions and cure diseases by means of applying needles at specific points on the body surface. It has proven effects of local and central analgesic action, anti-inflammatory action, anxiolytic action and improved immune defence. Temporomandibular dysfunction (TMD) is of complex and multifactorial aetiology because involves anatomical, occlusal, muscular and psychological factors. In order to evaluate the efficiency of Chinese acupuncture in the treatment of these disorders, 20 fully dentate volunteers aged 18 to 30 years were selected, divided into moderate TMD and severe TMD (n=5), treated with traditional Chinese acupuncture or sham acupuncture (control groups). All volunteers were treated with ten sessions of acupuncture, one per week, in which the needles were inserted in local and distant points to the temporomandibular joint, so that there was organism restoration and the remission or reduction of symptoms. The results showed that the technique used was effective in the control and remission of temporomandibular dysfunction signs, and all volunteers, at the end of treatment, were considered non temporomandibular patients.
La acupuntura es una herramienta de la medicina tradicional china que se utiliza para armonizar la fisiología del cuerpo humano, restaurar las funciones deterioradas, y curar las enfermedades mediante la aplicación de agujas en puntos específicos de la superficie corporal. Tiene efectos demostrados de acción analgésica local y central, acción anti-inflamatoria, acción ansiolítica, y mejora de la defensa inmune. El trastorno de la articulación temporomandibular (ATM) es una etiología compleja y multifactorial, ya que implica factores anatómicos, oclusivos, musculares y fisiológicos. A fin de evaluar la eficiencia de la acupuntura china en el tratamiento de estos trastornos, seleccionamos a 20 voluntarios totalmente dentados, con edades comprendidas entre 18 y 30 años, divididos en grupos de trastorno de la ATM moderado y severo (n=5), tratados con acupuntura china tradicional o acupuntura “sham” (grupo control). Todos los voluntarios fueron tratados con diez sesiones de acupuntura, una por semana, insertándose las agujas en puntos locales y distantes de la articulación temporomandibular, para restauración del organismo y remisión o reducción de los síntomas. Los resultados reflejaron que la técnica utilizada fue efectiva para el control y remisión de los signos del trastorno temporomandibular, comprobándose al final del tratamiento que no podía considerarse a los voluntarios pacientes de dicho trastorno.
The temporomandibular joint (TMJ) is considered one of most complex joints in human body, since it is able to perform various movements associated with action from masticatory muscles, making possible the accomplishment of stomatognathic functions. TMJ is related to these functions, influencing and being influenced by all the organs that make up this system: tongue, lips, hard and soft palate, teeth, blood supply, nervous supply, maxilla, mandible and chewing muscles. The dysfunction of that joint, called temporomandibular dysfunction (TMD), is a condition in which there is disharmony in stomatognathic system, may occur involvement and injury in masticatory muscles, in TMJ itself, or both, being classified, respectively, as muscular, articular and muscle-articular or mixed.1–3
TMD etiology is complex and multifactorial, since it involves factors of anatomic, occlusal, muscular and psychological origin. Among the main etiological factors are myofunctional changes, dental malocclusion, poor habits generating muscular hyperactivity and consequent overload in joint, emotional troubles, stress, among others. TMD is usually characterized by presenting signs and symptoms, such as pains involving chewing muscles, preauricular region, the joint itself, clicks and crackling in articulation, reduction of mandibular movements with functional limitations.4–6
Treatment of TMD aims to control all signs and symptoms that characterize it, especially the relief of chronic pain. When treatment for this dysfunction is performed, the professional aims to eliminate or minimize etiological factors and signs and symptoms that bring discomfort to patient, and are usually classified how definitive or supportive treatment.3,7 Acupuncture is considered a supportive therapy, since it aims at reducing physical signs and symptoms presented by patient; but also can be considered as definitive treatment, since it acts similarly on TMD etiological factors.8
Acupuncture treatment can be based on a variety of techniques, among them the choice of local and distance points, use of extraordinary vessels, unitary energy channels, tendinomuscular channels, among others. Thus, considering a person with TMD, should be recognized the channels or meridians of energy that pass through TMJ region, the chewing muscles and also those related to pain must; in this case highlighting meridians of Dan, Da Chang, Wei, San Jiao and Xiao Chang. It should also be considered Gan, which in Chinese medicine governs ligaments and tendons, structures naturally involved in TMJ dysfunction.9–13 The literature shows that acupuncture has its good results in chronic pain treatment, as in TMD, due to its anti-inflammatory, anxiolytic and myo-relaxing properties and activating immune function in human organism.14–21
Thus, the objective of this research was to perform treatment in individuals with temporomandibular dysfunction by means of use an Acupuncture protocol, since this disturb affects a large number of people and therapies normally used are not fully effective in signs and symptoms control presented by patients with TMD.
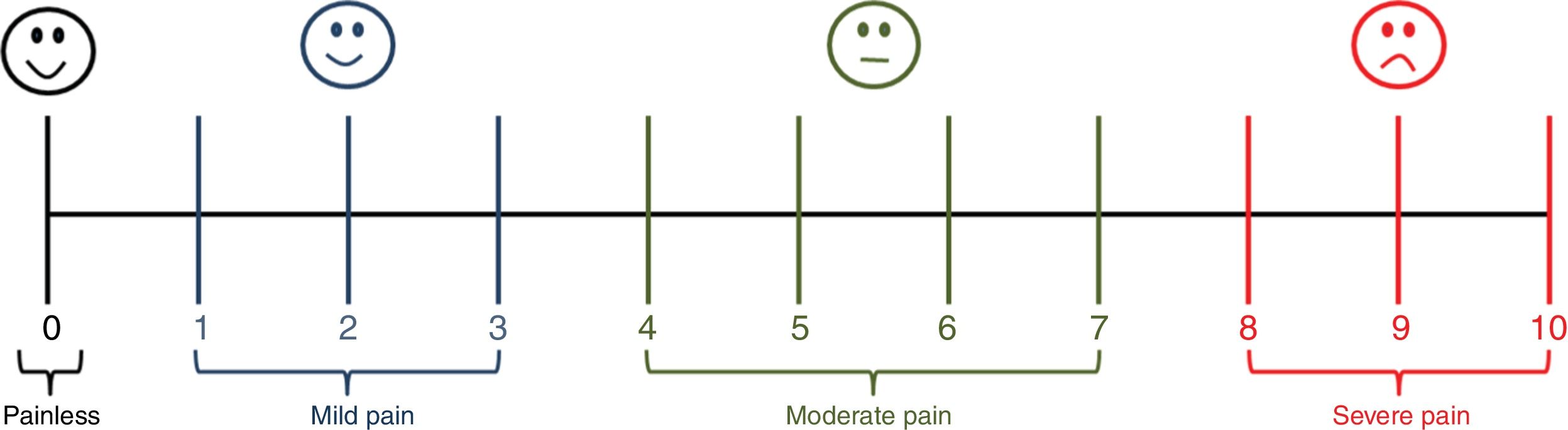
MethodsTwenty volunteers, female, independent of color and race, aged between 18 and 30 years, all teeth, with temporomandibular dysfunction, diagnosed and classified by means of a questionnaire recommended by Fonseca et al., 1994, analyzed and validated by literature22,23. Volunteers were divided into four groups (n=5), with moderate and severe TMD, treated with Chinese Traditional Acupuncture (CTA) or Sham acupuncture - control (SA). Before each session, a visual analogical pain scale was shown to volunteers (figure 1), so that could quantify this symptom and to allow the comparison. The research was approved by Ethics Committee in Research of Federal University of Alfenas, with number CAAE 48021715.4.0000.5142.
In each acupuncture session, in treated groups with CTA, the following points were used: GB41 (Zulinqi), TB5 (Waiguan), LI4 (Hegu), ST6 (Jiache) and TB17 (Yifeng). After introduction of needles, they were manipulated until each volunteer manifested De Qi. These points were chosen because of energetic functions they present, which are extremely useful for temporomandibular dysfunction treatment. The points GB41 (Zulinqi) and TB5 (Waiguan) are opening points of two extraordinary vessels, respectively Dai Mai and Yang Wei Mai. These extraordinary vessels act as Qi reservoir in relation to main meridians; point LI4 (Hegu) is the Yuan point of Da Chang meridian and is one of Acupuncture points that acts on harmonization in High and Low energy and acts on Yang Ming's circulation; point ST6 (Jiache) has the main energy functions of strengthening the teeth and mandible, improving the Qi of the TMJ, removing the Qi obstruction in energy channels, dispersing the perverse wind and cold, cleaning the perverse heat and relaxing the facial muscles, being indicated for temporomandibular joint dysfunctions; and TB17 (Yifeng) is used to strengthen the Triple Burner Qi, disperse the perverse wind and heat, strengthen the Qi of auricular region and the vision, relax the tendons and muscles.9–13 SA groups received the same amount of needles at points 1cm away from points used (medially at points GB41, TB5 and LI4 and prior to points ST6 and TB17), outside meridians and superficially, without manifestation of De Qi. The volunteers received ten acupuncture sessions once a week. They were placed comfortably lying on a stretcher in dorsal decubitus and the needles 0,25x30mm. inserted in specific points with perpendicular insertions, remained for thirty minutes. Prior to insertion, the accupoints received antisepsis with 70° alcohol.
All data were submitted to statistical analysis using the Prisma software, version 7, and ANOVA Two Way was performed, with significance level of 5%.
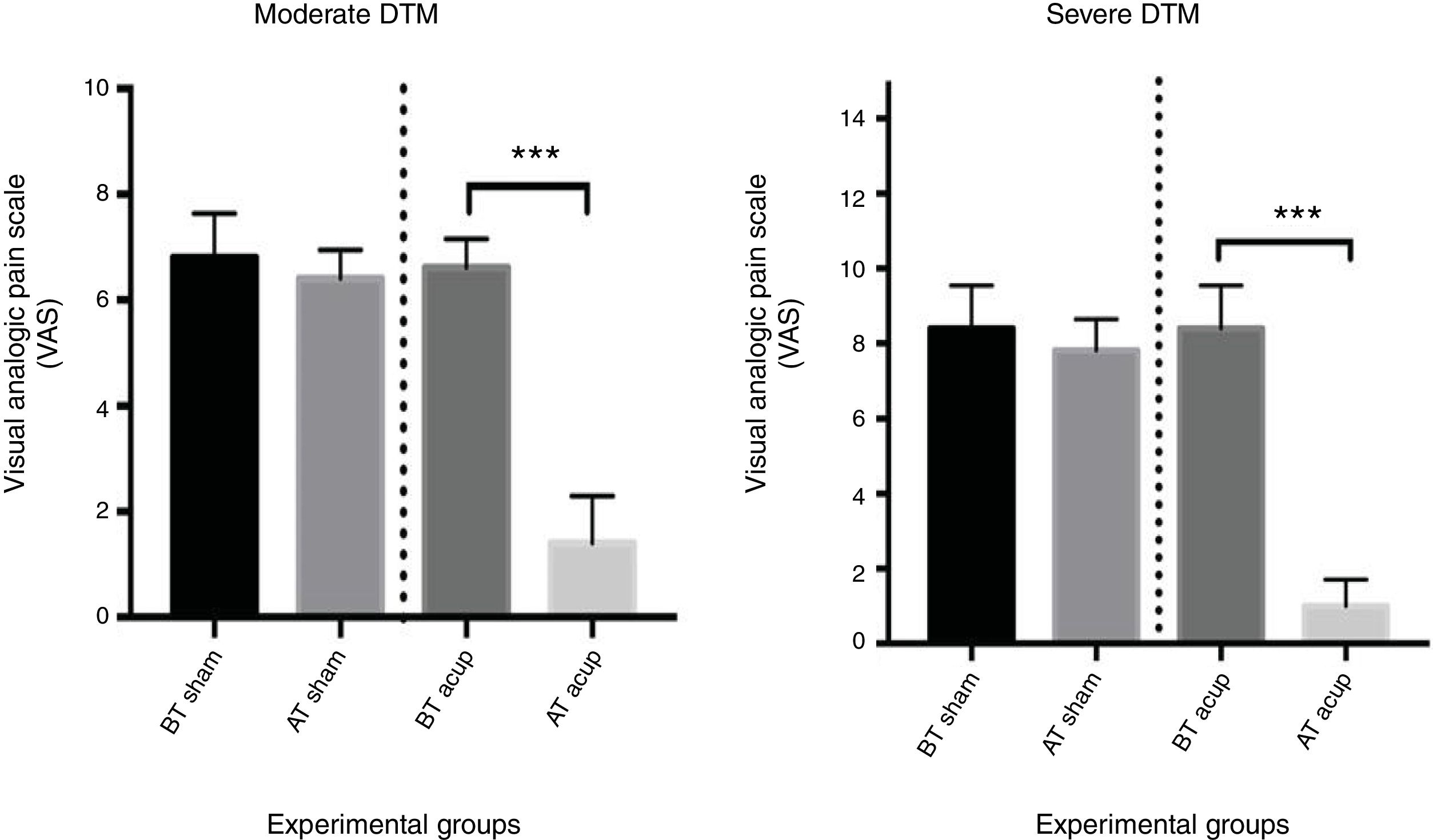
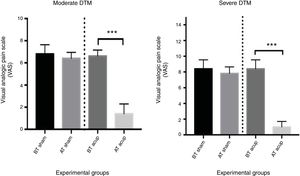
ResultsThe results of work show great efficiency in TMD signs and symptoms control. The Figure 1 show numerical values obtained for quantification of pain when volunteers analyzed visual analogic pain scale (VAS), prior to start of treatment and after end treatment. It can be seen in groups that received Traditional Chinese Acupuncture there was a statistically significant difference in reduction of pain after treatment, which did not occur in groups treated with Sham Acupuncture. It is important to note that the remission of pain occurred in all volunteers of CTA groups, right after first treatment session and decreased with each new session.
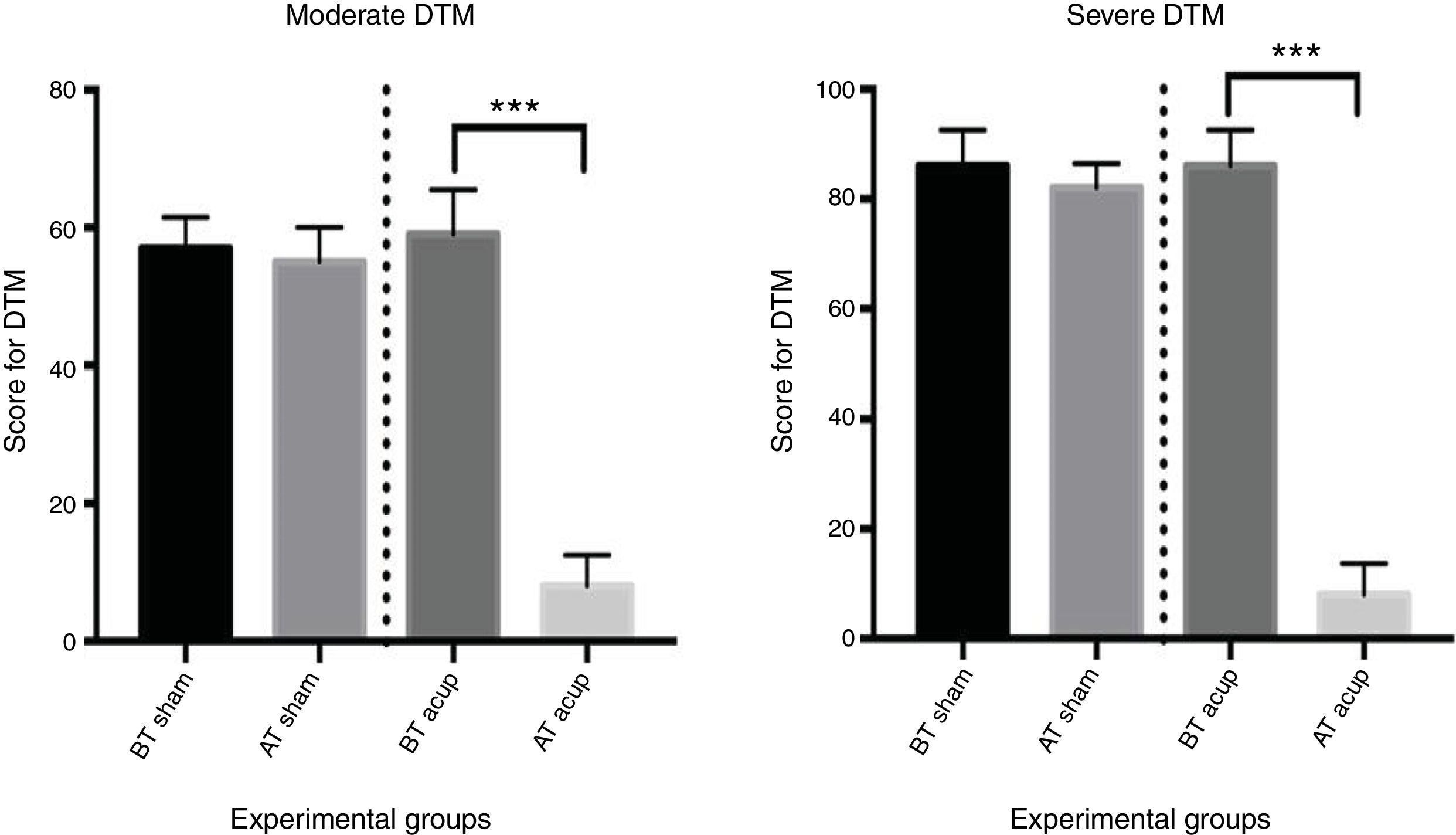
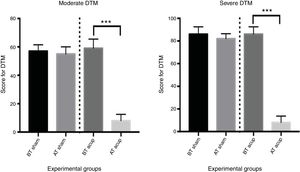
Figure 2 present numerical values obtained when comparing initial and final scores used to classify each volunteer in moderate and severe TMD, before and after Traditional Chinese Acupuncture or Sham acupuncture treatments. It can be clearly seen that in groups that received Traditional Chinese Acupuncture, results are statistically significant (p vaule<0.0001) and, at the end of treatment, none volunteer were considered TMD patients when a new diagnosis was made. In Sham Acupuncture groups, no volunteers had improvement in their TMD score, with values at the end of treatment without statistical differences compared to initial values.
These results show that, even though there was no total remission of pain in analyzed volunteers, all of them, at the end of proposed treatment, presented no TMD according to diagnostic criteria used, revealing that Traditional Chinese Acupuncture was effective in treating this alteration. Figure 3
DiscussionAcupuncture has contributed greatly to dentistry, being applied in conventional way, with manual stimulation of needles, or in modern forms, associated to use of electrical stimulation devices or lasers. Several authors have shown that its efficacy in treatment of craniofacial pain is quite satisfactory and is currently the subject of several studies.17,24,25 This study showed that Acupuncture should not be a simple resource or the patient's last attempts in temporomandibular disorders control, since it was effective in control of this disorder.
The Acupuncture is part of Traditional Chinese Medicine, which is holistic, visualizing the whole patient, namely, an undivided set, composed simultaneously by body, mind, spirit and all its relations with environment in which patient is leased. Rather than treating organs and symptoms, Traditional Chinese Medicine seeks to assess the patient's energy pattern as well as all factors that triggered the disorder and led to onset of a particular organic or emotional dysfunction. Qi energy and all its variations, travels through the body per channels called meridians. Each meridian connects to another through organs (Zang) and energy flows by irrigating and nourishing the human body organs and tissues, thereby causing effective functioning of organism. Involvement of one or some meridians or Zang Fu system generates an energy imbalance and, consequently, disease.9,10,13,26,27
For List & Helkimo 28acupuncture should be used for treatment of any source pain. In orofacial pain arising from temporomandibular disorders, neuralgies, odontogenic pain etc., acupuncture may be palliative, curative or associated with other therapy considered as conventional. This study presented that it was a very useful technique in order to control the volunteer's pain, besides promoting emotional balance, which allowed a functional rearrangement of nervous system and, in turn, allowed a rebalancing of stomatognathic system structures. The treatment of orofacial pain varies according to level of impairment of these structures, with clinical signs and symptoms and the time of disorder installation. It is recommended that treatment should be multidisciplinary, whom may include psychological therapy, physiotherapy, music therapy, acupuncture, among others. The results demonstrate that acupuncture is a technique wich should always be used, since in itself, has already provided quite satisfactory results; so it can be assumed that associated with other techniques, including conventional treatment, the efficiency of therapy would be even better. When Acupuncture is performed, concomitantly with the release of natural opioids, muscle relaxation occurs, thus reducing existing tensions. In this way, it acts in decrease of regional reflex circuits excitability, by activation of afferent neurons and by induction control pain system. This action is clear from numerical values presented in results of this study, with a significant reduction of pain.
The technique, used as complementary therapy in dental treatment, can be used in many situations. Nader,29 Vachiramon et al.,30 Boleta-Ceranto et al.31 show that Acupuncture has been used in dentistry to treat orofacial pains including odontogenic pains; for vomit reflex control, mainly during the moldings and radiographic takes; control of postoperative vomit in patients with general anesthesia for larger oral surgeries; increased anesthetic effect; increased salivary secretion; in therapy for anxious, stressed and phobic dental treatment; in patients with systemic diseases and hypertension, which allows less traumatic care; improvement in hemostasis; treatment of trismus and bruxism; increased immune response; improvement of bone quality; control of postoperative pain; among others. For Hirschfeld,32 Acupuncture can be used as a complement to conventional treatment. As only resource in analgesia for surgical intervention, its value is questionable; however, in control of postoperative pain, TMD and orofacial pain, Acupuncture has a significant additional value to therapeutic arsenal of dentist. The data of this research clearly demonstrate the high efficiency of Acupuncture at control of pain in patients with temporomandibular dysfunction and, certainly, can be a tool that should be used and implemented in dentistry formation, especially to show its action, efficiency and low cost compared to reality of dental offices. Obviously there should be adequate training for professionals to use it as accurately as possible.
It is important to emphasize that Acupuncture does not always have effect, that is, it is not a miracle therapy. Generally, if no significant modification occurs after three to four sessions, the treatment may not be effective. There are at least two reasons for this: some patients fail to acupuncture respond per se, or diagnosis according to Traditional Chinese Medicine precepts was failure. Therefore, treatment duration may vary from case to case for the same disease, since it should be taken into account if acute or chronic disease, and even individual responses different from acupuncture treatment. It is not uncommon, however, that patients to report improvement in first session of acupuncture.13 The results of this study show that all volunteers who received traditional Chinese Acupuncture showed significant improvements, which did not occur in those who were treated with Acupuncture Sham. However, not all showed this improvement in first or second session, but from the fourth session, was reported a significant improvement of all symptoms and signs presented. It is worth noting that use of “Protocol in Acupuncture” is not recommended by Traditional Chinese Medicine, since each individual, on a given day, at a certain time, in a given climate and according to their diet or emotional state, may present interference in results of treatment. Thus, the fact that there is no total remission of signs and symptoms, as observed in results of this study, may be due to these considerations.
Oliveira 33reports the importance of professionals working with patients who present and suffer of stomatognatic system disorders consequences and related structures, also be aware that somatic, psychic and social factors may be altered and compromise the normal sense of well-being. The results of study highlight these statements and show that Acupuncture proved to be a complete tool for treatment of TMD, since the volunteers analyzed had complete dentition with a normal occlusion; thus, the most probable cause of signs and symptoms of DTM in these individuals is related to emotional factors, on this account, as reported in literature, the origin of TMD is multifactorial, always emphasizing, besides physical factors, the emotional ones. As Acupuncture is a technique that treats each individual completely, all causal conditions can be treated simultaneously, obtaining quite considerable results, as presented in this study.
All results allow to suggest that Acupuncture acts positively on functioning of stomatognathic system, altering physiologically the pattern of chewing muscles due to relaxation caused and, probably, than potential bite force, besides considerably reducing the pain symptomatology. All volunteers treated with TCA reported complete physical and mental well-being during treatment, with total remission of pain. However, it is always important to affirm that is necessary to carry out more researchers, in order to reinforce what has been obtained in literature and, especially, to show the durability of this therapy in life of each person.
ConclusionsThe results obtained in this study showed that Acupuncture was effective in controlling and remission of signs and symptoms that characterize temporomandibular dysfunction. All volunteers treated with Traditional Chinese Acupuncture, who presented varying degrees of TMD according to methodology used (moderate or severe), at end of treatment, were considered non-carriers of this disorder, which did not occur with those treated with Sham Acupuncture. However, new studies are suggestive, with same or different protocols, so that the real efficiency of most used technique within the knowledge of Traditional Chinese Medicine, Acupuncture, can be verified.
Conflicts of InterestThe authors declare no conflicts of interest regarding the publication of this paper.