T2 magnetic resonance imaging (T2MR) is a new method for the diagnosis of invasive candidiasis, although most studies have analyzed its role in patients with candidemia or not infection.
Case reportWe present the case of a patient with arteritis and thrombosis of the hepatic graft resulted from an undocumented fungal infection in the explanted liver.T2MR in serum was a suitable diagnostic tool for the diagnosis of the deep-seated invasive candidiasis in the absence of candidemia or the isolation of the yeast in culture.
ConclusionsT2MR allowed the diagnosis of deep-seated invasive candidiasis in an immunodepressed patient without candidemia, even before the onset of symptoms.
La técnica T2 de visualización en resonancia magnética (T2MR, por su abreviatura en inglés) es un método nuevo de diagnóstico de candidiasis invasora, si bien la mayoría de los estudios la ha validado en casos de candidemia o cuando no hay infección.
Caso clínicoSe presenta el caso de una paciente con arteritis y trombosis de la arteria hepática en el injerto secundarias a una infección profunda por Candida en el hígado explantado. La positividad de la técnica T2MR en suero constituyó la única evidencia de infección profunda por Candida en ausencia de candidemia o existencia de la levadura en cultivo.
ConclusionesLa técnica T2MR permitió el diagnóstico de una infección profunda por Candida en una paciente inmunodeprimida en una fase muy precoz de la enfermedad.
Diagnosis of deep-seated invasive candidiasis (IC) in the absence of candidemia is a challenge for clinicians.2 IC remains a leading cause of morbidity and mortality among liver transplant recipients.1 Fungal aneurysms and arteritis are mostly attributable to Candida or Aspergillus species, both of which invade the vascular endothelium, and arteritis cannot be ruled out in the absence of candidemia.5
T2 magnetic resonance imaging (T2MR) for the detection and identification of Candida species is a new method for the diagnosis of IC that has been approved by the US FDA and by the EMEA.4 To date, most studies have analyzed the role of T2MR in patients with candidemia, although information is limited in patients with deep-seated IC.
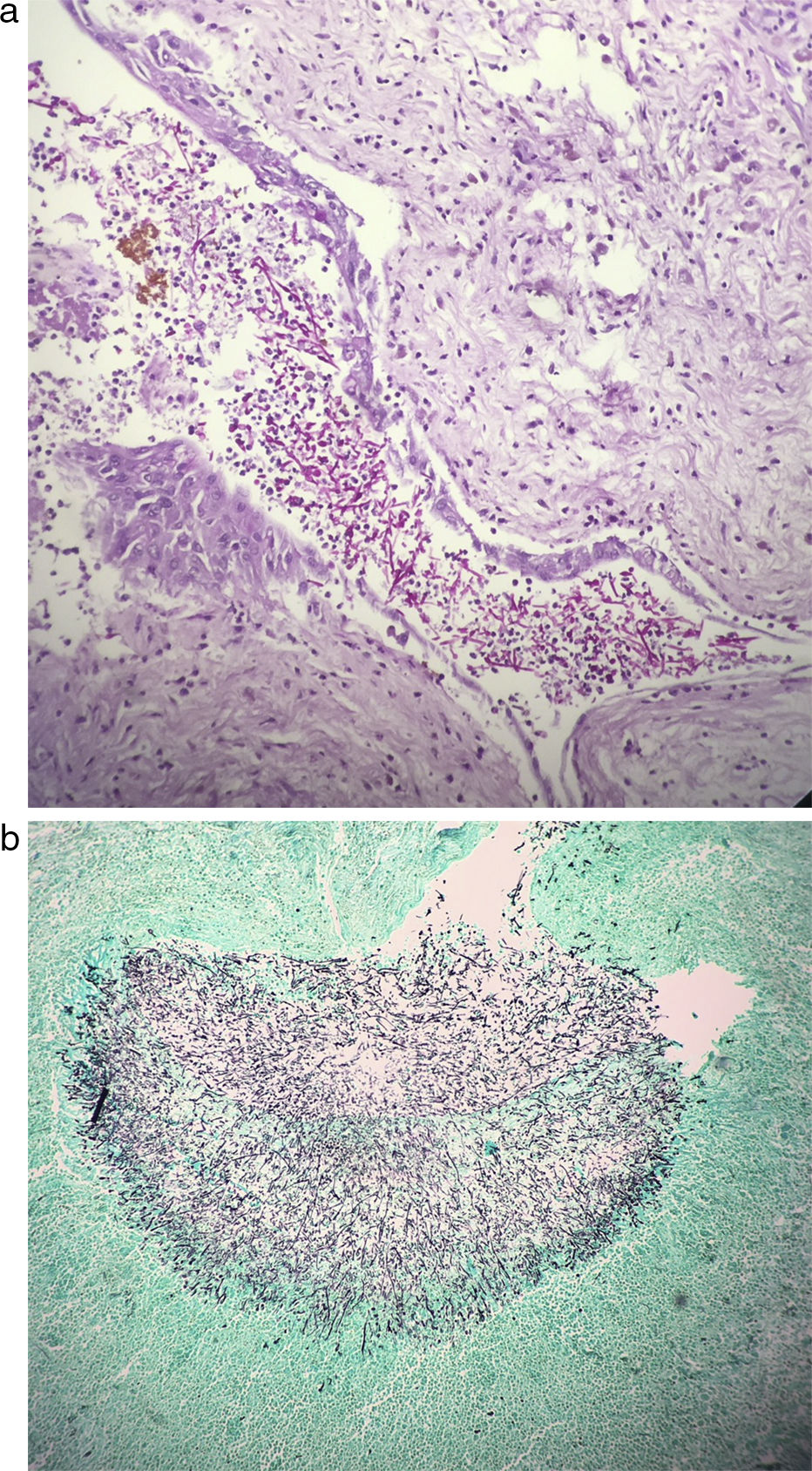
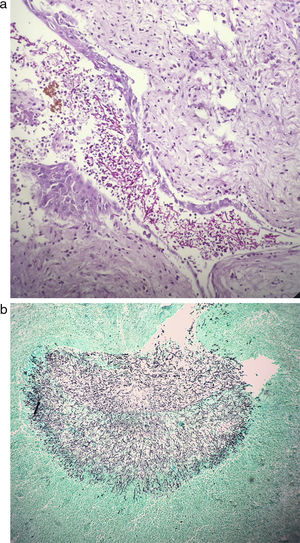
Case reportWe treated a 57 year-old woman with insulin-dependent diabetes mellitus and primary sclerosing cholangitis. Between 2015 and 2017, she had 15 episodes of cholangitis, with bacteremia found in 6 episodes. Liver transplantation was performed on May 9th, 2017, with no complications. No antifungal drug was administered. The patient was discharged without symptoms on May 23rd. On May 27th, the final histological analysis of the explanted liver revealed the presence of a cholangiolitic microabscess with mycotic structures. Blood cultures (2×) were made, even though the patient was asymptomatic. As the latter were negative, further blood samples were obtained for T2MR. In the absence of symptoms, no antifungal or other antimicrobial agents were administered. The patient was readmitted on May 31st with sudden abdominal pain. A computed tomography angiography confirmed the presence of a hyperdense pseudoaneurysm and thrombosis of the hepatic artery, surrounded by a heterogeneous collection causing partial thrombosis of the portal vein. Cultures of blood (2×) and ascitic fluid were negative. Vancomycin, meropenem, caspofungin, and anticoagulants were given, and a hepatic artery stent was successfully placed. On June 15th, an abdominal Doppler ultrasound and a computed tomography scan revealed the preservation of the arterial flow and subtotal thrombosis of the portal vein with filiform passage of the contrast medium, persistence of the organized hematoma, and the presence of three lesions suggestive of intrahepatic abscesses. On June 28th, the patient underwent a second transplant. Non-purulent friable inflammatory tissue was observed in the hepatic hilum, with extensive thrombosis of the portal vein and hepatic artery, and generalized hepatic ischemia. In the following hours, the patient developed graft failure and severe coagulopathy and died. All the cultures made before death, including blood (obtained at admission and repeated 3 times during hospitalization), ascitic fluid at admission, and liver and abdominal tissues during the retransplantation procedure, were sterile. Subsequent T2RM performed on blood samples obtained on May 27th, May 31st, June 9th, June 16th, and June 26th showed amplification of Candida albicans/Candida tropicalis in all samples. Histopathology of explanted liver tissue revealed multiple ischemic areas with abundant filamentous fungal structures in their interior (Fig. 1a, b). C. albicans was amplified using multiplex PCR, even though the cultures from the liver biopsy were sterile.
DiscussionOur two key findings were that arteritis and thrombosis of the hepatic graft resulted from an undocumented fungal infection in the explanted liver and that T2MR was a suitable diagnostic tool for the diagnosis of deep-seated IC in the absence of blood cultures.
In the present case, the arteritis and the abscesses in the hepatic hilum of the graft were similar to those observed in renal transplantation associated with contamination of the preservation fluid. Fungal infections have been less explored in liver transplantation, although hepatic artery aneurysm and Candida peritonitis were recently reported after contamination of the preservation fluid, with a mortality rate of 62.5%.6
As for T2MR, we believe that the results are very significant. All the determinations revealed amplification of C. albicans/C. tropicalis, even at the beginning of the process when the patient was asymptomatic. T2MR is a new, fully automated nano-diagnostic technology that can detect molecular targets of Candida species in whole blood specimens, without the need for prior isolation.3 Data from a recent cohort study show an overall specificity of 99.4% and sensitivity of 91.1%.4 The technique detected the five most frequent species involved in IC, which were coupled according to their resistance patterns—C. albicans, C. tropicalis, Candida krusei/Candida glabrata, and Candida parapsilosis—with results available within 4h.
In conclusion, this case highlights the potential advantage of T2MR in the diagnosis of deep-seated IC in an immunodepressed patient without candidemia, even before the onset of symptoms. This experience and the high specificity and positive predictive value obtained in other studies are encouraging.
FundingThis study was co-funded by the European Regional Development Fund (A Way to Achieve Europe program; Spanish Network for Research in Infectious Diseases, REIPI: Red Española de Investigación en Patología Infecciosa).
Conflict of interestNothing to declare.
We thank Tomas O’Boyle for his excellent technical assistance.