Candidemia is a life-threatening fungal infection characterized by the presence of Candida in the blood.
AimsTo describe the clinical–epidemiological features and main risk factors among patients with candidemia admitted to Intensive Care Unit.
MethodsA cross-sectional, retrospective and observational study was performed between January 2015 and July 2016. Laboratory reports and medical records from ICU patients admitted to a public hospital in northeastern Brazil were analyzed.
ResultsThere were 1573 admissions and 67 of them were positive for candidemia. The majority of patients were male (53.3%) and remained at the hospital for more than seven days (86.6%). Non-C. albicansCandida infections (60%) were predominant. Broad-spectrum antibiotic therapy was prescribed in 98.4% of the cases. The most frequent underlying diseases were sepsis (73.3%), presence of solid tumors (15%), respiratory condition (60%), urinary tract disease (56.6%) and gastrointestinal tract diseases (23.3%). Surgeries were carried out on 43% of the patients, consisting of 23.3% abdominal surgeries, with a mortality rate of 92.8%. Risk factors were venous central access (93.3%), mechanical ventilation (81.6%), nasoenteral tube (83.3%), nasogastric tube (25%), indwelling bladder catheter (88.3%), diabetes mellitus (55%) and tracheostomy (36.6%). Statistical analysis correlated the use of indwelling bladder catheter with a higher mortality rate (r=0.07412, p=0.0353).
ConclusionsThe current study reveals the high case fatality rates among critically ill patients suffering from candidemia admitted to ICU. Herein, we highlight the importance of identifying non-C. albicansCandida species and reinforce the idea of carrying out epidemiological surveillances and antifungal susceptibility tests.
La candidemia es una infección potencialmente fatal caracterizada por la presencia de Candida en la sangre.
ObjetivosDescribir las características clínico-epidemiológicas y los principales factores de riesgo en pacientes con candidemia ingresados en la unidad de cuidados intensivos (UCI).
MétodosEntre enero de 2015 y julio de 2016 se llevó a cabo un estudio transversal, retrospectivo y observacional en el que se analizaron los registros médicos e informes de laboratorio de pacientes de la UCI de un hospital público del noreste de Brasil.
ResultadosEntre las 1.573 admisiones registradas hubo 67 diagnósticos de candidemia. La mayoría de los pacientes fueron del sexo masculino (53,3%) y la permanencia en el hospital fue superior a siete días (86,6%). Las infecciones por especies de Candida no-C. albicans fueron el 60% de los casos. En el 98,4% de los casos se prescribió antibioterapia de amplio espectro. Las enfermedades de base más frecuentes fueron la sepsis (73,3%), la presencia de tumores sólidos (15%), las enfermedades respiratorias (60%), la enfermedad del tracto urinario (56,6%) y las enfermedades del tracto gastrointestinal (23,3%). Se realizaron cirugías en el 43% de los pacientes, siendo el 23,3% cirugías abdominales, con una tasa de mortalidad del 92,8%. Los factores de riesgo fueron la existencia de un acceso venoso central (93,3%), ventilación mecánica (81,6%), sonda nasoenteral (83,3%), sonda nasogástrica (25%), catéter vesical permanente (88,3%), diabetes mellitus (55%) y traqueostomía (36,6%). Los análisis estadísticos correlacionaron el uso del catéter urinario permanente con una mayor mortalidad (r=0,07412; p=0,0353).
ConclusionesEste estudio muestra las elevadas tasas de letalidad asociadas a pacientes con candidemia ingresados en la UCI. Destacamos la creciente importancia de identificar las especies de Candida diferentes de C. albicans, y reforzamos la idea de llevar a cabo una vigilancia epidemiológica y de realizar pruebas de sensibilidad a los antifúngicos.
Candidemia is a life-threatening fungal infection whose incidence has significantly increased in recent years; it is associated with prolonged hospital stays, which increases hospital costs, and is responsible for high morbidity and mortality rates among critically ill patients.13 Candidemia accounts for almost 80% of all hospital related fungal infections1,24 and Candida is the fourth most common isolated pathogen that leads to nosocomial sepsis in adults and the third most common among neonates.3,27 Mortality rates of candidemia reach from 54% to 72%5,7 and its incidence in Brazil is 2.49 per 1000 hospital admissions.8,23 Around 38% of all fungal-based hospital infections are diagnosed in Intensive Care Unit (ICU) patients as they are in a higher risk condition, in need of higher level of care and in need of more invasive procedures.10,15,22,23 The main risk factors associated are the use of broad-spectrum antibiotics, prolonged hospital stays, neutropenia, parenteral nutrition, bladder catheter, central venous catheter, mechanical ventilation, and colonization of multiple anatomical sites by yeasts. Higher rates of fungemia can be found in infants with less than one year, and in the elderly over 65 years.9,12,22,25
There are few studies on the epidemiology of candidemia in Latin America and Brazil, whereas it has been well documented in the countries of the Northern Hemisphere.23 In the Northeast region of Brazil, the matter becomes even more alarming as there are only four studies published3,15,16,21 on the subject and none whatsoever approaches its characteristics in critically ill patients. Considering the high mortality rate and high estimated hospital costs, all the knowledge on the incidence, the risk factors, and the Candida species involved together with the sensitivity antifungal profile of the isolates recovered in this population, become extremely important, especially when aiming toward the control and management of this disease.
Materials and methodsType of studyA retrospective study with observational prospective approach was developed in the period between January 2015 and July 2016, involving either the cases of candidemia (diagnosed by blood culture carried out in a microbiology laboratory hired by the Regional Health authority), and critically ill patients’ medical records. The patients had been hospitalized in an ICU of a tertiary public hospital in Northeastern Brazil.
Site of study and target populationThe study took place in the ICU of a tertiary public hospital attending trauma patients, general admissions, orthopedic traumas with surgery and medical clinic admissions. The ICU ward counted 30 beds: 20 for general ICU admissions and 10 for surgical ICU admissions. Critically ill adult patients over 18 years old admitted to the ICU with symptoms and signs of infection, along with a positive result for candidemia, were included in the study. According to hospital protocols, patients with leukocytosis or leukopenia, tachycardia and tachypnea, fever or hypothermia and an increase of 2 or more points on SOFA – Sequential Organ Failure Assessment Score, were considered potentially infected. Patients having vasoactive drugs to maintain an average blood pressure higher than 65mmHg and hyperlactatemia (lactate >2mmol/l) were considered to be under septic shock. Patients with incomplete clinical, laboratorial or epidemiologic data were excluded.
Data collectionProfessionals of the institution, as requested by the medical staff and following the protocols of the laboratory, collected the blood samples. The identification of the isolates was done through an automatic system with the Walk-Away™ device.
Any isolation of Candida in the blood culture of a patient with signs and symptoms of infection, such as fever, tachycardia, hypotension and tachypnea, was considered diagnostic of candidemia. If a subsequent blood culture of the same patient was positive to any species of Candida up until 30 days after the first sample collection, it was considered the same candidemia episode; if the isolation in the blood culture occurred after 30 days, it was considered a new episode.15,23 Data on patients’ evolution and their clinical information was followed up until they were discharged, referred to another unit or declared deceased. The following variables were noted: age, gender, length of stay, underlying diseases, performed invasive procedures (minor or major surgery, orotracheal intubation, introduction of catheters, etc.), antibacterial drug treatment, use of antifungals, fungal specimens isolated and the presence of other microorganisms. The risk factors analyzed were the presence of central venous catheters, mechanical ventilation, previous broad spectrum antibiotic usage, parenteral nutrition, indwelling bladder catheters, corticotherapy, previous surgery (and if it was abdominal or not), hemodialysis, risky ages (less than one year old or higher than 65 years old), prolonged hospital stays (equal to or longer than 7 days), hematological or oncological disease, diabetes mellitus, presence and duration of neutropenia, chemotherapy or radiotherapy and immunosuppression. Only conditions presented up to 30 days before the infection occurred were considered as risk conditions for candidemia. Data on mortality, the cumulative incidence and the Candida albicans and non-C. albicans distribution were filed.
According to the service protocol, the Sevilla Score was used for the risk presumption of candidemia. This score evaluates the colonization sites, health condition at the moment of hospitalization and the clinical status of the patient. Patients showing moderate or severe risk (score >8) would start an antifungal treatment.
Statistical analysesThe frequency of risk factors was calculated with the ratio of the number of exposed patients to the referred variable and the total number of included patients. The mortality rate was calculated with the ratio between number of deaths and the total number of included patients. The cumulative incidence was calculated with the ratio of candidemia episodes per thousand ICU admissions.
The Spearman correlation test was used to observe the correlation between each of the predisposing factors and death, considering p≤0.05 as statistically significant.6 All statistical analyses were created with Graphpad Prism version 5.01.
Ethical research aspectsThis study was approved by the Human Research Ethics Committee of the Health Sciences Centre (CCS) of the Federal University of Pernambuco (UFPE) under CAAE number 01847812.0.0000.5208, following the ethical principles established under the resolution 466/12 of the National Council of Health (CNS). All data were collected and filed after CPE approval. All the information was used exclusively in the present study, and the individuals’ identities were maintained under absolute secrecy.
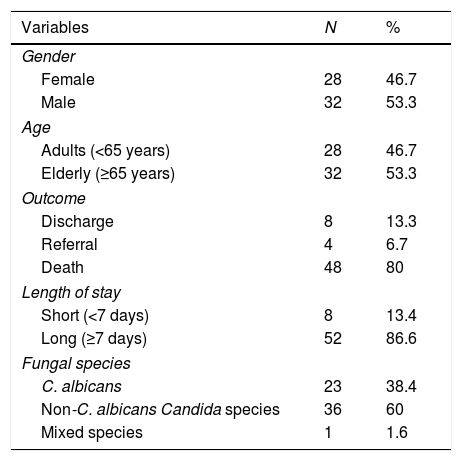
ResultsBetween January 2015 and July 2016, 1573 patients were admitted to the ICU of the Health Unit and 4129 blood cultures were performed, being 67 (1.6%) of them positive for Candida. The candidemia cumulative incidence was 42.59 cases per 1000 ICU admissions. Despite a total of 67 Candida-positive blood cultures were used to calculate the cumulative incidence, only 60 episodes of candidemia were used to describe clinical–epidemiological features of patients and their risk factors. Seven patients were excluded for having incomplete data in their medical records. The average age of the sample population was 64.4 (±18.7) years old, with a median of 67 years old. Thirty-two (53.3%) of these patients were males and twenty-eight (46.7%) were females. Fifty-two (86.6%) of them were hospitalized for a long period, the average hospitalization length being 31.7 days. Table 1 summarizes the epidemiological characteristics of the studied sample. Among the isolated yeasts, non-C. albicansCandida species were present in 36 (60%) cases and C. albicans in 23 (38.4%). The blood culture of one patient (1.6%) yielded both C. albicans and another species of the genus.
Clinical–epidemiological characteristics of ICU patients with candidemia diagnosed by blood culture.
| Variables | N | % |
|---|---|---|
| Gender | ||
| Female | 28 | 46.7 |
| Male | 32 | 53.3 |
| Age | ||
| Adults (<65 years) | 28 | 46.7 |
| Elderly (≥65 years) | 32 | 53.3 |
| Outcome | ||
| Discharge | 8 | 13.3 |
| Referral | 4 | 6.7 |
| Death | 48 | 80 |
| Length of stay | ||
| Short (<7 days) | 8 | 13.4 |
| Long (≥7 days) | 52 | 86.6 |
| Fungal species | ||
| C. albicans | 23 | 38.4 |
| Non-C. albicans Candida species | 36 | 60 |
| Mixed species | 1 | 1.6 |
Death was the main outcome occurring in 48 (80%) of the cases. Eight (13.3%) patients were discharged and 4 (6.7%) were referred to other Health Units. Mortality figures were similar when comparing patients with C. albicans infection (82.6%; 19/23) and those infected with other species of the genus (81.9%; 30/37). The isolation of other microorganisms different from Candida was registered in the blood culture of 58.3% of the patients. Only one (1.6%) of the patients was not on broad-spectrum antibiotic therapy, but was having an antifungal therapy. Forty nine (83%) patients among the 59 on broad-spectrum were taking three or more types of antibiotics. Antifungal drugs were administered to 29 (48.3%) of the patients. Those drugs included fluconazole, which was used in 10 (34.4%) of the cases, followed by micafungin (9 cases; 31%) and amphotericin B (3 cases; 10.3%). Corticotherapy was prescribed in 31 (51.6%) of the patients during their ICU stay.
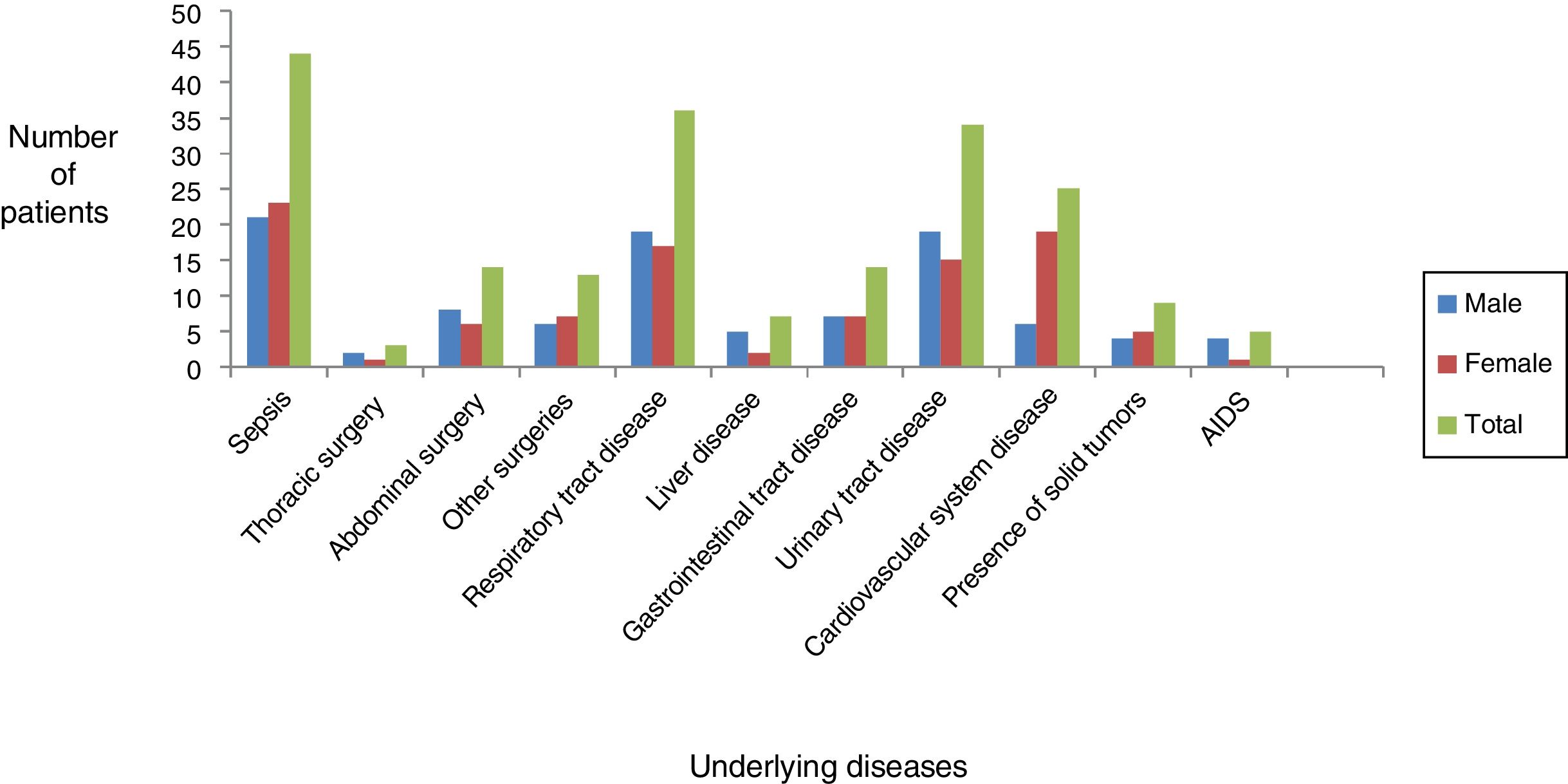
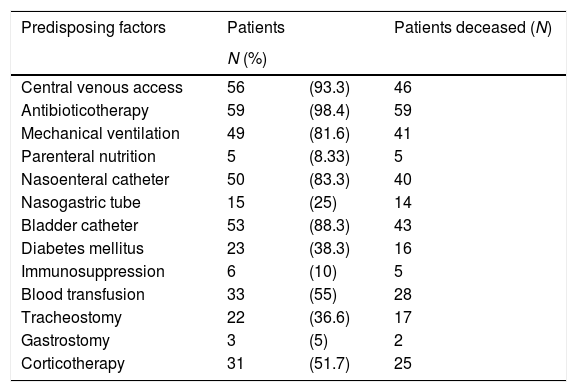
Sepsis, respiratory diseases and urinary tract diseases were the most common diagnoses, as shown in Fig. 1. Sepsis was diagnosed in 44 (73.3%) patients, 36 (60%) patients had respiratory diseases as underlying disease and 34 (23.33%) had urinary tract diseases (urinary infection or renal insufficiency). Thirty six (60%) patients required hemodialysis during hospitalization. Other underlying diseases observed were the presence of solid tumors in 9 (15%) of the patients, gastrointestinal tract diseases in 14 (23.33%), liver diseases in 7 (11.66%) and acquired immune deficiency syndrome – AIDS in 5 (8.33%). Cardiovascular comorbidities were present in 25 (41.66%) of the cases. During their ICU stay, 30 (43.33%) patients underwent some type of surgical procedure. Abdominal surgery, the main one and most major type of surgery, was performed on 14 (23.33%) patients; 3 (5%) patients underwent thoracic surgery, and 13 (21.66%) other patients were submitted to minor surgery. There was evidence of a high mortality rate, 92% (13/14), among the patients submitted to abdominal surgery. Table 2 shows the other risk factors that can be found; the most prevalent ones were central venous access in 56 (93.3%) of the patients, mechanical ventilation in 49 (81.6%), nasoenteral tube in 50 (83.3%), nasogastric tube in 15 (25%), indwelling bladder catheter in 53 (88.3%), diabetes in 23 (38.3%), blood transfusion in 33 (55%) and tracheostomy in 22 (36.6%). According to the predisposing factors analyzed there is a positive correlation between the use of indwelling bladder catheter and death (r=0.07412, p=0.00353), as evidenced in Table 2.
Risk factors and number of deaths among ICU patients with candidemia.
| Predisposing factors | Patients | Patients deceased (N) | |
|---|---|---|---|
| N (%) | |||
| Central venous access | 56 | (93.3) | 46 |
| Antibioticotherapy | 59 | (98.4) | 59 |
| Mechanical ventilation | 49 | (81.6) | 41 |
| Parenteral nutrition | 5 | (8.33) | 5 |
| Nasoenteral catheter | 50 | (83.3) | 40 |
| Nasogastric tube | 15 | (25) | 14 |
| Bladder catheter | 53 | (88.3) | 43 |
| Diabetes mellitus | 23 | (38.3) | 16 |
| Immunosuppression | 6 | (10) | 5 |
| Blood transfusion | 33 | (55) | 28 |
| Tracheostomy | 22 | (36.6) | 17 |
| Gastrostomy | 3 | (5) | 2 |
| Corticotherapy | 31 | (51.7) | 25 |
Candida infections have increased significantly in recent decades, then rising the morbidity and mortality in critically ill patients, as well as hospital costs. Adequate treatment for candidemia is estimated to increase total hospital costs by up to US$40,000 and extends the hospitalization period from 3 to 13 days.14
Sixty-seven cases of candidemia were registered with a cumulative incidence of 42.59 cases per 1000 ICU admissions. In a multicentric study of 712 candidemia cases in 11 different public health services centers in Brazil, by Colombo et al., an incidence of 2.49 cases per 1000 hospital admissions was found.8 With an incidence rate that is 17 times higher, our study draws attention to the prevalence of candidemia cases in critically ill patients.
The main etiological agent of candidemia worldwide is C. albicans. In the Northeast region of Brazil, the higher prevalence of other species of the genus was evidenced in studies by Hinrichsen,15,16 demonstrating that C. parapsilosis was more predominant in private hospitals. Results showed the predominance of other species different from C. albicans (37 of the cases, 60%), which can be related to the higher severity status of critically ill patients that are submitted to a greater number of invasive procedures as well as to prophylactic or empirical antifungal treatments.11,17 Bassetti et al.4 have reported a rise around 50% in the incidence of candidemia due to non-C. albicansCandida species in critically ill patients. To establish proper treatments to improve patients’ condition, it is essential to identify the species.29 In our study, the systematic identification of non-C. albicans Candida species was not done by the outsourced microbiology's support laboratory.
The infection may be endogenous, due to gastrointestinal tract or mucocutaneous colonization, or exogenous, through health workers, medical objects or infected infusions, among others.12 The correct identification of the Candida species involved in the infection episode may reveal the source, leading to the implementation of different strategies and approaches to control the infection.
A large number of studies in Brazil showed a mortality rate of 54–72% in patients with candidemia.5,21 These figures might be higher considering only critically ill patients. In a study with 2362 patients, where 63 critically ill patients had 77 candidemia episodes, Karacaer et al. observed a 78% mortality rate.18 Patients who underwent abdominal surgery had a 92.8% (13 patients out of 14) mortality rate. It is important to highlight that the mortality rate was higher among the patients infected with C. albicans, whereas Azoulay et al.2 and Larrondo et al.19 observed a higher mortality rate among the patients infected with other species of Candida; this fact could be attributed to the rise of resistance to the commonly used antifungal drugs in the ICU.2,19
Hospitalization length, ICU admission and age are predisposing factors for candidemia as described in the support literature.8 In our study, more than 50% of the patients were older than 65 years and stayed in the ICU for a long period (>7 days). Among them, 8 (13.3%) patients remained in the ICU from 7 to 15 days, and 41 (68.3%) for more than 15 days. Almost all the patients (59/60) were on broad-spectrum antibiotic therapy, from whom 49 (83%) had three or more antibiotic schemes before taking antifungal drugs. Most of the patients were on corticosteroids. Data suggest that broad-spectrum antibiotic therapies, as well as corticosteroids, are risk factors for associated opportunistic infections. No reference score, as the Sevilla score or any other score instituted by the Health Unit, seemed to be used for monitoring the critically ill patients under suspicion of Candida invasive infection. This tool determines, through the analysis of the medical condition of the patients, the susceptibility to acquire candidemia, establishing a score that rises from asymptomatic patients to those in septic shock.20,28
Sepsis, respiratory and urinary tract diseases were the most common diagnoses among men and women. Other publications show the importance of Candida as a cause of septicemia.1 Our results agree with those in the published literature, suggesting that sepsis, respiratory and urinary tract diseases, abdominal surgery and the presence of solid tumors are the most common diagnoses among patients with an invasive Candida infection.2,28 As shown in previous studies, the use of central venous catheters, indwelling bladder catheters and mechanical ventilation were the most prevalent risk factors, observed in 93.3%, 88.3% and 81.6% of the patients, respectively. The small number of patients under parenteral nutrition stands out as we observed a disagreement with literature data concerning certain risk factors.9,12,22,25 However, results suggest that the presence of other catheters, such as nasoenteral and nasogastric tubes and tracheostomy, as well as blood transfusions, were relevant risk factors. These data may be explained by the fact that catheters are invasive devices which predispose to infections and the formation of microbial biofilms.26 Indwelling bladder catheters, which were used in 88.3% of the cases, were the only risk factor with a positive and significant correlation with the death of the patients (p=0.0353). It is well known that the use of catheters increases the risk of urinary tract infections, and the development of biofilm decreases the drug's effect, thus making the patient more vulnerable to urosepsis and death.
Appropriate diagnosis and treatment of the infection through health care assistance remains a challenge. Adequate interaction between ICU multidisciplinary teams, infection control team and the laboratory of microbiology, associated to an assertive pondering of the risk factors and the severity of each case, raise suspicions and leads to a better clinical diagnosis. It must be highlighted that laboratorial support investment to encompass Candida specimen identification along with its sensitivity profile to the available antifungal drugs is necessary. Additionally, the health staff's awareness and the implementation of measures that allow the monitoring of critically ill patients during their entire hospitalization period are essential for a more favorable clinical outcome.
Conflict of interestsThe authors declare no conflict of interest.
This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) by research grant number 455745/2014-5.