The inappropriate use of antifungals is an important health problem related to increasing adverse effects, unnecessary cost and promotion of resistant and emerging fungal infections. Despite its relevance, many health institutions assign few resources to improve prescribing practices.
AimsTo evaluate the efficiency of an antifungal stewardship programme (ASP) centered on restricted antifungal agents.
MethodsThe main activity during the eight-month study was to perform a programmed review of restricted antifungals (lipid formulations of amphotericin B, echinocandins and voriconazole) prescribed in hospitalized patients. In the case of amendable antifungal treatment, a recommendation was included in the electronic medical record.
ResultsA total of 280 antifungal prescriptions for 262 patients were revised during the study period. The indications were prophylactic in 85 cases (30.4%), pre-emptive in 10 cases (3.5%), empiric in 122 cases (43.6%), and directed in 63 cases (22.5%). A total of 70 prescriptions (25%) in 61 patients were considered to be amendable. In most of these cases, treatment could have been reduced considering the patient's clinical improvement and microbiological results. The most common advice was antifungals change (70%), antifungal withdrawal (21%), removal of one antifungal drug in cases of combined therapy (7%), and switching to oral route (1%). Proposed recommendations were addressed in 28 cases (40%). There was no significant difference in adherence with respect to the type of recommendation (p=0.554). There was a 42% lower use of antifungals during the period of the study compared to that observed during a similar previous period. Mortality among patients who were treated according to the recommendations of the ASP was 17% and in whom treatment was not modified it was 30% (p=0.393).
ConclusionsASPs centered on hospitalized patients may be an efficient strategy to ameliorate antifungal use in hospitals.
El uso inadecuado de los antifúngicos es un problema de salud relevante que puede incrementar los efectos adversos y generar costes innecesarios, además de favorecer la aparición de resistencias y de infecciones micóticas emergentes. A pesar de su importancia, muchas instituciones sanitarias destinan escasos recursos para mejorar las prácticas de prescripción.
ObjetivosEvaluar la eficiencia de un programa de asesoramiento sobre antifúngicos basado en la prescripción de agentes antifúngicos restringidos.
MétodosLa principal actividad durante el estudio de ocho meses de duración fue la realización de una revisión programada de antifúngicos restringidos, prescritos en los pacientes hospitalizados (formulaciones lipídicas de anfotericina B, equinocandinas y voriconazol). En el caso del tratamiento antifúngico modificable, se procedió a anotar una recomendación en la historia clínica electrónica.
ResultadosSe revisó un total de 280 prescripciones de antifúngicos en 262 pacientes durante el período de estudio. Las indicaciones fueron de tipo profiláctico en 85 casos (30,4%), anticipado en 10 (3,5%), empírico en 122 (43,6%) y dirigido en 63 (22,5%). Se consideraron modificables un total de 70 prescripciones (25%) en 61 pacientes. En la mayoría de estos casos, el tratamiento podía reducirse teniendo en cuenta la mejoría clínica y los resultados microbiológicos del paciente. La indicación más frecuentemente realizada fue el cambio de antifúngico (70%), seguido por la retirada de dicho fármaco (21%), la eliminación de uno de los fármacos antifúngicos en casos de tratamiento combinado (7%) y, finalmente, la sustitución del tratamiento por la administración oral (1%). Las recomendaciones propuestas se aceptaron en 28 casos (40%). No se produjo una diferencia significativa en la adherencia con respecto al tipo de recomendación (p=0,554). Durante el período de estudio se evidenció un descenso en el uso de antifúngicos del 42%, en comparación con el uso observado en un período previo similar. La mortalidad de los pacientes que fueron tratados de acuerdo con las recomendaciones fue del 17%, y del 30% en aquellos en los que no se modificó el tratamiento (p=0,393).
ConclusionesEl programa de asesoramiento sobre los antifúngicos prescritos en pacientes hospitalizados puede resultar una estrategia eficaz para mejorar el uso de estos fármacos.
Invasive fungal infections (IFI) are a major cause of morbidity and mortality in hospitalized patients in many countries worldwide.4,9 The prompt initiation of effective antifungal therapy reduces patient mortality.2 The poor prognosis associated with IFI combined with suboptimal diagnostic tools has driven the overuse of antifungal drugs which account for an important and increasing part of the cost of drugs for inpatients.2,20,24 Inappropriate use of antifungals also contributes to the global increase in antifungal resistance and the incidence of IFI due to emerging fungi.3,10,16
According to previous studies, most inappropriate antifungal prescriptions are due to difficulties in distinguishing between colonization and infection, little knowledge of the local rate of fluconazole resistance, limited awareness of the first line of treatment for IFI, low switching from intravenous to oral antifungal administration, no adjustment after microbiological results, and excessive length of therapy.27,30,34,35 Among the strategies to improve this situation the use of new technology for a rapid identification of fungal species must be highlighted.1
The important role of antifungal agents in the management of IFIs along with the high costs and their recognized toxicities has been addressed as the principal justification for antifungal stewardship.3,10,16 However, antifungal stewardship has received very little attention in comparison with antibiotic stewardship.35 It should be noted that the antifungal stewardship programmes (ASP) conducted to date have promoted a reduction in spending on antifungal drugs but not in mortality.20,27
The aim of this study was to determine the usefulness of an ASP programme in a tertiary hospital with a high number of hematological and solid organ transplantation patients.
MethodsBetween 1st October 2012 and 31st May 2013, a prospective study was carried out in the Hospital Puerta de Hierro, Madrid, a tertiary university hospital with 600 beds that includes a surgical ICU (20 beds), medical ICU (20 beds) and an active solid organ and hematopoietic stem cell transplantation programme. Electronic medical records are available; they contain computerized prescriptions and progress notes made by physicians. The Local Hospital Infections Committee created a team responsible for implementing the programme. The team was coordinated by two infectious diseases (ID) specialists, and included a pharmacist, a pharmacologist, a preventive medicine specialist and a microbiologist.
The study protocol was approved by the Local Ethics Committee. Requirements for patients’ informed consent were waived because the study was directed at attending physicians with the primary objective of assessing their adherence to ID recommendations entered in the patients’ electronic record. The aim of the programme was presented and discussed in the hospital's main departments during clinical meetings between staff and internal medicine residents.
During this eight-month study the main activity was to perform a programmed review of antifungals prescriptions in hospitalized patients. This review was carried out by two ID specialists together with an internal medicine resident. A list of patients who were prescribed an antifungal considered restricted was provided by the hospital pharmacy department. Lipid formulations of amphotericin B, echinocandins and voriconazole were considered restricted antifungals. Posaconazole was not included in the study because its use was specifically restricted to prophylactic indications in hematologic patients. In the case of patients who were prescribed inadequate systemic antifungal treatments, a recommendation was included in the electronic medical record during the first working day. In most cases, there were neither direct interviews with the prescribing doctor nor patient examinations. On average, the physicians responsible for reviewing the patients (two ID specialists) devoted approximately one hour per day to this activity. Patients could be included more than once if they received any antifungal several times during the study period. Fungal infections in study patients were classified as possible, probable or proven according to recent European Organization for Research and Treatment of Cancer criteria.7 Antifungal prescriptions were regarded as amendable if they were not considered clinically justified and/or did not follow local, national or international guidelines.12,15,24,32 The identification of fungal species was performed by conventional cultures, implementing special techniques when necessary.6 Antifungal susceptibility testing was performed on the isolates according to the microdilution broth procedures CLSI M27-A3 and EUCAST.26
Special care was taken to neither criticize nor discredit current antifungal prescriptions due to the fact that several suitable options to treat the infections may exist, and also because the judgement of the investigators could not take into account certain patient characteristics only known by the treating clinicians.
The record was reviewed again one week later in order to establish whether or not the prescribing physician had adhered to each recommendation. The physician was considered to have followed the recommendation if the appropriate modification had been made within 24h of the advice being given. The clinical records were reviewed six weeks later to assess complications and mortality. The quantities of the antifungals administered were recorded using defined daily doses (DDD).
Paired categorical and continuous variables were compared using the chi-squared test and Mann–Whitney U-test, respectively. Significance was set at p<0.05.
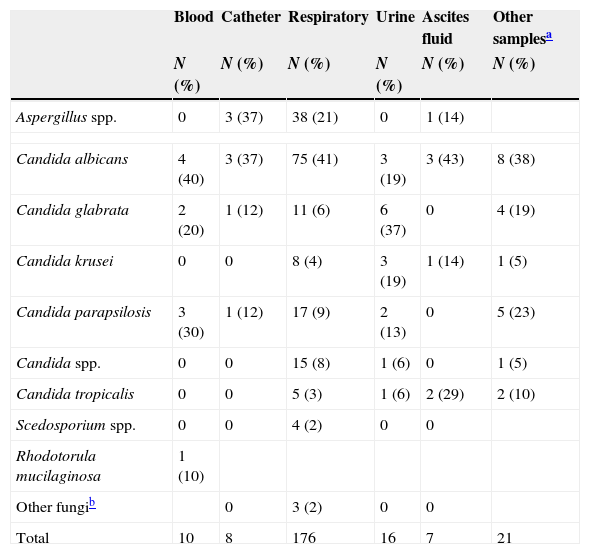
ResultsDuring the study period 280 restricted antifungals were prescribed for 262 patients. In 19 cases the patients were receiving two antifungal drugs (combined treatment). Mean age was 55 (±14) years and 101 patients (65%) were male. The mean hospital stay was 39.6 (±31.7) days. The indications for antifungal prescriptions were prophylactic in 85 cases (30.4%), pre-emptive in 10 cases (3.5%), empiric in 122 cases (43.6%), and directed in 63 cases (22.5%). Among this last group, 27 prescriptions (43%) corresponded to proven IFI (43%), 24 prescriptions (38%) to probable infection and 16 prescriptions (25%) to possible infection. Candida species were the most frequently isolated fungi followed by Aspergillus spp. (Table 1). Ten percent of the yeasts isolated were resistant to fluconazole: Candida krusei, 13 strains (100%), Candida glabrata, 4 strains (17%) and Rhodotorula spp., 2 strains (100%). Among those patients with Candida spp. in respiratory samples (129 cases), 19 patients (15%) received prophylactic treatment, 69 patients (53%) received empirical treatment, and 23 patients (18%) received a treatment directed against those fungal isolates from other samples. There were 18 cases (14%) that received inappropriate treatment, based only on yeast respiratory isolation.
Isolated fungi in microbiological samples.
| Blood | Catheter | Respiratory | Urine | Ascites fluid | Other samplesa | |
|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Aspergillus spp. | 0 | 3 (37) | 38 (21) | 0 | 1 (14) | |
| Candida albicans | 4 (40) | 3 (37) | 75 (41) | 3 (19) | 3 (43) | 8 (38) |
| Candida glabrata | 2 (20) | 1 (12) | 11 (6) | 6 (37) | 0 | 4 (19) |
| Candida krusei | 0 | 0 | 8 (4) | 3 (19) | 1 (14) | 1 (5) |
| Candida parapsilosis | 3 (30) | 1 (12) | 17 (9) | 2 (13) | 0 | 5 (23) |
| Candida spp. | 0 | 0 | 15 (8) | 1 (6) | 0 | 1 (5) |
| Candida tropicalis | 0 | 0 | 5 (3) | 1 (6) | 2 (29) | 2 (10) |
| Scedosporium spp. | 0 | 0 | 4 (2) | 0 | 0 | |
| Rhodotorula mucilaginosa | 1 (10) | |||||
| Other fungib | 0 | 3 (2) | 0 | 0 | ||
| Total | 10 | 8 | 176 | 16 | 7 | 21 |
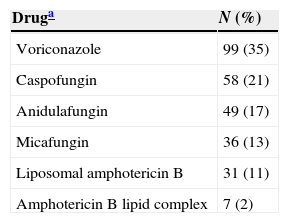
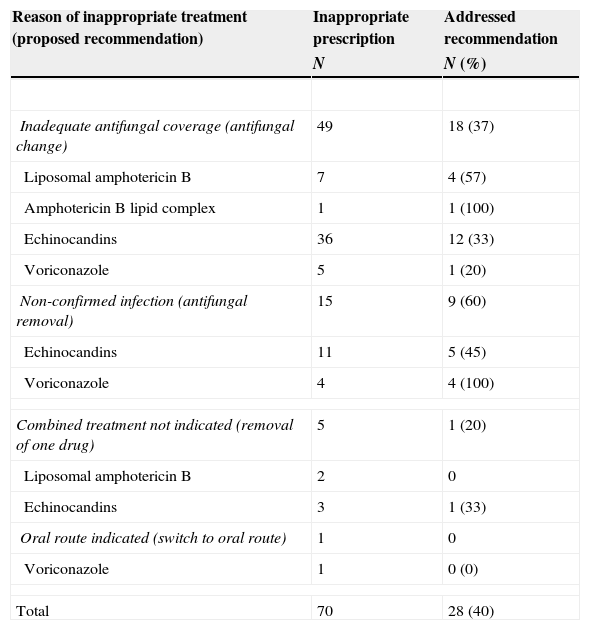
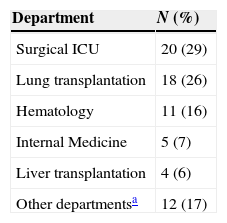
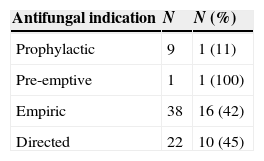
The most frequent prescribed antifungal drugs in the studied patients were echinocandins and voriconazole (Table 2). Overall, 70 (25%) prescriptions in 61 patients were considered amendable. The reasons of inappropriateness are shown in Table 3. Proposed recommendations were addressed in 28 prescriptions (40%). In 49 cases the recommendation made was to change the antifungal drug (adherence 37%), in 15 cases it was to remove the antifungal agent (adherence 60%), in 5 cases to remove one of the antifungal agents in the combined treatment (adherence 20%), and finally the change in the administration route in 1 patient (adherence 0%, Table 3). The adherence according to hospital departments and antifungal indications is expressed in Tables 4 and 5. When the recommendation was to change the current antifungal treatment to liposomal amphotericin B, adherence was 71%; however, it was lower when the recommended antifungal was voriconazole (38%) or fluconazole (26%).
Restricted antifungal prescribed in 261 patients.
| Druga | N (%) |
|---|---|
| Voriconazole | 99 (35) |
| Caspofungin | 58 (21) |
| Anidulafungin | 49 (17) |
| Micafungin | 36 (13) |
| Liposomal amphotericin B | 31 (11) |
| Amphotericin B lipid complex | 7 (2) |
Reasons of inappropriate antifungal treatment and addressed recommendation according to its indication.
| Reason of inappropriate treatment (proposed recommendation) | Inappropriate prescription | Addressed recommendation |
|---|---|---|
| N | N (%) | |
| Inadequate antifungal coverage (antifungal change) | 49 | 18 (37) |
| Liposomal amphotericin B | 7 | 4 (57) |
| Amphotericin B lipid complex | 1 | 1 (100) |
| Echinocandins | 36 | 12 (33) |
| Voriconazole | 5 | 1 (20) |
| Non-confirmed infection (antifungal removal) | 15 | 9 (60) |
| Echinocandins | 11 | 5 (45) |
| Voriconazole | 4 | 4 (100) |
| Combined treatment not indicated (removal of one drug) | 5 | 1 (20) |
| Liposomal amphotericin B | 2 | 0 |
| Echinocandins | 3 | 1 (33) |
| Oral route indicated (switch to oral route) | 1 | 0 |
| Voriconazole | 1 | 0 (0) |
| Total | 70 | 28 (40) |
Patients with recommendations of antifungal treatment depending on hospital departments.
| Department | N (%) |
|---|---|
| Surgical ICU | 20 (29) |
| Lung transplantation | 18 (26) |
| Hematology | 11 (16) |
| Internal Medicine | 5 (7) |
| Liver transplantation | 4 (6) |
| Other departmentsa | 12 (17) |
Adherence to the recommended antifungal treatment according to treatment indications.
| Antifungal indication | N | N (%) |
|---|---|---|
| Prophylactic | 9 | 1 (11) |
| Pre-emptive | 1 | 1 (100) |
| Empiric | 38 | 16 (42) |
| Directed | 22 | 10 (45) |
Prophylactic: prescription due to risk factors for Invasive fungal infection (IFI). Pre-emptive: prescription due to the presence of a biochemical marker of IFI (galactomannan) in patients with risk factors. Empiric: prescription in patients with clinical manifestation suspected to be due to IFI. Directed: IFI attributed to an isolated fungal species.
The mortality among the patients treated according to the recommendations of the ASP was 17% (4 patients), and 30% in those whose treatment was not modified (11 patients, 2 due to infection) (p=0.393).
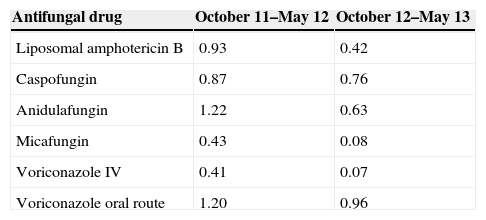
Antifungal consumption from October 2011 to May 2012 was 5.06 daily defined doses (DDD) per 100 occupied bed-days, which decreased to 2.92 DDDs (42% lower) during October 2012 to May 2013. A decrease was detected in the use of all antifungal drugs during the second period (Table 6).
Antifungal use during October 11–May 12 and October 12–May 13 (DDD per 100 occupied bed-days).
| Antifungal drug | October 11–May 12 | October 12–May 13 |
|---|---|---|
| Liposomal amphotericin B | 0.93 | 0.42 |
| Caspofungin | 0.87 | 0.76 |
| Anidulafungin | 1.22 | 0.63 |
| Micafungin | 0.43 | 0.08 |
| Voriconazole IV | 0.41 | 0.07 |
| Voriconazole oral route | 1.20 | 0.96 |
A quarter of the reviewed prescriptions were found to be amendable. As in similar studies, the most frequent causes of modifiable antifungal treatment were inadequate antifungal coverage, no confirmed infection, combined treatment not indicated or oral route indicated.2,21,27,34
The degree of adherence to recommendations in this study (40%) based on unsolicited consultations may be considered reasonable.11,17,22,34 This result may be encouraging taking into account the accused clinical severity of many patients, the suboptimal IFI diagnostic tools and the fact that the poor prognoses in many cases constitute relevant additional difficulties when giving antifungal advice.19,33 To improve adherence it is crucial that prescribing physicians rely on the wisdom and knowledge of the reviewer and maintain continual feedback.20,34 It should be considered that external reviewing physicians may be less compromised with the clinical evolution of the patient. This may explain why, even when susceptibility results are available to guide therapy, clinicians are often reluctant to de-escalate therapy when a seriously ill patient is improving with broad-spectrum treatment.19,33
The use of electronic clinical history record systems may help to save time when reviewing antimicrobial treatments and in optimizing the efficiency of this strategy.33 Some factors that have previously been related to the success of such strategies are the knowledge of local fungal epidemiology and resistances, establishing therapeutic guidelines, implementation of treatment strategies for empirical, pre-emptive and prophylactic therapy in defined patient populations, catheter management guidelines and the rapid communication of test results from the microbiology laboratory personnel to the physician.14,18
The degree of adherence was higher when the recommendation was to remove the antifungal (60%), perhaps because in many of these cases the prescribing physician was persuaded that maintenance of the antifungal agent was not justified.16,17 Many of these recommendations are related to the lack of confirmatory microbiological results or to the limited diagnostic value of the isolation of Candida species in the respiratory tree, drainage or other locations other than the blood or sterile liquids.4 Adherence was lower when the recommendation was to change the antifungal (37%). It should be noted that adherence was higher when the recommended antifungal agent was amphotericin B (which is perceived as a potent, broad-spectrum antifungal) than when the use of fluconazole was suggested.4,23,28 In one study, less than 40% of echinocandin-treated patients with fluconazole-susceptible organisms were de-escalated to fluconazole.9 Knowledge of resistance in bloodstream yeast infection can be extremely helpful when making any recommendation.9 Switching to oral route may be notable in the case of intravenous azoles because removing the intravenous line could prevent the development of blood stream infections.13
The use of restricted antifungal during the intervention period was 42% lower than during the comparison period. These results are similar to other studies2,5 which observed that the main benefit of adherence to antifungal recommendations was reductions in hospital stays, adverse effects and cost,8,9 together with reduced resistance to antifungals in cases of community acquired candidiasis.8,9 It should be noted that, in the present study, the use of all restricted antifungals actually decreased but were more pronounced in the case of anidulafungin, micafungin and intravenous voriconazole. The reduction in the prescription of intravenous voriconazole could, in part, be explained by a change in the prescription from intravenous to oral treatment.31 The lower mortality observed in patients treated according to the recommendations did not reach significance and may be more related to the severity of the patient with the persistence of antifungal treatment previously prescribed.7 In addition, it should be noted that options other than those suggested by the researchers could have resulted in a favourable clinical outcome.
Considering the marked use of antifungal treatments in hematologic and lung transplantation patients, it could be argued that ID consultations should be performed in services with the greatest consumption of antifungal agents such as hematology, transplant or the ICU,8,25,29 especially in hospitals that can only allocate limited human resources to ASPs. In addition, it would be preferable to target a few high cost antifungal drugs which may have suboptimal use, such as liposomal amphotericin, the echinocandins or intravenous voriconazole than to demonstrate an overall reduction in all antifungal drugs.4
Some limitations to our study must be noted. The results obtained in the intervention period were compared with those of the previous 12 months; thus, a bias resulting from a change in patient characteristics cannot be discharged. Another limitation is that not all the changes in antimicrobial treatments could be attributed to written recommendations because a deterrent factor cannot be ruled out due to prescribers being aware that the restricted antifungal treatment was to be reviewed. In addition, due to the fact that this was a time-limited study, an increased consumption of antifungals during the months following the intervention cannot be ruled out.
In summary, ASP in admitted patients may be successfully implemented with a high degree of compliance. This approach may be cost effective and could be included as part of an antimicrobial stewardship programme in institutions that devote limited human resources to improve antimicrobial prescribing.
Conflicts of interestThe authors declare no conflicts of interest.
Parts of this study were presented at 18th Spanish Society for Clinical Microbiology and Infectious Diseases Congress (Seville, Spain, 2014). This work was supported in part by unrestricted educational grants from the Spanish Ministry of Health [EC11-094]. The authors wish to thank Martin Hadley-Adams for assisting with the English language and preparation of the manuscript.