Application of sentinel lymph node biopsy (SLNB) procedure in early-stage vulvar cancer and analysis of results, recurrences and complications.
Material and methods40 patients with vulvar cancer and SLNB between 2008 and 2018 were retrospectively reviewed. During the surgical procedure the inguinofemoral lymph nodes were checked with a gamma probe to identify the sentinel nodes that were removed and referred for intraoperative pathological assessment. Subsequently, long-term patient follow-up was performed with analysis of complications, relapse and mortality.
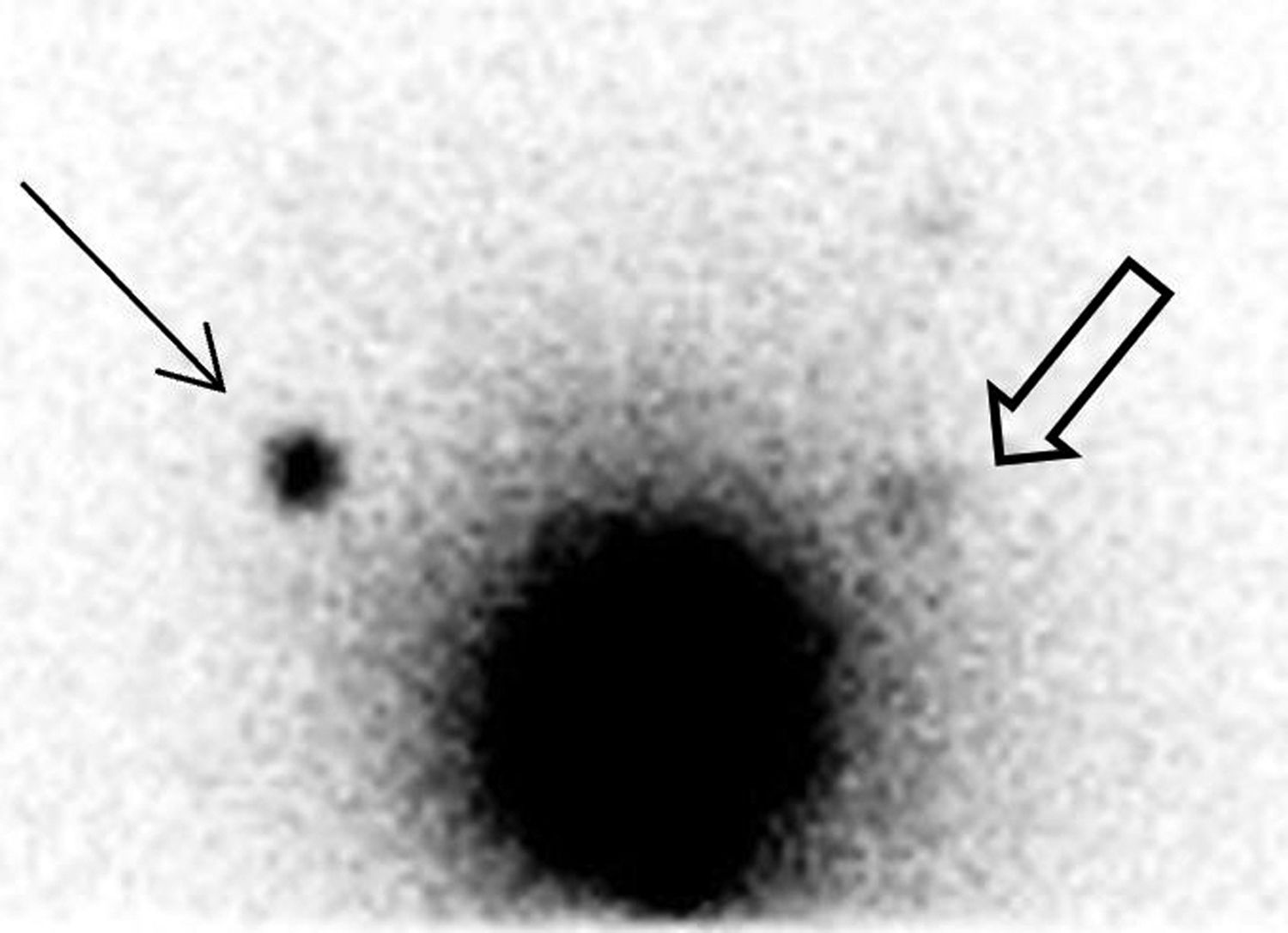
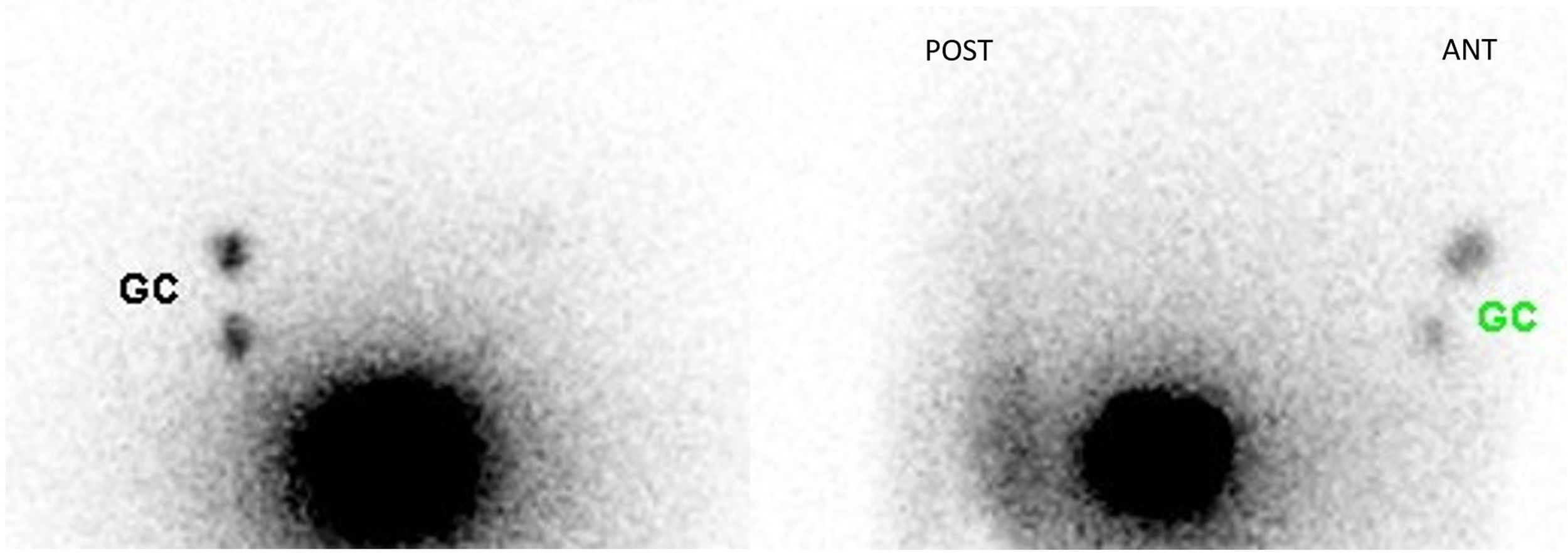
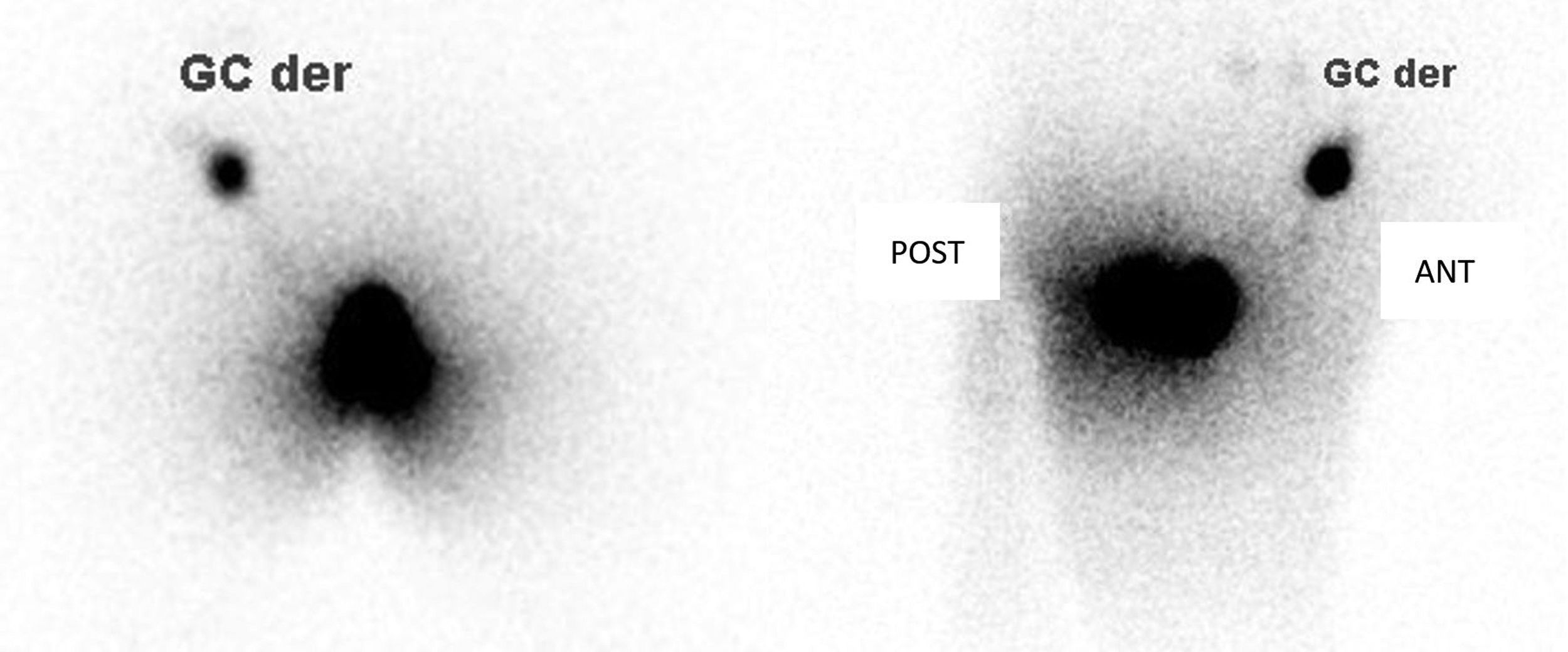
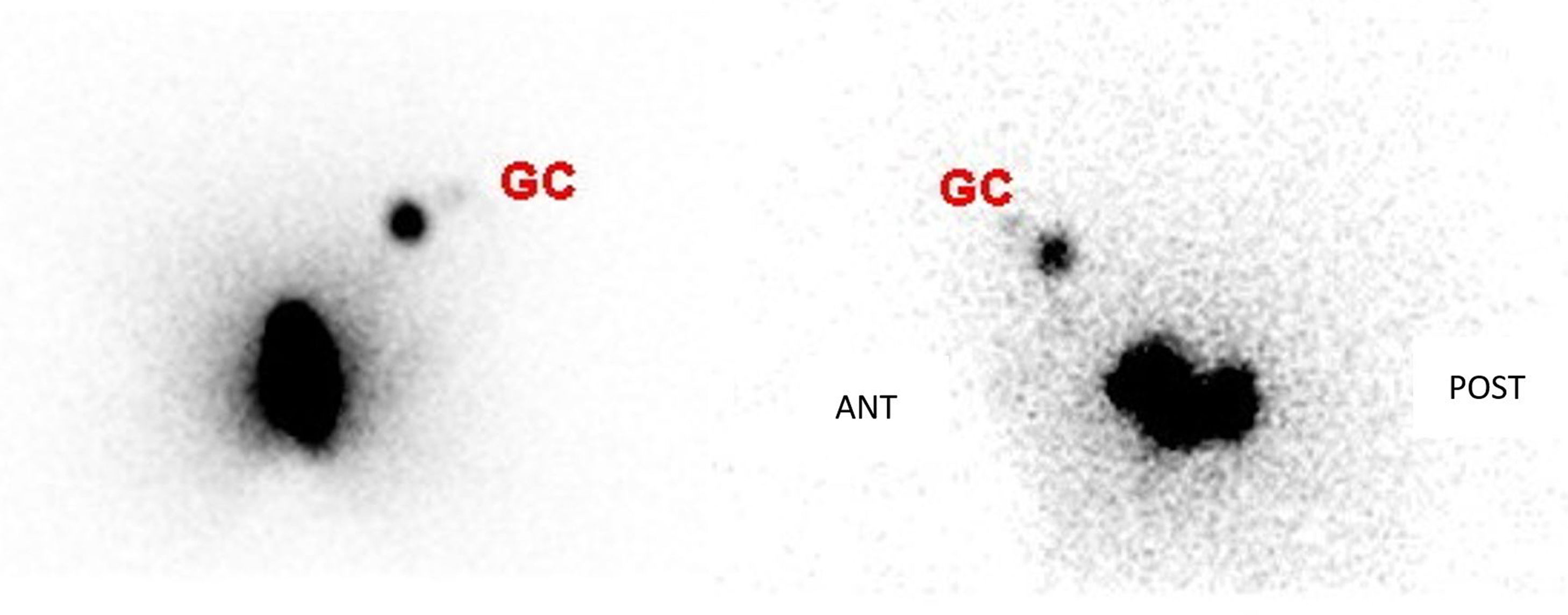
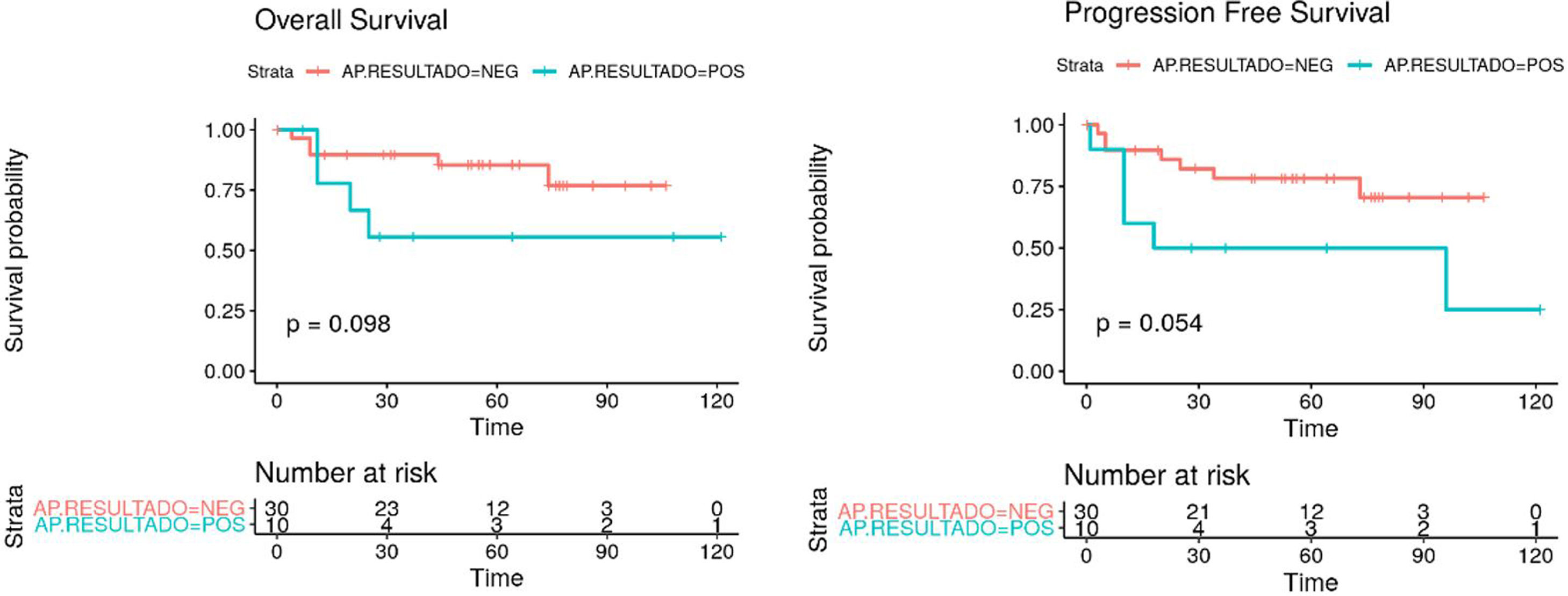
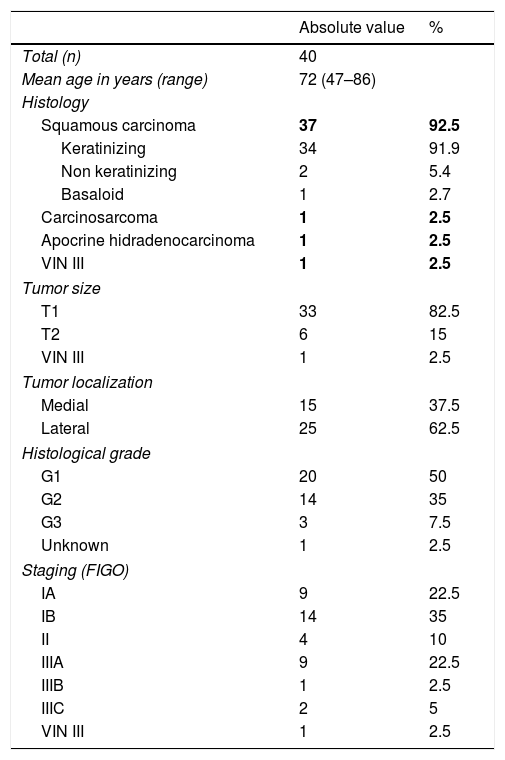
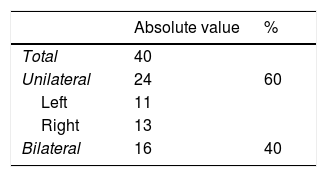
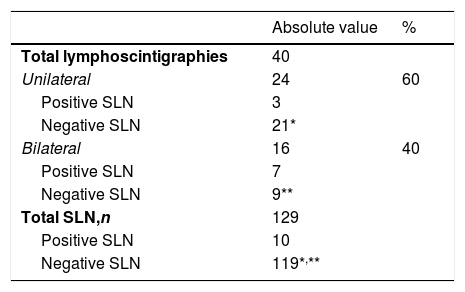
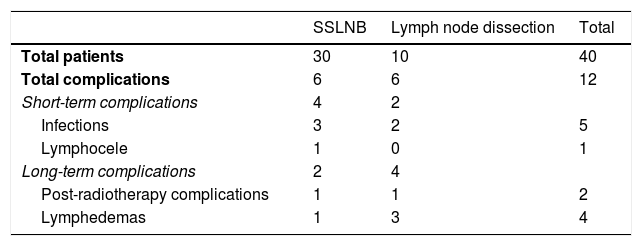
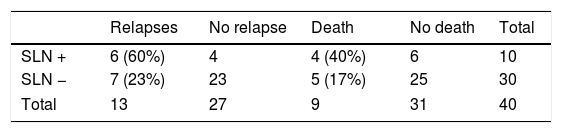
Results40 patients (mean age: 72 years [47–86]), the overall detection rate per patient was 95% and a total of 129 sentinel lymph nodes (SLNs) were removed (3.22SLN/patient). In 3 out of 25 patients with lateral tumor lesions drainage was bilateral and in 2 out of 15 with midline lesions drainage was unilateral. On lymphoscintigraphy, 16 out of 40 had bilateral drainage and 24 unilateral. A total of 119 SLN− and 10 SLN+ were obtained, in 8 out of 10 an inguinofemoral lymphadenectomy was performed. In the SLN− group, one case of lymphatic blockage and one false negative were included. In 12 out of 40 patients there were post-surgical complications, 4 of them lymphoedemas. In the median follow-up (40 months), 6 out of 10 with SLN+ (40% mortality) and 7 out of 30 SLN− (16% mortality) had recurrences.
ConclusionsSLNB in vulvar cancer is the technique of choice for correct staging and locoregional therapy. Correct clinical lymph node staging is important before surgery in order to avoid potential blockage drainages which could induce a false negative SLN.
Aplicación de la biopsia selectiva de ganglio centinela (BSGC) en el carcinoma de vulva en estadios iniciales y análisis de los resultados, recurrencias y complicaciones.
Material y métodosSe revisaron retrospectivamente 40 pacientes con cáncer de vulva y BSGC entre 2008 y 2018. El día de la intervención se rastrearon las cadenas ganglionares inguinales mediante sonda gammadetectora para identificar los ganglios centinela que se extirparon y remitieron para estudio anatomopatológico intraoperatorio. Posteriormente, se realizó seguimiento a largo plazo con análisis de complicaciones, recaída y mortalidad.
ResultadosDe las 40 pacientes (edad media: 72 años [47-86]), la tasa de detección global por paciente fue del 95%, con un total de 129 ganglios centinela (GC) (3,22GC/paciente). En tres de 25 pacientes con lesiones tumorales laterales el drenaje fue bilateral y en dos de 15 con lesiones de línea media fue unilateral. De las 40 linfogammagrafías 16 presentaban drenaje bilateral y 24 unilateral. Se obtuvieron un total de 119 GC− y 10 GC+, realizándose vaciamiento en ocho. En el grupo de GC− se incluyeron un caso de bloqueo linfático y un falso negativo. En 12 de 40 pacientes hubo complicaciones posquirúrgicas, cuatro de ellas linfedemas. Durante una mediana de seguimiento de 40 meses, recayeron seis de 10 con GC+ (40% mortalidad) y siete de 30 GC− (16% mortalidad).
ConclusionesLa BSGC en cáncer de vulva es la técnica de elección para una correcta estadificación y tratamiento locorregional. Es importante una adecuada estadificación ganglionar previa a la cirugía para evitar posibles bloqueos linfáticos que puedan inducir falsos negativos.
Article
If you experience access problems, you can contact the SEMNIM Technical Secretariat by email at secretaria.tecnica@semnim.es or by phone at +34 619 594 780.
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)