PSMA imaging has proved a great efficiency in recurrence work-up of prostate cancer and already revolutionized the prostate cancer management by a superior diagnostic performance over conventional diagnostic modalities such as computed tomography (CT) or multiparametric magnetic-resonance imaging (mpMRI).1 Nevertheless, there are certain clinical scenarios demanding a meaningful combination of PSMA hybrid imaging with a conventional imaging method.
We present a case of a 79-year-old male patient with mucinous adenocarcinoma of the prostate with a Gleason score of 9 and a PSA level of 20.0 ng/mL at the presentation in our clinic, who underwent a recurrence work-up due to referral because of gross hematuria. Since the patient had undergone prior transurethral resection interventions (TURP) with a Gleason score of 7, this case is to be regarded as a local relapse of prostate cancer. The recurrence work-up included the conduct of a contrast-enhanced, whole-body [18F]PSMA-1007 PET/CT scan (acquisition time of 120 min after an IV administration of 268 MBq tracer) and three weeks later an mpMRI of prostate.
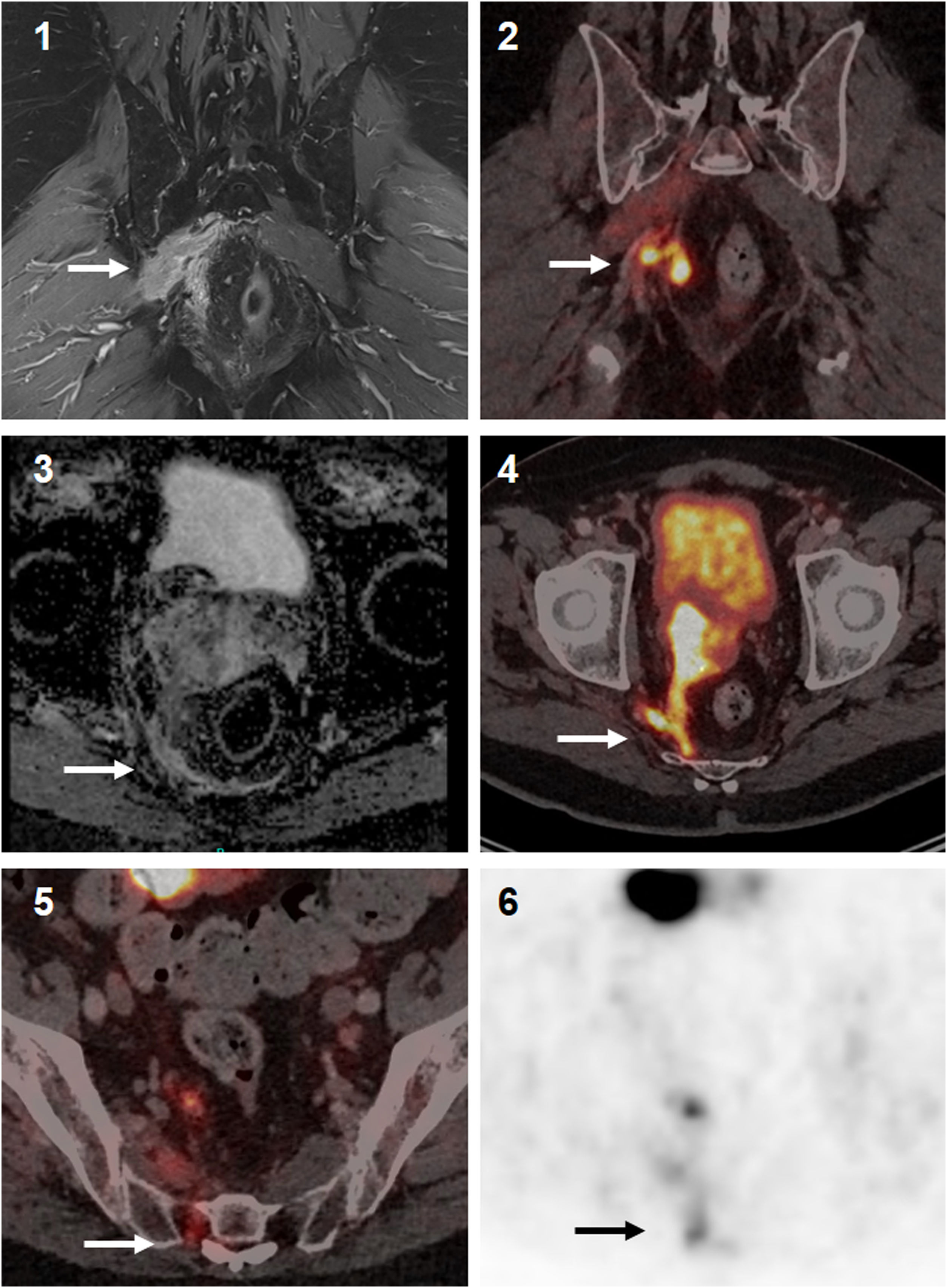
The contrast enhanced mpMRI demonstrated a locally advanced prostate cancer with infiltration of mesorectal fascia, right seminal vesicle and, besides, oedema with contrast enhancement of the right piriformis muscle and thickening of the nerval roots of the plexus sacralis indicated tumor infiltration, albeit mpMRI has limitations for the correct identification of mucinous parts of prostate carcinoma. In addition, mpMRI revealed multiple lymph node metastases in the pelvis. Despite morphologically extensive tumor involvement of the pelvic organs and the known diagnostic superiority of mpMRI over PET/CT regarding the soft tissue evaluation, a contrast-enhanced, whole-body [18F]PSMA-1007 PET/CT scan had to follow for a better tumor delineation in the area of sacral plexus, as this plays a pivotal role for the quality of life for patients as well as a correct radiotherapy planning (determination of gross tumor volume = GTV). The PSMA imaging revealed a locally advanced prostate cancer with infiltration of adjacent structures and organs involving right seminal vesicle, reaching to the anterior wall of the rectum and metastasis to pelvic lymph nodes and a further solitary metastasis to right scapular bone (Fig. 1). The tumor findings in the pelvis exhibited in total a moderate PSMA uptake with an SUVmax of up to 18.1, whereas the metastases to lymph nodes showed rather low PSMA uptake with an SUVmax of up to 1.9. An intensive [18F]PSMA-1007 uptake was seen in the scapular bone with an SUVmax of up 34.0 with no CT correlate. Clinically most significant [18F]PSMA-1007 finding was the identification and also correct tumor delineation in the area of sacral plexus, as [18F]PSMA-1007 imaging here adds further information to the MRI findings (Fig. 2).2,3 In the following clinical course, the patient received a PSMA-guided, palliative radiotherapy of the pelvic parts of malignant spread in combination of a systemic androgen deprivation therapy (ADT). The scapular lesion underwent osteoblastic changes after the initiation of ADT, which was interpreted as a validation of malignancy.
[18F]PSMA-1007 PET/CT scan; Maximum intensity Projection (MIP) (A), PET imaging (B1 − 4), fused [18F]PSMA-1007 PET/CT images (C1 − 4). Solitary metastasis of the right scapular bone (B1 and C1). Lymph node metastases and infiltration of the sacral foramina (B2 + C2) and the right piriformis muscle (B3 + C3). Intraprostatic PSMA uptake and central hypodense extension after multiple transurethral resections (B4 + C4).
Synergistic effect of multiparametric MRI and [18F]PSMA-1007 PET/CT imaging: Better delineation and discrimination of the local tumor extent (1,2). Due to the lack of ADC descent on MRI (3), it is not possible to distinguish reliably between infiltration or possible oedema. PSMA PET/CT (4) suggests tumor infiltration due to PSMA expression. In addition, [18F]PSMA-1007 imaging (5, 6) indicates tumor infiltration of the sacral plexus, which escapes the detection by the standard MRI protocol.
In this rare case of a mucinous adenocarcinoma, our patient could highly benefit from the complementary diagnostic efficacy of the combination of mpMRI and [18F]PSMA-1007 PET/CT scan for exact tumor delineation particularly for mucinous components of prostate cancer involving the sacral plexus.
Funding statementThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Institutional review board statementThis work was performed in line with the principles of the Declaration of Helsinki. Since all the procedures being performed were part of the routine care and this is an observational case study, the institutional Ethics Committee waives the ethical approval according to national/local regulations. Written informed consent was obtained from the patient for publication of this case review, including accompanying images.
Data availability statementThe data used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
F.L.G. has patent application for [18F]PSMA-1007 and is an advisor at ABX, Telix, and SOFIE Biosciences. The other authors declare no conflict of interest regarding this manuscript.
The authors gratefully acknowledge the participating patient.





![[18F]PSMA-1007 PET/CT scan; Maximum intensity Projection (MIP) (A), PET imaging (B1 − 4), fused [18F]PSMA-1007 PET/CT images (C1 − 4). Solitary metastasis of the right scapular bone (B1 and C1). Lymph node metastases and infiltration of the sacral foramina (B2 + C2) and the right piriformis muscle (B3 + C3). Intraprostatic PSMA uptake and central hypodense extension after multiple transurethral resections (B4 + C4). [18F]PSMA-1007 PET/CT scan; Maximum intensity Projection (MIP) (A), PET imaging (B1 − 4), fused [18F]PSMA-1007 PET/CT images (C1 − 4). Solitary metastasis of the right scapular bone (B1 and C1). Lymph node metastases and infiltration of the sacral foramina (B2 + C2) and the right piriformis muscle (B3 + C3). Intraprostatic PSMA uptake and central hypodense extension after multiple transurethral resections (B4 + C4).](https://static.elsevier.es/multimedia/22538089/0000004400000004/v1_202507071135/S2253808925000163/v1_202507071135/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![Synergistic effect of multiparametric MRI and [18F]PSMA-1007 PET/CT imaging: Better delineation and discrimination of the local tumor extent (1,2). Due to the lack of ADC descent on MRI (3), it is not possible to distinguish reliably between infiltration or possible oedema. PSMA PET/CT (4) suggests tumor infiltration due to PSMA expression. In addition, [18F]PSMA-1007 imaging (5, 6) indicates tumor infiltration of the sacral plexus, which escapes the detection by the standard MRI protocol. Synergistic effect of multiparametric MRI and [18F]PSMA-1007 PET/CT imaging: Better delineation and discrimination of the local tumor extent (1,2). Due to the lack of ADC descent on MRI (3), it is not possible to distinguish reliably between infiltration or possible oedema. PSMA PET/CT (4) suggests tumor infiltration due to PSMA expression. In addition, [18F]PSMA-1007 imaging (5, 6) indicates tumor infiltration of the sacral plexus, which escapes the detection by the standard MRI protocol.](https://static.elsevier.es/multimedia/22538089/0000004400000004/v1_202507071135/S2253808925000163/v1_202507071135/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)

