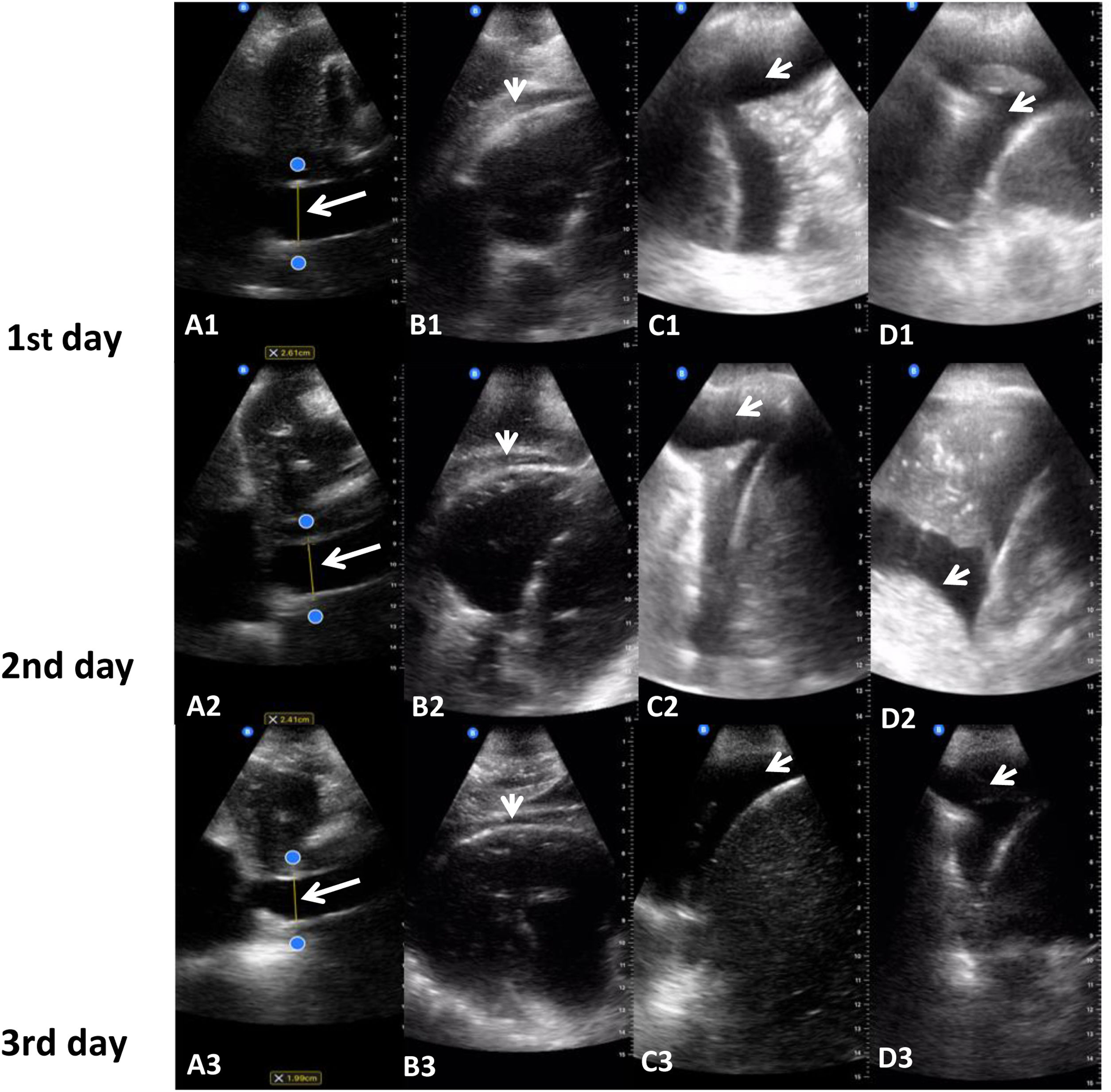
79-Year-old independent gentleman with no known diagnosis of dementia with past medical history of metastatic prostate cancer, 12 years of evolution (having received multiple therapies over this time, with brachytherapy, radiotherapy, and chemotherapy) and nephrostomy in situ for obstructive nephropathy, who consult to emergency service with clinic consisting of 24h of abdominal pain, diarrhea, vomiting, fever, shortness of breath, and general deterioration. On physical examination, its observed generalized cutaneous-mucous pallor, tachypnea with chest clear and abdomen soft painful on palpation in the left flank. The investigations showed Na+ 129mmol/L, K+ 4.5mmol/L, urea 14.7μmol/L, creatinine 125μmol/L, eGFR 48ml/min/0.73m2, Ca++ 2.15mmol/L, C-reactive-protein 176mg/L, Hb 89g/L, MCV 86fl, MCH 30.5pg, WBC 4.93×109/L and Plat 353×109/L; blood culture and urine culture showed growth of Escherichia coli sensitive to piperacillin–tazobactam and stool sample was negative. Considering these findings, the patient was diagnosed with urosepsis and considering the history of nephrostomy, is evaluated by the urology service who diagnose a blocked left nephrostomy and performed flushed and draining. Also, is diagnosed with new atrial fibrillation, commenced on digoxin and bisoprolol. Low molecular weight heparin started but was held due to low platelets. Considering shortness of breath, in the ward of hospitalization, it is done POCUS where observed, ventricular asynchrony, evidence of left ventricular hypertrophy bilateral pleural effusions, passive atelectasis, pericardial effusion, and enlarged vena cava being compatible with hypervolemia. So, it started treatment with furosemide, POCUS was performed on the first, third and fifth day with the aim of monitoring the response to treatment and adjusting the dose accordingly until clinical resolution (Fig. 1).
(A1, A2 and A3) Evolution of vena cava with diuretics at first, third and fifth day. (B1, B2 and B3) Evolution of pericardial effusion with diuretics at first, third and fifth day. (C1, C2 and C3) Evolution of right pleural effusion with diuretics at first, third and fifth day. (D1, D2 and D3) Evolution of left pleural effusion with diuretics at first, third and fifth day.
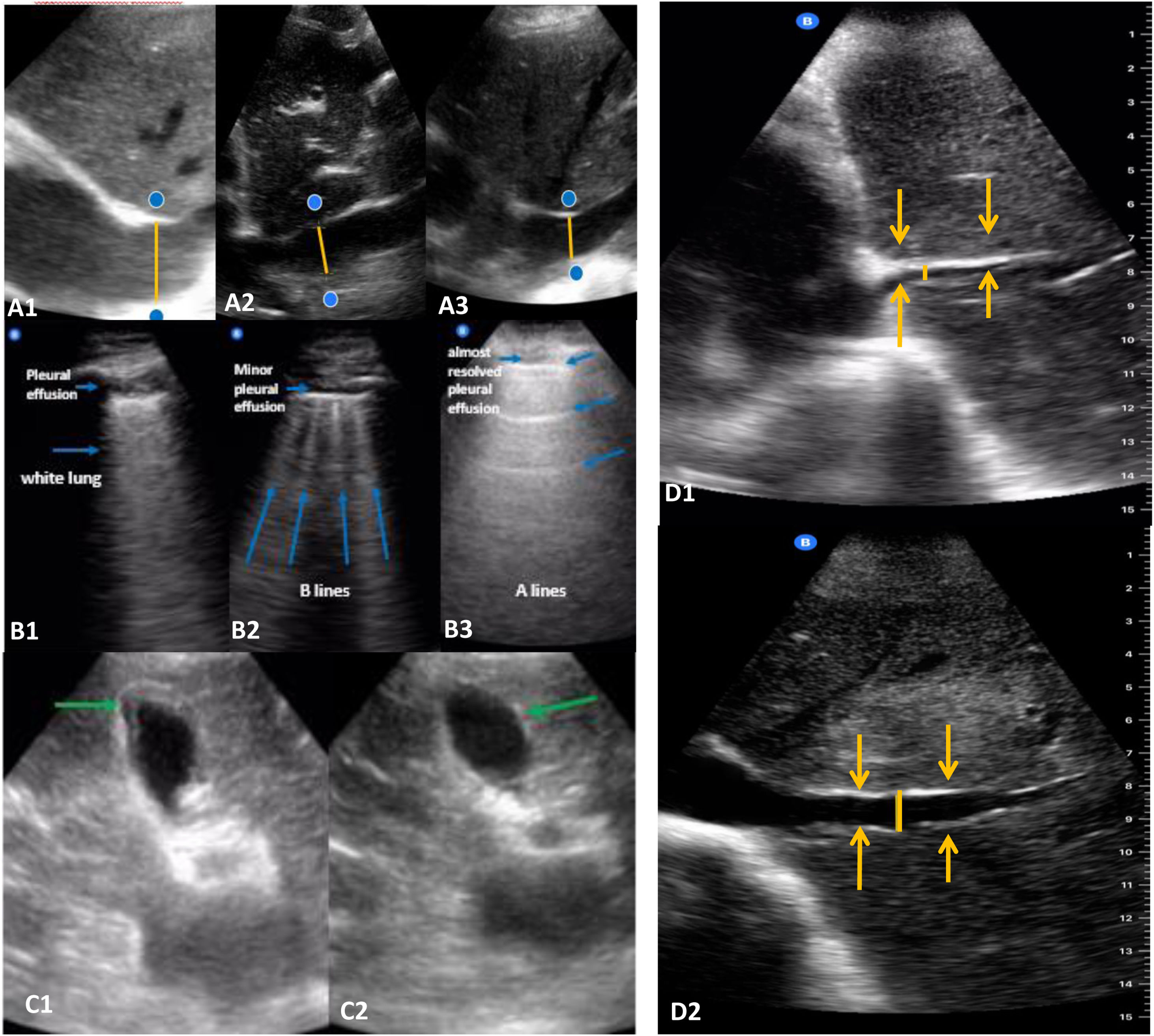
84-Year-old independent ex-smoker gentleman with no cognitive impairment and past medical history of chronic obstructive pulmonary disease (COPD), paroxysmal atrial fibrillation anticoagulated, heart failure with normal systolic function, EF >55% and chronic kidney disease (baseline GFR 45ml/min/1.73m2) who was taken to the hospital after being found on the floor by his granddaughter for a fall, the patient reported falling backwards onto his bottom in his bedroom, denying any preceding symptoms, head injury or loss of consciousness. On physical examination it was observed chest with creps and wheezes. In the investigations it was observed elevated CK levels, presumed rhabdomyolysis, and long lie reason for which commenced on intravenous fluids, Na 128mmol/L, K 4.3mmol/L, urea 14.4μmol/L, creatinine 145μmol/L, ALT 196U/L, C-protein-reactive 89mg/L, Hb 116g/L, WBC 11×109/L and Neutro 8.8×109/L. During hospitalization developed shortness of breath and wheeze, managed for exacerbation of COPD with antibiotics and steroids and atrial fibrillation with fast rate and decompensated heart failure. For this reason, lung POCUS is performed, observing compatible findings with bilateral interstitial syndrome (white lung), hypervolemic vena cava and congested gallbladder, so treatment with diuretics was started, adjusting the dose based on successive ultrasound and clinical controls until resolution of the condition, observing progressive separation of B lines and appearance of A lines (Fig. 2(A1–A3, B1–B3, C1–C2)).
(A1) Vena cava in a hypervolemic patient (heart failure). (A2) Vena cava during the treatment with diuretics. (A3) Vena cava after diuretics intravenous. (B1) Lung with interstitial syndrome (the A lines disappear, showing a white lung because of the union of multiple B lines). (B2) Improvement of the interstitial syndrome, observing the B lines more separated. (B3) Almost resolved pleural effusion, lines B disappear and lines A appear. (C1) Gallbladder in a hypervolemic patient (trilaminar wall). (C2) Gallbladder after intravenous diuretics. (D1) Vena cava in a hypovolemic patient clinically not evidenced. (D2) Vena cava after fluids intravenous.
80 years old patient, independent, no cognitive impairment, with past medical history of prostate adenocarcinoma and spinal metastasis, who went to emergency services with sudden onset weakness shortness of breath, fever and confusion. In the physical examination the oral mucosa was hydrated, chest with some basal creps, no other notable finding. In the investigations Na+ 132mmol/L, K+ 4.5mmol/L, urea 14.4μmol/L, creatinine 138μmol/L, eGFR 43ml/min/0.73m2, Ca++ 2.63mmol/L, C-reactive-protein 339mg/L, Hb 100g/L, MCV 85.1fl, MCH 28.2pg, WBC 21.3×109/L, Plat 272×109/L; electrocardiogram showed sinus rhythm; being diagnosed sepsis with respiratory source, CURB 65 Score 4, Type 1 respiratory failure, mild asymptomatic hyponatremia and acute on chronic kidney injury prerenal. In the ward of hospitalization, it is done POCUS with showed collapsed vena cava, suggestive of significant hypovolemia. For this reason, parenteral hydration was established with favorable clinical evolution (Fig. 2(D1–D2)).
DiscussionTo date, blood volume measurement in geriatric patients is done by physical examination and measurement of central venous pressure; on the other hand, monitoring of the response to diuretic in patients with heart failure treatments is carried out through physical examination and at the time of diagnosis, chest X-ray.
However, with the advancement of technologies, new tools have emerged for the evaluation of blood volume, such as ultrasound, describing that:
The inferior vena cava when measured from the right atrium is considered normal when the diameter is 1.5–2.5cm and compressibility around 50%, hypervolemia when the diameter was greater than 2.5cm and compressibility less than 50%, and hypovolemia when its diameter is less than 1.5 and compressibility greater than 50%.1
Nevertheless, it has described that lung ultrasound has a diagnostic accuracy of 95% for alveolar-interstitial syndrome and 93% for pleural effusion, chest radiography has a diagnostic accuracy of 72% for alveolar-interstitial syndrome and 47% for pleural effusion and physical exam (auscultation) has a diagnostic accuracy of 55% for alveolar-interstitial syndrome and 61% for pleural effusion.2
In relation to the B-line artifact, useful for the ultrasound diagnosis of interstitial syndrome, “the artifact” has been described as having a sensitivity of 92.5% and a specificity of 65.1% for the diagnosis of radiological alveolar-interstitial syndrome.3
In addition, it allows quantify the extent of lung injury and, it has proved to be cost-effective. POCUS also proved helpful in the management of hypotension and cardiac arrest (shock).4–6
Hence the importance of using POCUS for the evaluation and clinical follow up of older people with heart failure and blood volume disorders, and of practical training of geriatricians nowadays for its routine use.7–9
ConclusionsPOCUS is an accessible, cost-effective, and portable tool useful in the diagnosis and monitoring of treatments in older patients beyond the physical examination, especially in pathologies such as heart failure, and could constitute the fifth pillar of diagnosis alongside inspection, auscultation, palpation, and percussion.
Conflict of interestThe authors declare that they have no conflicts of interest.