To describe our experience treating dorsal radiocarpal fracture dislocations, regarding long-term clinical and radiological outcomes.
Material and methodRetrospective chart review of 15 patients treated in our institution from 2007 to 2021. Inclusion criteria were patients over 16 years, treated at a third level hospital of Madrid and an average follow-up of 56 months. Epidemiological data were collected from digital records. VAS, QuickDASH and Patient-Rated Wrist Evaluation (PRWE) scales were employed for clinical results assessment. All radiological studies were reviewed for radiological results assessment. A descriptive statistical analysis of all variables was developed.
ResultsAmong 15 patients with a mean follow-up of 56 months: 12 males (80%) and 3 females (20%) with a mean age of 39.5 years. The left wrist was injured in most cases (66.7%). All patients were treated surgically; 4 of them (27%) were assisted by wrist arthroscopy. Mean VAS at final follow-up was 2.6 with activity. Mean PRWE was 32 and mean QuickDASH was 28, which means satisfactory results. Eighty percent of patients developed wrist stiffness with most affected flexo-extension followed by prono-supination. Sixty-seven percent of patients developed radiological signs of wrist osteoarthritis at the end of follow-up.
ConclusionsIn spite of a large number of clinical and radiological complications during follow-up, long-term functional results are good in this kind of wrist injuries.
Describir nuestra experiencia en el tratamiento de las luxaciones radiocarpianas, aportando resultados funcionales y radiológicos a largo plazo.
Material y métodoEstudio retrospectivo de 15 pacientes tratados en nuestro centro desde 2007 a 2021. Los criterios de inclusión fueron pacientes mayores de 16 años tratados en un hospital de tercer nivel en la Comunidad de Madrid y seguidos un mínimo de 6 meses. Se recogieron datos epidemiológicos a través de la historia clínica electrónica. Se emplearon las escalas EVA, QuickDASH y Patient-Rated Wrist Evaluation (PRWE) para el análisis de resultados clínicos. Se realizó la revisión de pruebas de imagen para el estudio de resultados radiológicos. Análisis estadístico descriptivo de todas las variables.
ResultadosSe obtuvieron 15 pacientes con un seguimiento medio de 56 meses: 12 varones (80%) y 3 mujeres (20%) con una edad de media de 39.5 años. La muñeca izquierda fue la afectada en la mayoría de los casos (66,7%). Todos los pacientes fueron tratados quirúrgicamente, y en 4 de ellos (27%) se realizó asistencia artroscópica para el tratamiento de la lesión. La EVA media al final del seguimiento fue de 2,6 con actividad. El valor medio de la escala PRWE fue de 32, y de 28 para la escala QuickDASH, lo que se traduce en resultados satisfactorios. El 80% de los pacientes refirieron rigidez articular para flexo-extensión y prono-supinación. El 67% de los pacientes mostraron signos radiográficos de artrosis de muñeca al final de seguimiento.
ConclusionesA pesar del alto número de pacientes que desarrollan complicaciones durante el seguimiento, los resultados funcionales son satisfactorios a largo plazo.
Radiocarpal dislocations and fracture dislocations are extremely rare injuries. Current epidemiological data remain inaccurate, with approximate incidence and prevalence values reflected in a few case series.1–3 These are entities associated with high-energy trauma, most frequently in motorcycle accidents and falls.4–6 They occur in association with both skeletal and visceral systemic injuries, in the context of the polytrauma patient.
The exact mechanism of injury is not well established and depends on multiple factors: the volar radiocarpal ligaments are at their greatest tension during extension and ulnar tilt of the wrist. The compression and rotational forces that pass through the joint during trauma result in forced intracarpal supination movements that have been described as necessary to generate avulsion or rupture of the ligaments.7–10 Biondi et al.11 refer to the typical mechanism of injury during motorcycle accidents as “the throttle injury.” In these cases, the shearing forces that pass through the joint cause dorsal impaction of the carpus against the distal radius, causing a fracture and dorsal dislocation.
Dorsal displacement in radiocarpal dislocations is much more common than volar displacement.11–15 In the latter case, differential diagnosis with volar Barton's fracture is mandatory, since the carpus remains attached to the radial articular fragment through the intact volar radiocarpal ligaments.7
These injuries are highly complex, both in their bone and ligament components, making them extremely difficult to classify. Dumontier et al.12 described the most well-known system, based on involvement of the radial styloid. As progress has been made in understanding and understanding this type of injury, it has become clear that the classification systems described to date are overly simplistic.5,12 For this reason, Biondi et al.,13 proposed a new classification system for dorsal radiocarpal injuries based on distal radius fractures associated with ligamentous injuries, assessed by preoperative CT. These authors established four injury grades, from pure dislocations (type I) to genuine joint bursts (type IV), which result in a poorer prognosis. However, this system is far from perfect, as it focuses excessively on the bone component and pays little or no attention to the ligamentous component (intra- and extracarpal), which is equally or more important than the distal radius fracture itself.
The treatment principles are clear in the literature: restoration of radiocarpal joint congruity; diagnosis and treatment of associated ligament injuries, and stable ligament and bone repair.4,7,16 However, surgical treatment remains poorly standardised, and the role of wrist arthroscopy remains poorly established.17
The objective of this study is to describe our experience in the treatment of dorsal radiocarpal fracture dislocation, including the role that wrist arthroscopy may play in this process. We also describe the long-term clinical and radiological outcomes obtained in our series.
Material and methodBetween April 2006 and September 2021, 18 patients diagnosed with radiocarpal dislocation and fracture dislocation were seen and treated at our centre. The criteria for inclusion in this study were: patients older than 16 years, a diagnosis of radiocarpal dislocation or fracture dislocation, as well as surgical treatment and follow-up for a minimum of 6 months at our institution. Exclusion criteria included paediatric patients (under 16 years of age); other types of high-energy wrist injuries; joint sequelae from previous injuries, and patients transferred to other centres for treatment and/or follow-up.
Of the 18 patients initially selected, we were unable to contact 3 for follow-up and functional scale assessment, with the result that the final number of patients included in this study was 15, spanning a period from September 2007 to September 2021.
Epidemiological data were extracted from the electronic medical record, including age, sex, laterality, and type of injury according to the Dumontier et al. classification.12 The mechanism of injury; associated injuries; initial management in the emergency department; delay to definitive treatment; types of treatment; follow-up, and complications were collected and organised along with the rest of the epidemiological data in an Excel database.
A clinical assessment was performed using the Visual Analogue Scale (VAS) to assess residual pain, as well as the QuickDASH and Patient-Rated Wrist Evaluation (PRWE) scales.18 Residual active wrist balance was assessed using a conventional goniometer in the office. This parameter was measured in all patients for the affected wrists. This measurement was not performed on the healthy wrists, as the study objectives did not include a comparison between the affected and healthy sides due to the small sample size.
The radiological results were evaluated using posteroanterior and lateral projections of the wrist and included: development of degenerative changes, residual carpal subluxation, residual intracarpal instability, and Bouman's index for assessing residual ulnar translation of the carpus.19,20
A descriptive statistical analysis was performed on all study variables.
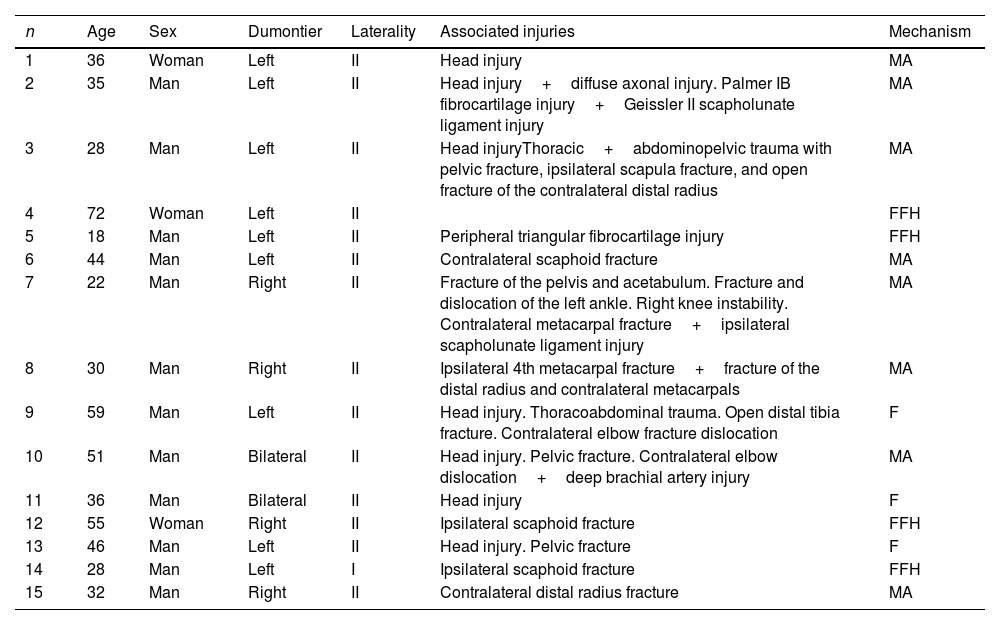
ResultsA total of 15 patients were included in the study, with a mean final follow-up of 56 months (range, 6–174 months): 12 men (80%) and 3 women (20%), with a mean age of 39.5 years (range, 18–72 years). The left wrist was affected in the majority of cases (66.7%), and 2 cases suffered a bilateral injury. The dominant hand was affected in 5 patients (33.3%). The epidemiological data and associated injuries are summarised and contained in Table 1.
Summary of epidemiological data, associated injuries and injury classification.
| n | Age | Sex | Dumontier | Laterality | Associated injuries | Mechanism |
|---|---|---|---|---|---|---|
| 1 | 36 | Woman | Left | II | Head injury | MA |
| 2 | 35 | Man | Left | II | Head injury+diffuse axonal injury. Palmer IB fibrocartilage injury+Geissler II scapholunate ligament injury | MA |
| 3 | 28 | Man | Left | II | Head injuryThoracic+abdominopelvic trauma with pelvic fracture, ipsilateral scapula fracture, and open fracture of the contralateral distal radius | MA |
| 4 | 72 | Woman | Left | II | FFH | |
| 5 | 18 | Man | Left | II | Peripheral triangular fibrocartilage injury | FFH |
| 6 | 44 | Man | Left | II | Contralateral scaphoid fracture | MA |
| 7 | 22 | Man | Right | II | Fracture of the pelvis and acetabulum. Fracture and dislocation of the left ankle. Right knee instability. Contralateral metacarpal fracture+ipsilateral scapholunate ligament injury | MA |
| 8 | 30 | Man | Right | II | Ipsilateral 4th metacarpal fracture+fracture of the distal radius and contralateral metacarpals | MA |
| 9 | 59 | Man | Left | II | Head injury. Thoracoabdominal trauma. Open distal tibia fracture. Contralateral elbow fracture dislocation | F |
| 10 | 51 | Man | Bilateral | II | Head injury. Pelvic fracture. Contralateral elbow dislocation+deep brachial artery injury | MA |
| 11 | 36 | Man | Bilateral | II | Head injury | F |
| 12 | 55 | Woman | Right | II | Ipsilateral scaphoid fracture | FFH |
| 13 | 46 | Man | Left | II | Head injury. Pelvic fracture | F |
| 14 | 28 | Man | Left | I | Ipsilateral scaphoid fracture | FFH |
| 15 | 32 | Man | Right | II | Contralateral distal radius fracture | MA |
MA: motorcycle accident; FFH: falls from height; F: falls.
The most common mechanism of injury was motorcycle accident in 8 cases (53%), falls from height in 4 patients (27%), and falls in 3 cases (20%). All dislocations were dorsal, and all patients were classified as Dumontier type II injuries, except for one case (Fig. 1a–c). In two cases, the injuries were open, classified as Gustilo types I and II, respectively. Preoperative CT was performed in eight cases, all of them between 2019 and 2021 (53%).
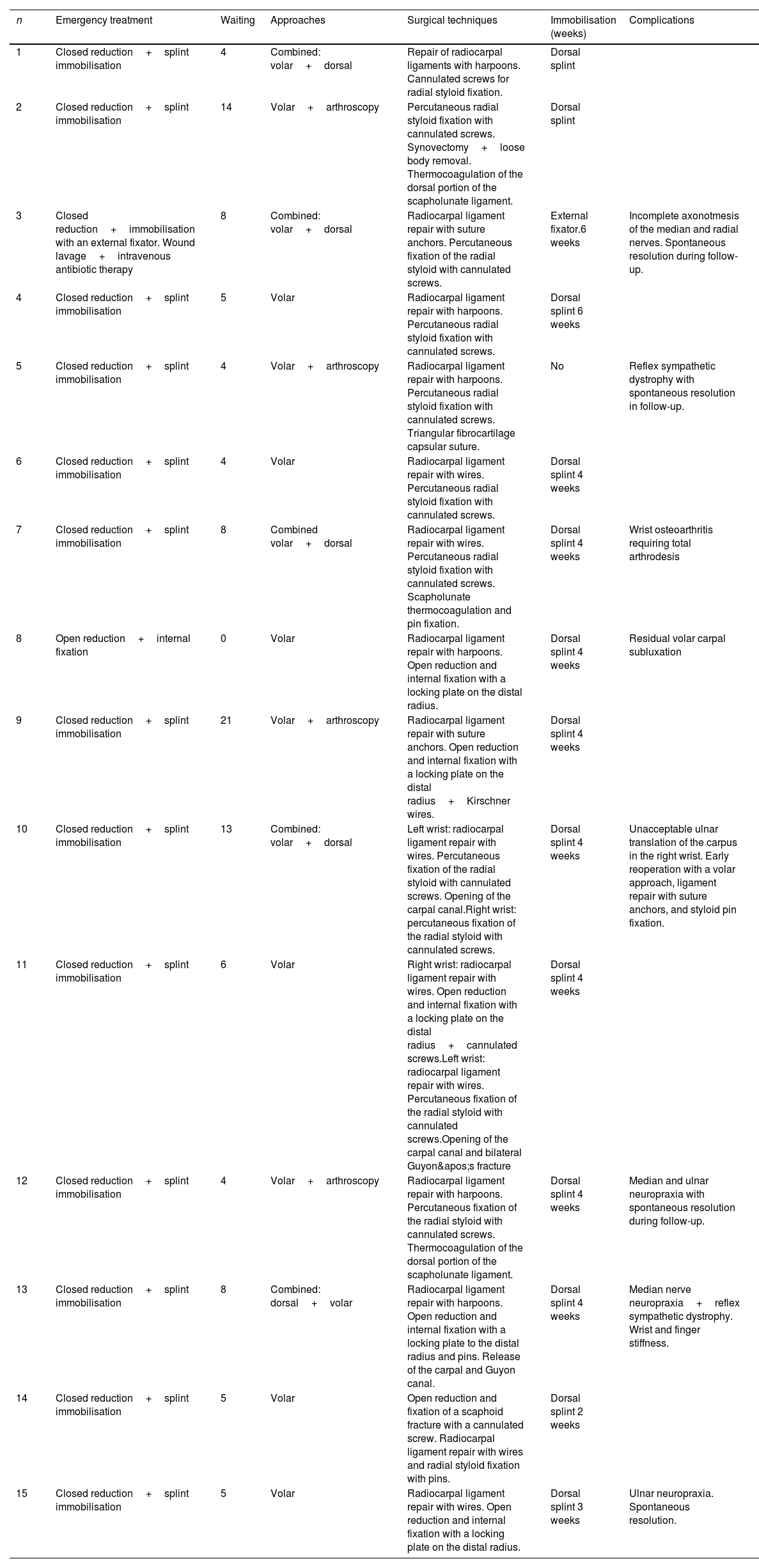
Initial treatment in the emergency department was closed reduction and immobilisation with a forearm cast in all cases, except for one patient, who required urgent external fixation due to an open injury. The delay until definitive treatment was 7 days (range 0–21 days). Definitive treatment was surgical in all cases, with an extended volar approach to reanchor the volar capsuloligamentous complex (Fig. 2). Five patients (33.3%) required a dual dorsal and volar approach. In four cases (27%), surgery was assisted by arthroscopy, with reduction of the articular surface under direct visualisation, and a diagnosis of intrinsic carpal injuries was made. The carpal tunnel and Guyon's canal were opened, and the neurovascular structures were released in three cases (20%). In these cases, the opening was performed prophylactically due to the significant tissue oedema. All cases except one, in which external fixation was performed, required postoperative immobilisation using a dorsal forearm splint for a mean period of 4 weeks. Data on the surgical techniques used are summarised and contained in Table 2.
Summary of data on treatment options and complications.
| n | Emergency treatment | Waiting | Approaches | Surgical techniques | Immobilisation (weeks) | Complications |
|---|---|---|---|---|---|---|
| 1 | Closed reduction+splint immobilisation | 4 | Combined: volar+dorsal | Repair of radiocarpal ligaments with harpoons. Cannulated screws for radial styloid fixation. | Dorsal splint | |
| 2 | Closed reduction+splint immobilisation | 14 | Volar+arthroscopy | Percutaneous radial styloid fixation with cannulated screws. Synovectomy+loose body removal. Thermocoagulation of the dorsal portion of the scapholunate ligament. | Dorsal splint | |
| 3 | Closed reduction+immobilisation with an external fixator. Wound lavage+intravenous antibiotic therapy | 8 | Combined: volar+dorsal | Radiocarpal ligament repair with suture anchors. Percutaneous fixation of the radial styloid with cannulated screws. | External fixator.6 weeks | Incomplete axonotmesis of the median and radial nerves. Spontaneous resolution during follow-up. |
| 4 | Closed reduction+splint immobilisation | 5 | Volar | Radiocarpal ligament repair with harpoons. Percutaneous radial styloid fixation with cannulated screws. | Dorsal splint 6 weeks | |
| 5 | Closed reduction+splint immobilisation | 4 | Volar+arthroscopy | Radiocarpal ligament repair with harpoons. Percutaneous radial styloid fixation with cannulated screws. Triangular fibrocartilage capsular suture. | No | Reflex sympathetic dystrophy with spontaneous resolution in follow-up. |
| 6 | Closed reduction+splint immobilisation | 4 | Volar | Radiocarpal ligament repair with wires. Percutaneous radial styloid fixation with cannulated screws. | Dorsal splint 4 weeks | |
| 7 | Closed reduction+splint immobilisation | 8 | Combined volar+dorsal | Radiocarpal ligament repair with wires. Percutaneous radial styloid fixation with cannulated screws. Scapholunate thermocoagulation and pin fixation. | Dorsal splint 4 weeks | Wrist osteoarthritis requiring total arthrodesis |
| 8 | Open reduction+internal fixation | 0 | Volar | Radiocarpal ligament repair with harpoons. Open reduction and internal fixation with a locking plate on the distal radius. | Dorsal splint 4 weeks | Residual volar carpal subluxation |
| 9 | Closed reduction+splint immobilisation | 21 | Volar+arthroscopy | Radiocarpal ligament repair with suture anchors. Open reduction and internal fixation with a locking plate on the distal radius+Kirschner wires. | Dorsal splint 4 weeks | |
| 10 | Closed reduction+splint immobilisation | 13 | Combined: volar+dorsal | Left wrist: radiocarpal ligament repair with wires. Percutaneous fixation of the radial styloid with cannulated screws. Opening of the carpal canal.Right wrist: percutaneous fixation of the radial styloid with cannulated screws. | Dorsal splint 4 weeks | Unacceptable ulnar translation of the carpus in the right wrist. Early reoperation with a volar approach, ligament repair with suture anchors, and styloid pin fixation. |
| 11 | Closed reduction+splint immobilisation | 6 | Volar | Right wrist: radiocarpal ligament repair with wires. Open reduction and internal fixation with a locking plate on the distal radius+cannulated screws.Left wrist: radiocarpal ligament repair with wires. Percutaneous fixation of the radial styloid with cannulated screws.Opening of the carpal canal and bilateral Guyon's fracture | Dorsal splint 4 weeks | |
| 12 | Closed reduction+splint immobilisation | 4 | Volar+arthroscopy | Radiocarpal ligament repair with harpoons. Percutaneous fixation of the radial styloid with cannulated screws. Thermocoagulation of the dorsal portion of the scapholunate ligament. | Dorsal splint 4 weeks | Median and ulnar neuropraxia with spontaneous resolution during follow-up. |
| 13 | Closed reduction+splint immobilisation | 8 | Combined: dorsal+volar | Radiocarpal ligament repair with harpoons. Open reduction and internal fixation with a locking plate to the distal radius and pins. Release of the carpal and Guyon canal. | Dorsal splint 4 weeks | Median nerve neuropraxia+reflex sympathetic dystrophy. Wrist and finger stiffness. |
| 14 | Closed reduction+splint immobilisation | 5 | Volar | Open reduction and fixation of a scaphoid fracture with a cannulated screw. Radiocarpal ligament repair with wires and radial styloid fixation with pins. | Dorsal splint 2 weeks | |
| 15 | Closed reduction+splint immobilisation | 5 | Volar | Radiocarpal ligament repair with wires. Open reduction and internal fixation with a locking plate on the distal radius. | Dorsal splint 3 weeks | Ulnar neuropraxia. Spontaneous resolution. |
The most common early complication observed in our series was neurapraxia of the median or ulnar nerves in four patients (27%), all of which resolved completely during follow-up without the need for revision surgery. In three of these patients, carpal tunnel and/or Guyon's procedure were not performed during the initial surgery, while one patient developed neurapraxia despite having been treated with this procedure. One patient with bilateral fracture dislocation required urgent examination of the right wrist after immediate postoperative examination revealed an intolerable ulnar translation of the carpus after the initial surgery. No cases of infection or material extraction were reported in our series.
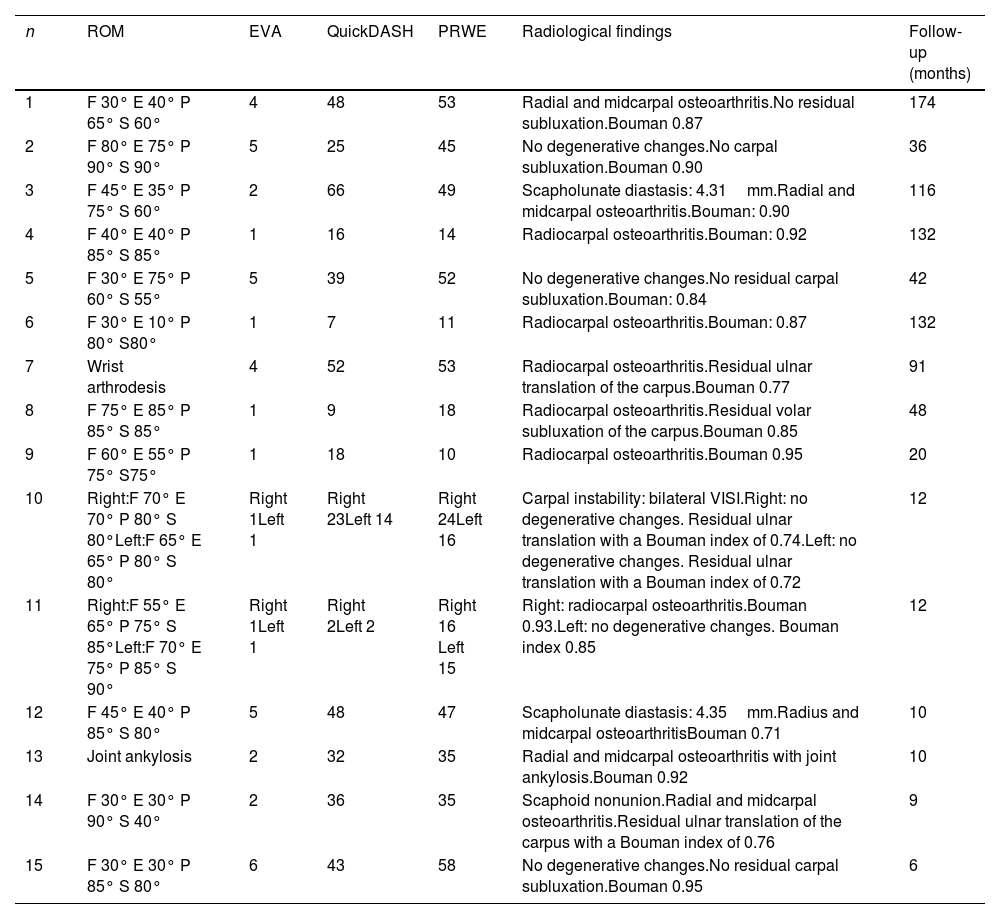
Regarding clinical outcomes, 12 patients (80%) reported moderate to severe loss of joint mobility, with particular impairment of flexion and extension. In 9 cases (60%), a moderate reduction in prono-supination was also detected. The “dart-throwing” movement was preserved in all cases except two: one patient who required total wrist arthrodesis due to symptomatic radiocarpal osteoarthritis, and spontaneous joint ankylosis in another case, in addition to severe joint degenerative changes (Table 3). The mean VAS score at the end of follow-up was 2.6 with activity; the mean PRWE score was 32 (range 10–58), and the mean QuickDASH score was 28 (range 2–66), which reflects satisfactory results.
Summary of data on long-term clinical, functional and radiological outcomes.
| n | ROM | EVA | QuickDASH | PRWE | Radiological findings | Follow-up (months) |
|---|---|---|---|---|---|---|
| 1 | F 30° E 40° P 65° S 60° | 4 | 48 | 53 | Radial and midcarpal osteoarthritis.No residual subluxation.Bouman 0.87 | 174 |
| 2 | F 80° E 75° P 90° S 90° | 5 | 25 | 45 | No degenerative changes.No carpal subluxation.Bouman 0.90 | 36 |
| 3 | F 45° E 35° P 75° S 60° | 2 | 66 | 49 | Scapholunate diastasis: 4.31mm.Radial and midcarpal osteoarthritis.Bouman: 0.90 | 116 |
| 4 | F 40° E 40° P 85° S 85° | 1 | 16 | 14 | Radiocarpal osteoarthritis.Bouman: 0.92 | 132 |
| 5 | F 30° E 75° P 60° S 55° | 5 | 39 | 52 | No degenerative changes.No residual carpal subluxation.Bouman: 0.84 | 42 |
| 6 | F 30° E 10° P 80° S80° | 1 | 7 | 11 | Radiocarpal osteoarthritis.Bouman: 0.87 | 132 |
| 7 | Wrist arthrodesis | 4 | 52 | 53 | Radiocarpal osteoarthritis.Residual ulnar translation of the carpus.Bouman 0.77 | 91 |
| 8 | F 75° E 85° P 85° S 85° | 1 | 9 | 18 | Radiocarpal osteoarthritis.Residual volar subluxation of the carpus.Bouman 0.85 | 48 |
| 9 | F 60° E 55° P 75° S75° | 1 | 18 | 10 | Radiocarpal osteoarthritis.Bouman 0.95 | 20 |
| 10 | Right:F 70° E 70° P 80° S 80°Left:F 65° E 65° P 80° S 80° | Right 1Left 1 | Right 23Left 14 | Right 24Left 16 | Carpal instability: bilateral VISI.Right: no degenerative changes. Residual ulnar translation with a Bouman index of 0.74.Left: no degenerative changes. Residual ulnar translation with a Bouman index of 0.72 | 12 |
| 11 | Right:F 55° E 65° P 75° S 85°Left:F 70° E 75° P 85° S 90° | Right 1Left 1 | Right 2Left 2 | Right 16 Left 15 | Right: radiocarpal osteoarthritis.Bouman 0.93.Left: no degenerative changes. Bouman index 0.85 | 12 |
| 12 | F 45° E 40° P 85° S 80° | 5 | 48 | 47 | Scapholunate diastasis: 4.35mm.Radius and midcarpal osteoarthritisBouman 0.71 | 10 |
| 13 | Joint ankylosis | 2 | 32 | 35 | Radial and midcarpal osteoarthritis with joint ankylosis.Bouman 0.92 | 10 |
| 14 | F 30° E 30° P 90° S 40° | 2 | 36 | 35 | Scaphoid nonunion.Radial and midcarpal osteoarthritis.Residual ulnar translation of the carpus with a Bouman index of 0.76 | 9 |
| 15 | F 30° E 30° P 85° S 80° | 6 | 43 | 58 | No degenerative changes.No residual carpal subluxation.Bouman 0.95 | 6 |
The results of the radiological analysis revealed that 12 patients (80%) developed signs of radiocarpal osteoarthritis. Four patients (27%) presented residual ulnar carpal translation, with a mean Bouman index of .74 (range .71–.77). Two cases also showed residual volar carpal subluxation. Four patients (27%) presented radiographic signs consistent with intracarpal injuries: scaphoid fracture in one case, scapholunate diastasis in two cases, and a bilateral VISI pattern in one case after surgery (Fig. 3a and b). All data on functional and radiological outcomes are compiled and contained in Table 3.
DiscussionThe primary restrainers of coronal carpal translation are the powerful volar radiocarpal ligaments. The radioscapholarge ligament originates from the volar lip of the radial styloid, at the level of the scaphoid fossa. Together with the dorsal radiotriquetral ligament, it participates in restricting ulnar translation of the carpus. The long radiolunar ligament originates from the volar lip of the scaphoid fossa, ulnar to the radioscaphoglottis. The short radiolunar ligament originates from the volar lip of the semilunar fossa of the distal radius. Radial styloid fractures associated with radiocarpal dislocations are usually caused by traction avulsions of the radioscaphoglottis and long radiolunar ligaments, whereas volar rim avulsions occur due to traction of the short radiolunar ligament.7,8,21-23 A wrist injury can only be classified as a radiocarpal dislocation if the volar ligaments are torn or have been avulsed from their sites of origin, regardless of the presence of fractures of the distal radius, intracarpal ligament injuries, or injuries to the distal radioulnar joint (DRUJ).
Some case series have reported good results with conservative or minimally invasive treatment using percutaneous needles.5,12,20,24 However, maintaining correct anatomical relationships and joint congruity can be difficult with these methods. Currently, surgical treatment is the treatment of choice for this type of injury due to its inherent complexity and instability.3 However, multiple points of controversy remain, including the use of arthroscopy.
In our experience, the volar capsuloligamentous complex is usually incarcerated within the joint after reduction manoeuvres, making proper healing impossible if managed conservatively. For this reason, we advocate for an extended volar approach in all cases, which allows for anatomical reattachment of the injured ligaments, proper joint lavage, extraction of free osteochondral fragments, and resection of most associated fractures. These findings are consistent with those of other series, which also advocate a mandatory volar approach for the treatment of this type of injury.5,7,8,14,25,26 The dorsal approach may be useful for reduction and osteosynthesis of the radial styloid, as well as for the treatment of associated intracarpal ligament injuries. In our series, a combination of dual approaches was used for 5 patients with dorsal carpal incarceration in whom anatomical reduction via the volar approach was impossible. More recently, minimally invasive dorsal approaches have been proposed for the treatment of this type of injury, using spanning plates as internal fixators. The goal is to ensure maintenance of longitudinal traction and joint reduction.14 Only Potter et al.25 combined volar ligament repair with this type of device, obtaining similar results in all series.
The most common technique for ligament repair is reanchoring with suture anchors.5,25,26 Extreme caution must be exercised in the positioning of the anchor and the tension applied to the suture, in order to recreate the anatomy and biomechanics of the volar capsuloligamentous complex.
Fixation of associated distal radius fractures depends on the location, fragment size, bone quality, and intra-articular extension. Bohm et al.26 have described the flipped volar rim, and how reduction of this small volar fragment is the key to the treatment of radiocarpal fractures. Kirschner wires, cannulated screws, fragment-specific plates, and locking buttress plates have been used in the treatment of radiocarpal fracture dislocations.8,12–14,20,26 In our series, the most common fixation method was the use of headless cannulated screws to achieve compression fixation of the radial styloid, followed by locking volar plates used in cases of severe joint comminution.
The role of wrist arthroscopy in this type of injury is not established, partly due to the paucity of published studies. However, it is clear that it can be a tool in the diagnosis and treatment of associated intracarpal injuries17,27; the evaluation of intra-articular fracture reduction; lavage; debridement, and assessment of osteochondral injuries, as well as the removal of intra-articular loose bodies. Furthermore, the volar capsuloligamentous complex is extra-articular, so its repair is currently impossible from an intra-articular approach, requiring an open technique.8 In our study, four patients received arthroscopically assisted surgical treatment, including suturing of the triangular fibrocartilage complex in one case, thermocoagulation of the dorsal portion of the EL ligament in two cases, and reduction of the radial articular surface in another. This finding currently makes our series the one with the highest number of patients to have received this treatment modality.
It has been well established that radiocarpal dislocations lead to joint stiffness, with particular impairment of mobility in the coronal plane and moderate impairment in pronation and supination.7 Spiry et al.,3 described a mean flexion of 47° and a mean extension of 30°. Cornu et al.20 reported a mean flexion of 63° and a mean extension of 51°. These results are similar to those obtained by Bohm et al.26 In our series, the mean flexion was 44°, and the mean extension was 43°.
Radiographically, these lesions frequently develop into radiocarpal osteoarthritis. Cornu et al.20 described signs of osteoarthritis in 43% of patients. However, only 3 cases were symptomatic. Wahl et al.28 published a series of 13 patients, 11 of whom developed degenerative changes in the wrist, with no clinical or functional significance. In our case, we observed degenerative changes in 66.7% of patients. However, the overall functional results were satisfactory, and the mean residual pain score was 2.6 with activity.
The established poor prognostic factors for this type of injury include open injuries; associated intracarpal injuries; neurovascular injuries; marginal injuries of the distal radius that are difficult to synthesize; non-anatomical reduction of the articular surfaces, and severe joint comminution,3,7 which emphasizes the importance of correct early diagnosis and appropriate, timely treatment.
This study has important limitations, such as its retrospective design and small sample size. Notwithstanding, it is a study with a long follow-up period that we believe will help us better understand the natural history of this type of injury. We also describe arthroscopically assisted cases, the most published series to date using this technique. Further reviews and studies are needed to more specifically establish the usefulness of this tool in the treatment of radiocarpal dislocation.
ConclusionsExpected outcomes after dorsal radiocarpal dislocation include the development of wrist stiffness and joint osteoarthritis. However, long-term functional results have proven satisfactory.
Level of evidenceLevel of evidence V.
Ethical considerationsThe study was evaluated by the centre's ethics committee, ensuring compliance with the data protection requirements for the reviewed medical records. As this was not an experimental study, registration with the hospital committee was not required.
FundingThis study was not funded by any public or private entities. The authors also declare that they did not receive any compensation for the development of this article.
Conflict of interestsAll authors declare that there are no conflicts of interest.