To analyze clinical and radiological mid-term outcomes in patients with scaphoid pseudarthrosis treated with arthroscopy-assisted osteosynthesis and autologous bone grafting.
Materials and methodsThirty-one patients (27 males, 4 female) were included in a retrospective study, with one bilateral case. The mean age was 28 years, and mean follow-up was 54 months. Twenty-six non-unions were in the waist, 5 in the proximal third, and one in the distal third. Arthroscopic debridement was performed and autologous bone graft from iliac crest was used. Fixation was performed percutaneously with a compression screw. Clinical and radiological evaluations were conducted preoperatively and postoperatively at one, three, six and twelve months. An additional mid-term follow-up visit was conducted. Patients were assessed for pain, wrist strength, range of motion and functional outcomes.
ResultsRadiological consolidation was achieved in 100% of cases within 12 weeks, with a mean of 10 weeks. Pain on the visual analog scale decreased from 7.1 to 1.5. Wrist strength improved from 27 to 48kg. Quick DASH improved from 58 to 11. Range of motion also increased: flexion from 51° to 71°, extension from 47° to 73°, radial deviation from 12° to 15°, and ulnar deviation from 23° to 36°. No complications were observed among the studied patients, and all returned to their respective jobs.
ConclusionsArthroscopy-assisted osteosynthesis with percutaneous compression screw and cancellous bone grafting has proven to be a viable method for the treatment of scaphoid pseudarthrosis, with low morbidity, good functional mid-term outcomes, and short consolidation periods.
Analizar los resultados clínicos y radiológicos a medio plazo en pacientes con seudoartrosis de escafoides tratados con osteosíntesis asistida por artroscopia e injerto óseo autógeno.
Materiales y métodosSe incluyeron 31 pacientes (27 hombres, 4 mujeres) en un estudio retrospectivo, con un caso bilateral. La edad media fue de 28 años y el seguimiento medio de 54 meses. Veintiséis seudoartrosis estaban en el tercio medio, 5 en el tercio proximal y una en el tercio distal. Se realizó desbridamiento artroscópico y se utilizó injerto óseo autógeno de la cresta ilíaca. La fijación se realizó de forma percutánea con un tornillo de compresión. Se realizaron evaluaciones clínicas y radiológicas preoperatorias y postoperatorias al mes, 3, 6, y 12 meses. Se realizó una última consulta adicional a medio plazo. Se evaluaron el dolor, la fuerza de la muñeca, el rango de movimiento y los resultados funcionales.
ResultadosSe logró la consolidación radiológica en el 100% de los casos en un plazo de 12 semanas, con una media de 10 semanas. El dolor en la escala visual analógica disminuyó de 7,1 a 1,5. La fuerza de la muñeca mejoró de 27 a 48kg. El Quick DASH mejoró de 58 a 11. También aumentó el rango de movimiento: la flexión pasó de 51 a 71°, la extensión de 47 a 73°, la desviación radial de 12 a 15° y la desviación cubital de 23 a 36°. No se observaron complicaciones entre los pacientes estudiados y todos retornaron a sus respectivos trabajos.
ConclusionesLa osteosíntesis asistida por artroscopia con tornillo de compresión percutáneo e injerto óseo esponjoso ha demostrado ser un método viable para el tratamiento de la seudoartrosis de escafoides, con baja morbilidad, buenos resultados funcionales a medio plazo y períodos de consolidación cortos.
When a scaphoid fracture progresses to pseudarthrosis the carpus gradually misaligns, leading to the development of radiocarpal and subsequently midcarpal arthritis.1 This progression clinically manifests as pain, stiffness, and loss of wrist strength.2,3 Open surgical treatment of scaphoid pseudarthrosis can be vascularized or non-vascularized, using bone grafts, usually in combination with supplementary internal fixation.4 This treatment leads to fracture consolidation in 80–90% of cases, depending on the technique used.2
With the increased use of wrist arthroscopic techniques and the use of bone grafts through them, a minimally invasive way to treat such injuries has emerged. Several studies have demonstrated the advantages of this procedure over open surgery.3,5 Among others, it can be highlighted the reduction of damage to the soft tissues surrounding scaphoid and better visualization of other associated intra-articular injuries. Additionally, it results in less postoperative pain and reduced joint stiffness, which in turn shortens the recovery time.2–4
The objective of our study is to analyze clinical and radiological outcomes in our initial 31 patients with scaphoid pseudarthrosis treated with arthroscopy-assisted osteosynthesis and autologous bone grafting. We hypothesized that arthroscopy-assisted osteosynthesis with autologous iliac crest bone graft would result in high union rates, good functional outcomes, and low morbidity in patients with scaphoid non-union.
Materials and methodsA retrospective study of patients diagnosed with scaphoid pseudarthrosis treated with arthroscopy-assisted osteosynthesis with autologous bone grafting and percutaneous internal fixation is presented. This study was conducted over a period of 5 years (from 2016 to 2021). Approval was granted by the Ethics Committee of Institutional Review Board of our Hospital (CEIm No: 24/451) and informed consent was obtained from all individual participants included in the study.
Thirty-one patients (32 wrists) were initially included in the study, and all of them completed the minimum follow-up period of 36 months, with a mean follow-up of 54 months (range 38–84). No patients were lost to follow-up at any stage of the study. Patients who missed an appointment were actively contacted by telephone and email, and new appointments were scheduled to avoid dropouts.
The inclusion criteria were a symptomatic non-union of the carpal scaphoid and age over 18 years. The exclusion criteria were having had a previous fracture or surgery in that wrist, a period of less than 6 months since the trauma, avascular necrosis of the proximal pole, SNAC (scaphoid non-union advanced collapse) wrist stages II, III, and IV, and patients under 18 years of age. Age, sex, and hand dominance were assessed.
All procedures were performed by three hand surgeons from our institution. Each surgeon possessed in-depth knowledge and extensive experience in wrist arthroscopy and in the arthroscopic management of scaphoid non-union. According to Tang and Giddins’ classification, this corresponds to the “highly experienced” level of surgical expertise (level IV).6
Clinical evaluationClinical outcome assessment was based on several variables. Pain intensity was recorded on a 0–10 visual analog scale (VAS) (0=no pain; 10=worst imaginable pain). We specifically captured VAS-with-activity, defined as the average pain during activities of daily living in the previous 7 days.
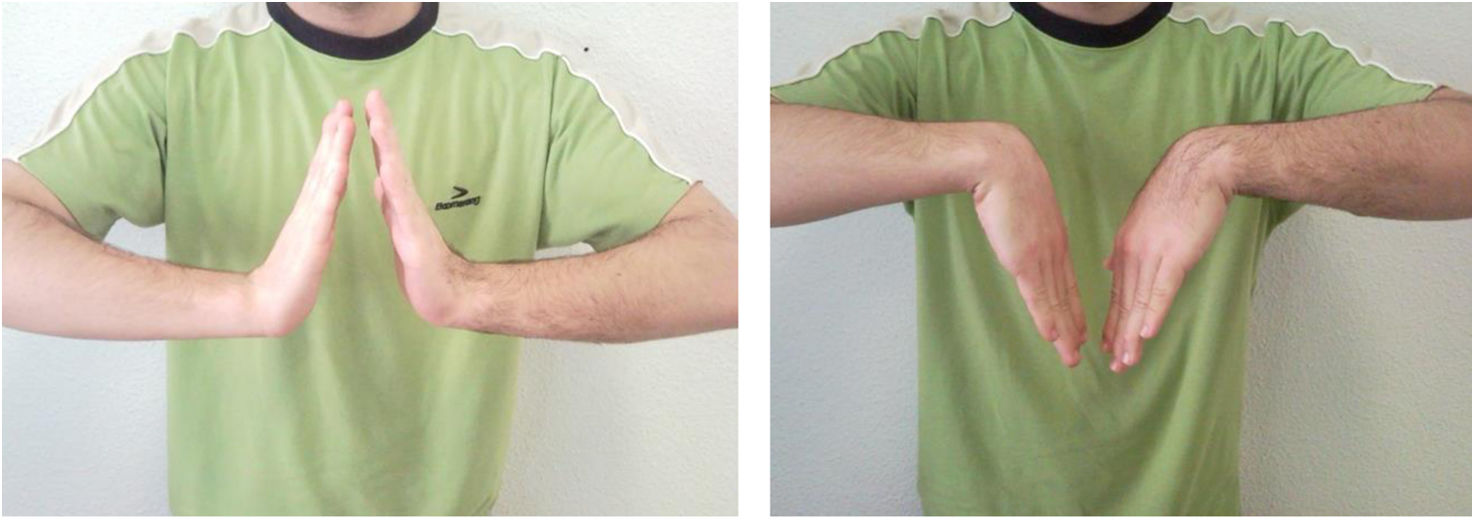
Range of motion was measured with a standard manual goniometer. Measurements were performed with the patient seated, shoulder in neutral, elbow at 90° flexion, forearm in neutral rotation for flexion–extension, and forearm pronated supported on the table for radial–ulnar deviation; the best of two consecutive measurements was recorded. Grip strength was assessed with a Jamar hydraulic hand dynamometer, with the patient seated, shoulder adducted, elbow at 90°, forearm in neutral and wrist in slight extension (20°). Three trials were performed with 30-s rest and the mean value (kg) was analyzed.
Each patient completed the Spanish version of the Quick Disabilities of the Arm, Shoulder, and Hand (Quick DASH) questionnaire during preoperative and postoperative follow-up.7 Return to work and sport was categorized as return without limitations versus with limitations or no return and documented at mid-term follow-up.
According to our institutional protocol, postoperative assessments were performed at 1, 3, 6, and 12 months. Control radiographs and measurement of pain, strength, and range of motion of the operated wrist were performed at each postoperative visit. Clinical evaluations were carried out in person by the principal surgeons who had performed the surgery.
After the 12-month visit, patients were discharged from routine surveillance. For the purposes of this retrospective analysis, all patients were later contacted and invited to attend one additional mid-term follow-up visit in January 2025, at which clinical scores and radiographic findings were recorded. The postoperative data reported in the “Results” section corresponds to this final follow-up visit.
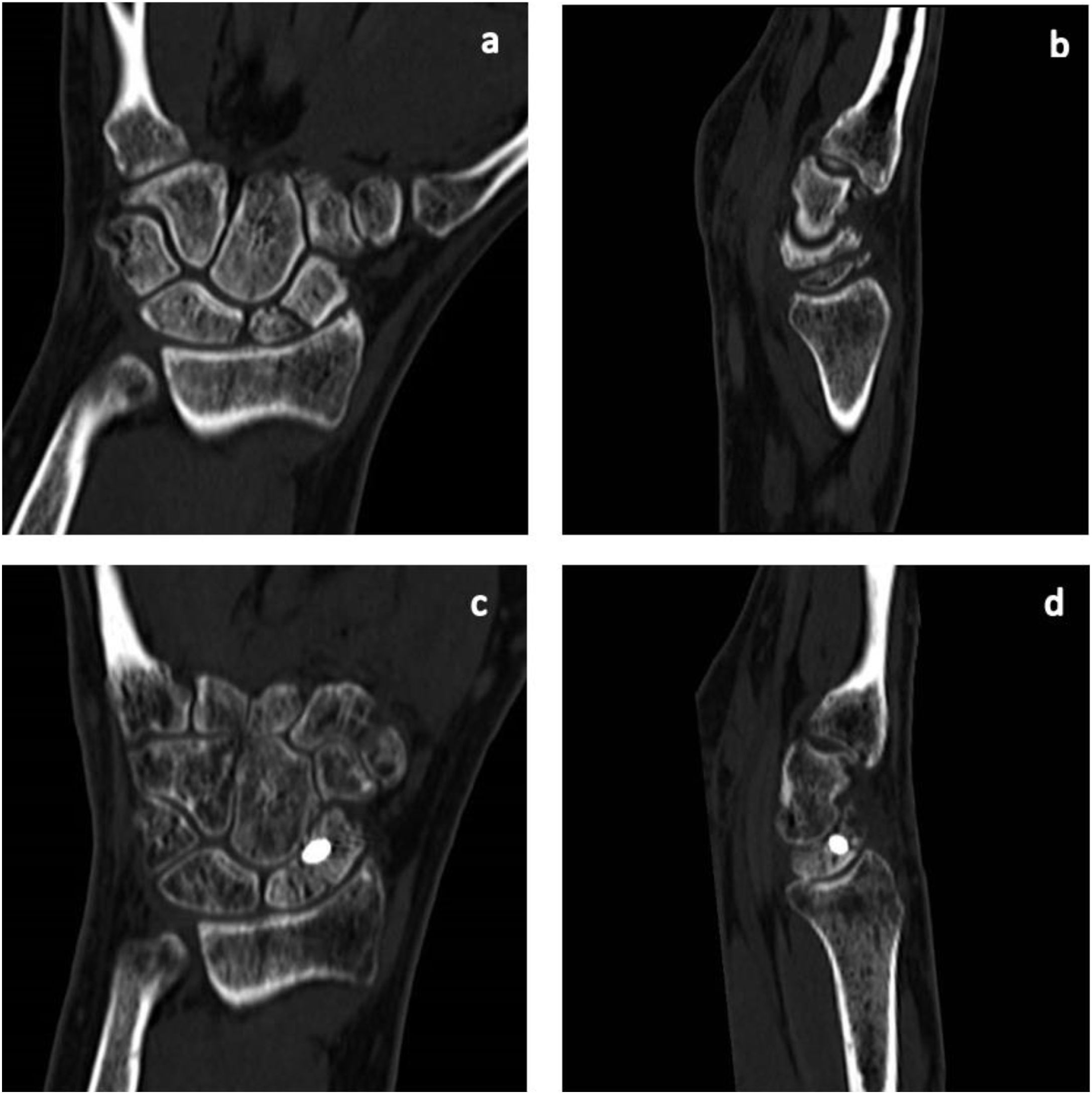
Radiological evaluationStandard preoperative radiographs were obtained in anteroposterior, lateral, oblique, and ulnar deviation projections of the affected wrist. Additionally, all patients underwent preoperative computed tomography (CT) to classify the injury and plan the surgical procedure.
The non-union of the scaphoid was radiographically evaluated by two individuals, the surgeon who had performed the surgery and a radiologist specialized in musculoskeletal pathology. Both evaluated it independently. To determine the type and location of the non-union, the classification used was that of Herbert and Fisher.8
In the postoperative period, the four radiographic projections described were repeated. Postoperative CT was not systematically performed in all patients. According to our institutional protocol, CT was reserved for cases in which there was discordance between clinical symptoms and radiographic findings (three patients in our study, apparently consolidated on radiographs but with persistent pain) to avoid unnecessary radiation exposure.
To determine bone union, both clinical and radiological aspects were considered. Clinically, the absence of tenderness upon palpation of the anatomical snuffbox, the scaphoid tubercle, and axial compression of the thumb of the hand were deemed necessary. The absence of pain with load was also necessary. Radiological consolidation was assessed according to a scoring system based on the resolution of the fracture line at the non-union site.9,10 Systematic inspection of the four cortices in orthogonal projections was performed, assigning each cortex a score of 1 (no callus and visible fracture line), 2 (callus present but fracture line still visible), or 3 (cortical bridging with disappearance of the line), for a total sum of 4–12 points. Union was defined as the presence of bridging callus in at least three of the four cortices and/or a score ≥10, in the absence of localized mechanical pain.
In cases where CT was performed, pseudarthrosis was considered consolidated if a trabecular bone bridge of more than 50% could be demonstrated in at least three CT slices.11,12 The surgeon who had performed the surgery and a musculoskeletal radiologist independently evaluated the postoperative CT scan (Fig. 1).
Surgical techniqueThe surgery was performed under general anesthesia with ischemia of the operated limb. The wrist was suspended in a traction tower with approximately 5–6kg of counterweight on the second and third fingers.
Dry arthroscopy was performed, using a 2.7mm arthroscope and the usual portals 3–4, 6R, ulnar midcarpal (MCU) and radial midcarpal (MCR).13 Simultaneously with the procedure on the scaphoid bone, another surgeon harvested cancellous bone graft from the contralateral iliac crest of the patient through a 2–3cm mini-incision. The iliac crest was chosen as donor site because it allows harvesting a sufficient volume of cancellous bone, with good biological properties, and can be obtained simultaneously by another surgeon during wrist arthroscopy, thus reducing operative time.
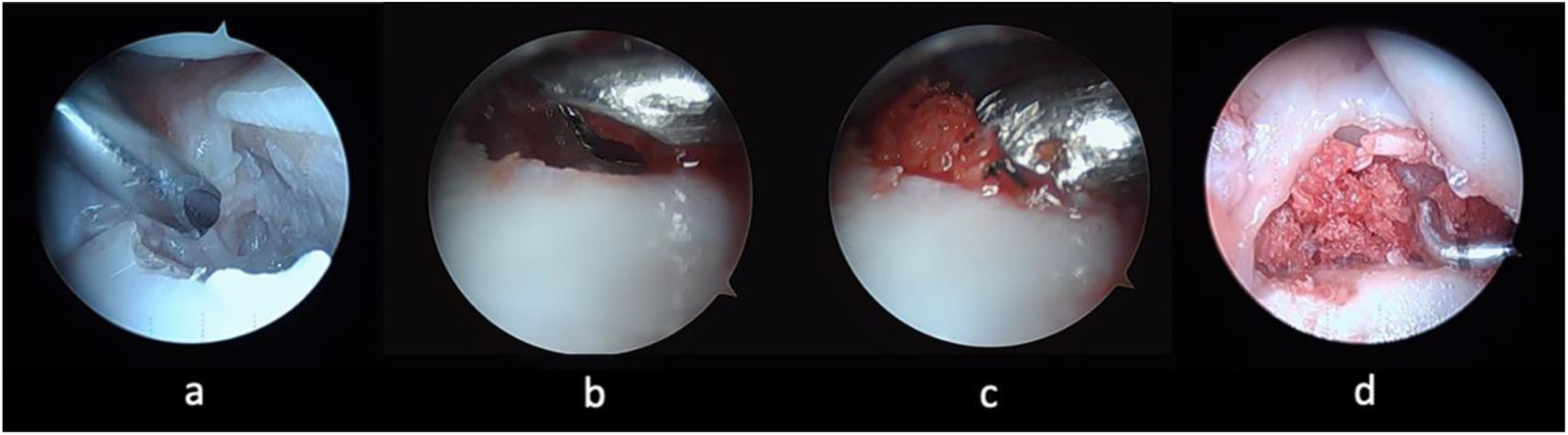
Once the scaphoid non-union is identified, the focus was debrided with a synoviotome and motorized burr (Fig. 2a). This process removes the sclerotic bone on each side of the non-union until the underlying trabecular bone is exposed, without removing to avoid compromising the integrity of the fragments.
Twenty-five-year-old male operated six months after a fracture of the scaphoid waist. Left non-dominant hand. The focus is debrided with a synoviotome and a motorized burr (a). The graft is introduced into an arthroscopy sheath (4mm) (b). The graft is compressed and deposited by penetrating the obturator into the sheath (c). Exposed bone graft at the focus (d).
After this, the lunate bone was internally fixed in neutral alignment with a Kirschner wire from the distal radius to the lunate bone, which stabilized the carpus. In the 5 cases with DISI (dorsal intercalated segment instability) that form part of our study, this deformity was corrected by flexing the wrist before introducing the wire. Sometimes intraoperative radiography alone is not sufficient to determine fixation; therefore, it must be confirmed arthroscopically.
The graft was introduced into a wrist arthroscopy sheath (4mm) (Fig. 2b), compressed, and deposited by penetrating the obturator into the sheath through the midcarpal portals in previously debrided and prepared non-union (Fig. 2c). The exposed bone graft on the midcarpal surface of the scaphoid was subsequently covered with fibrin glue (Fig. 2d).
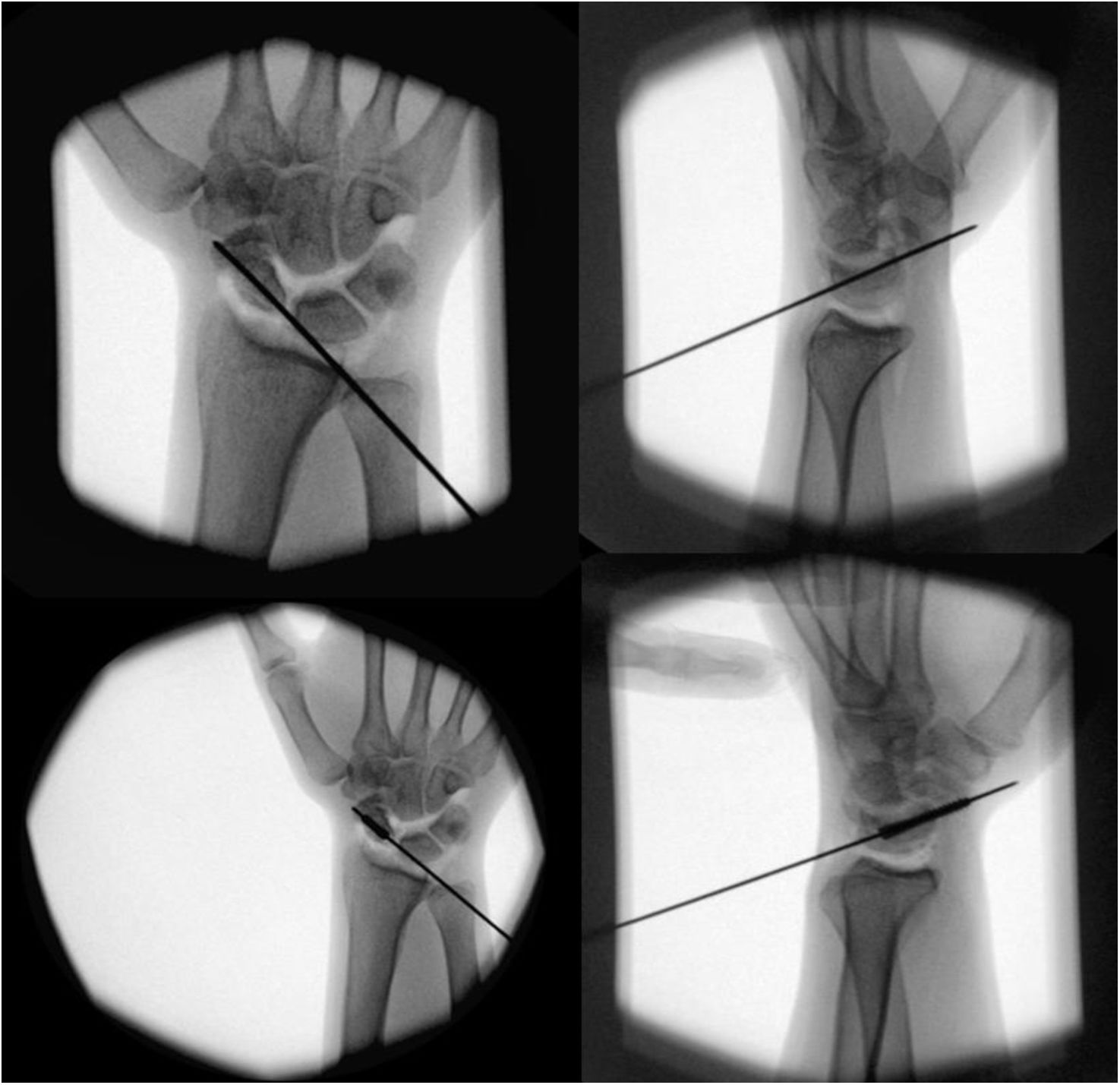
Finally, through the 3–4 portal, the scaphoid is fixed with a cannulated screw after introducing the guide wire and confirming its correct position radiologically and arthroscopically. To facilitate insertion, traction is released, and the wrist is positioned in maximal flexion. Once the guide wire and screw are positioned, traction is briefly reapplied only for fluoroscopic confirmation and documentation. Fig. 3 corresponds to this moment.
A 37-year-old male operated on 9 months after a scaphoid fracture. Dominant right hand. Placement of the cannulated screw through its guide wire. Although insertion was performed without traction and with the wrist in flexion, traction was briefly reapplied to document the position under fluoroscopy, explaining the radiocarpal and midcarpal distraction visible in the image.
Sometimes a volar percutaneous approach can be performed for retrograde screw insertion, because dorsal approach might be technically difficult. In our series, the volar approach was used for some scaphoid waist non-union with a viable proximal pole. Retrograde fixation was also used for the three cases with humpback deformity, preceded by its correction by positioning the wrist in hyperextension after lunate fixation in a neutral position with a radiolunate wire. Those cases of non-union of the proximal pole were performed dorsally, through the 3–4 portal, with anterograde screw placement. In this series, 24 anterograde screws and 7 retrograde screws were placed.
The screw length and the stability of the non-union line were determined by exploration and arthroscopic visualization. After graft placement, the gap between fragments measured with a depth gauge was always less than 1mm, so it did not affect screw measurement. In 29 patients, a 2.4mm Acutrak Mini screw (Acumed, Hillsborough, Oregon, USA) was used, and in two of them, a 3mm Cannulated Compression Screws (Medartis Co, Austrase 24, 4051 Basel, Switzerland) was used. Finally, the correct placement of the fixation and bone graft was verified with intraoperative radiographs. Sometimes, intraoperative fluoroscopy alone is not sufficient to determine fixation; therefore, we use both arthroscopy and fluoroscopy in all patients to ensure proper fixation.
In our series, eight patients presented a stage I SNAC pattern. Arthroscopic radial styloidectomy was performed on these patients, which proved useful in reducing pain caused by these degenerative changes.
After four weeks of immobilization with a dorsal forearm splint, patients began a supervised rehabilitation protocol. This included progressive range-of-motion exercises of the wrist, proprioceptive training, and gradual strengthening under the supervision of a rehabilitation physician. Weight-bearing and impact activities were restricted until 8 weeks postoperatively. Patients were encouraged to return progressively to their occupational and sports activities from the third postoperative month, according to their tolerance and radiological evidence of union.
Statistical analysisStatistical analysis was performed using descriptive methods. Continuous variables (VAS pain, grip strength, range of motion, Quick DASH) were expressed as mean, range, and 95% confidence intervals. Categorical variables (return to work and sport) were expressed as frequencies and percentages. Statistical analysis of the data was performed using Student's t-test for paired samples. A p-value <0.05 was considered to be statistically significant.
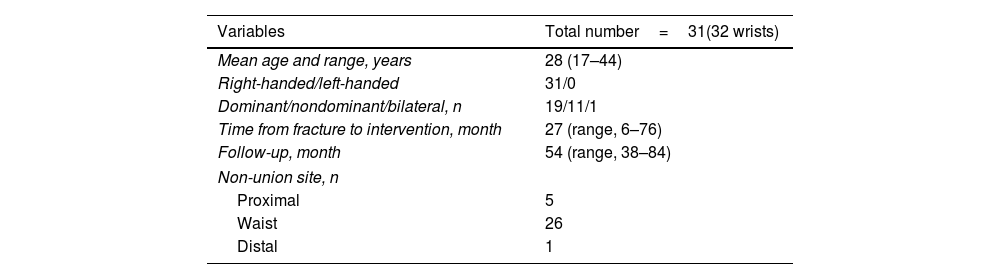
ResultsThe study included 31 patients (32 wrists): 27 men and 4 women. The mean follow-up period for the sample was 54 months (range, 38–84), with a minimum follow-up of three years. Demographic and non-union site data are shown in Table 1.
Demographic data of study patients.
| Variables | Total number=31(32 wrists) |
|---|---|
| Mean age and range, years | 28 (17–44) |
| Right-handed/left-handed | 31/0 |
| Dominant/nondominant/bilateral, n | 19/11/1 |
| Time from fracture to intervention, month | 27 (range, 6–76) |
| Follow-up, month | 54 (range, 38–84) |
| Non-union site, n | |
| Proximal | 5 |
| Waist | 26 |
| Distal | 1 |
The average ischemia time was 75min. Of the total, 11 non-unions were in the non-dominant hand, 19 in the dominant hand, and 1 bilaterally. Regarding the fracture pattern (before non-union), 26 fractures were of the scaphoid waist, 5 of the proximal third and 1 of the distal third. All the non-unions corresponded to subtype D2 of the Herbert and Fisher classification.8 Moreover, in the radiological evaluation before surgery, 8 cases of SNAC I and 3 humpback deformities with an average angle of 75° were observed.
Radiological consolidation was achieved in 100% of cases at 12 weeks post-intervention, with a mean time of 10 weeks (range, 8–12), regardless of the time elapsed before surgery, the type of non-union, or smoking habit (four patients were smokers with an average of half a pack per day). No complications were observed in any of the 31 patients.
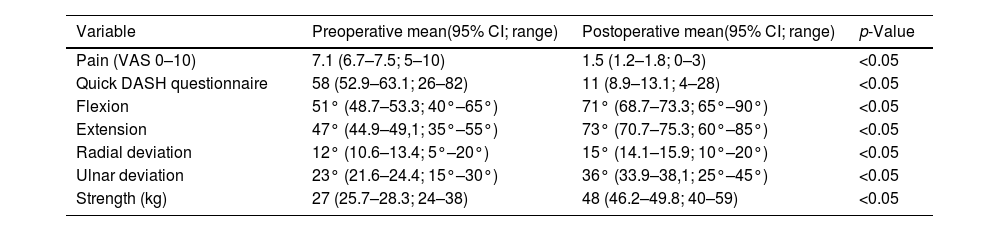
Pain on the VAS, grip strength, Quick DASH score and range of motion improved as shown in Table 2. All comparisons between preoperative and postoperative values (VAS, Quick DASH, grip strength, and range of motion) showed statistically significant improvements (p<0.05).
Clinical and radiological results of the 31 patients after being operated of scaphoid non-union through arthroscopy.
| Variable | Preoperative mean(95% CI; range) | Postoperative mean(95% CI; range) | p-Value |
|---|---|---|---|
| Pain (VAS 0–10) | 7.1 (6.7–7.5; 5–10) | 1.5 (1.2–1.8; 0–3) | <0.05 |
| Quick DASH questionnaire | 58 (52.9–63.1; 26–82) | 11 (8.9–13.1; 4–28) | <0.05 |
| Flexion | 51° (48.7–53.3; 40°–65°) | 71° (68.7–73.3; 65°–90°) | <0.05 |
| Extension | 47° (44.9–49,1; 35°–55°) | 73° (70.7–75.3; 60°–85°) | <0.05 |
| Radial deviation | 12° (10.6–13.4; 5°–20°) | 15° (14.1–15.9; 10°–20°) | <0.05 |
| Ulnar deviation | 23° (21.6–24.4; 15°–30°) | 36° (33.9–38,1; 25°–45°) | <0.05 |
| Strength (kg) | 27 (25.7–28.3; 24–38) | 48 (46.2–49.8; 40–59) | <0.05 |
VAS: Visual Analogue Scale; DASH: Disabilities of the Arm, Shoulder, and Hand; CI: confidence interval.
Before the scaphoid fracture, 26 individuals (84%) regularly engaged in high-demand sports activities, while five led sedentary lifestyles. After surgery, among those who were involved in sports, 19 (61%) continued without limitations, while seven (23%) stopped; four (13%) due to reasons unrelated to the fracture, another two (6%) due to persistent discomfort (a football goalkeeper and a handball player), and one (3%) due to insecurity despite having no pain or stiffness. Regarding occupational activity, 100% of the patients were engaged in manual labor before the fracture. After surgery, all of them have returned to their respective jobs without limitations, except for one patient, who has a slight limitation in lifting weights (cleaning service worker).
DiscussionThere are several options for treating scaphoid non-unions. However, there are fundamental common requirements for successful treatment. Among these, it should be highlighted the maintenance of blood supply, debridement of non-union area, fracture reduction, adequate bone grafting, and proper internal fixation.14,15
Minimally invasive techniques such as arthroscopy have become increasingly important in the treatment of these types of injuries. In the absence of solid evidence supporting the use of a specific technique for the best treatment of scaphoid non-unions, minimally invasive approaches via arthroscopy cause less morbidity for the patient, minimizing postoperative stiffness and maximizing functional outcomes.5 Although Oh et al.16 did not find statistically significant differences in clinical outcomes when retrospectively comparing two groups of patients treated arthroscopically versus open surgery, it is logical to assume that open approaches entail greater damage to surrounding tissues.
Open procedures may damage the limited blood supply of the scaphoid, which would worsen the condition of the already poorly vascularized proximal pole.17 Additionally, conventional open approaches traverse the areas where the palmar radiocarpal ligaments of the wrist run, as well as the joint capsules where the mechanoreceptors responsible for wrist proprioception are located, potentially damaging them and affecting wrist neuromuscular control.18 Another advantage of arthroscopy is its greater effectiveness in confirming fracture reduction compared to isolated intraoperative fluoroscopy. Additionally, it provides the possibility of assessing other associated injuries.17,19
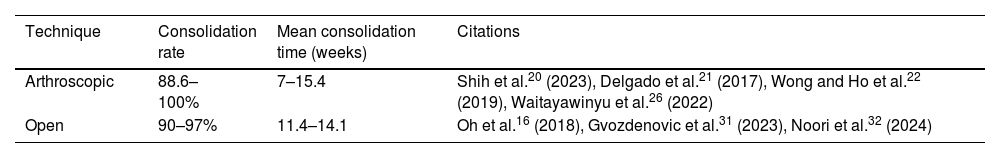
Recent studies confirm that arthroscopic outcomes are comparable to those of conventional open surgery, as shown in Table 3. Shih et al.20 reported a consolidation rate of 88.6% in 44 patients with a minimum follow-up of two years treated with arthroscopic osteosynthesis and cancellous bone grafting. Delgado et al.21 described 13 patients treated with cancellous bone graft and internal fixation with a cannulated screw, achieving 100% consolidation in a mean of seven weeks. Wong and Ho22 also reported favorable outcomes, with an overall union rate of 90.3% in their review.
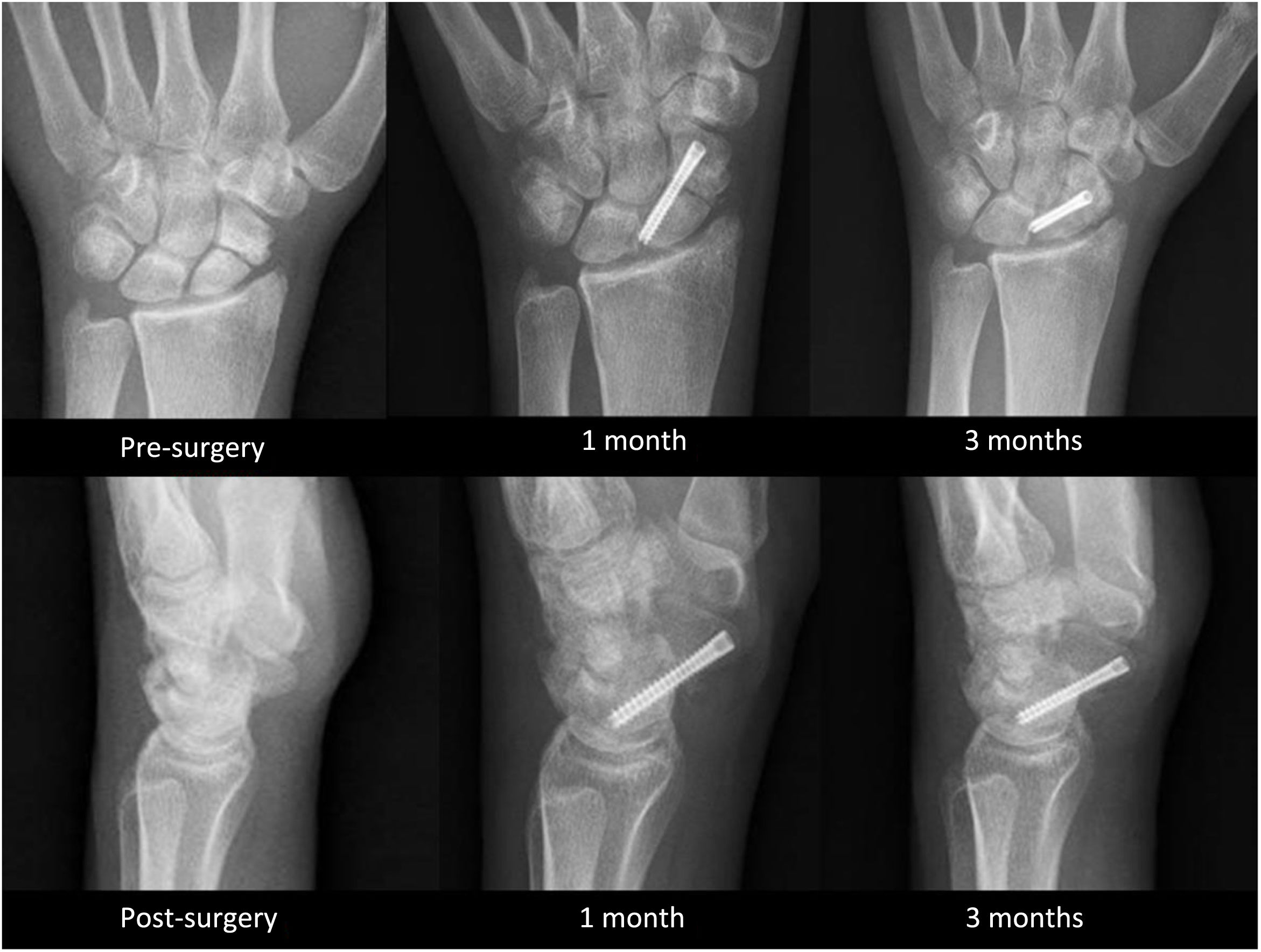
In our series, all patients achieved complete bone consolidation with satisfactory radiological and clinical results (Figs. 4 and 5). Of note, the mean consolidation time was 10 weeks, similar to Delgado's findings, and shorter than in most other published series. Furthermore, our study provides the longest follow-up of arthroscopically treated scaphoid non-unions reported to date. A comparison with recent studies is summarized in Table 4.
Comparison of the results obtained in recent studies in which scaphoid non-unions were treated with osteosynthesis assisted by arthroscopy.
| Study and year of publication | Specific details | Type of study | Level of evidence | Patients (n) | Union rate |
|---|---|---|---|---|---|
| Cognet et al.2 (2016) | Author's first 23 cases | Case series. Follow-up: 17 months | IV | 23 | 23/23 at 4 months |
| Delgado et al.21 (2017) | Author's first 13 cases | Case series. Follow-up: 17 months | IV | 13 | 13/13 at 7 weeks |
| Wong et al.22 (2019) | Arthroscopic cancellous bone graft | Case series. Follow-up: 34 months | IV | 125 | 112/125 at 14 weeks |
| Waitayawinyu et al.26 (2022) | Olecranon bone graft | Case series. Follow-up: 32 months | IV | 22 | 22/22 at 15 weeks |
| Ecker et al.23 (2022) | Proximal pole non-unions | Case series. Follow-up: non-reported | IV | 30 | 29/30 at 3 months |
| Wu et al.24 (2022) | Proximal pole non-unions | Case series. Follow-up: 31 months | IV | 20 | 20/20 at 14 weeks |
| Shih et al.20 (2023) | Non-unions stages I–III | Case series. Follow-up: 33 months | IV | 44 | 39/44 at 15 weeks |
Regarding internal fixation, Ecker et al.23 used three Kirschner wires to internally fixate the scaphoid and bone graft, achieving consolidation in 29 out of 30 treated patients (96.7%). They chose not to use headless compression screws because they can fracture the proximal pole and fail to achieve mechanically stable fixation in cases with a small proximal fragment. Kirschner wires are less likely to damage the proximal pole and can also control its rotation. In our experience with compression screws, we had no cases of fractures of the proximal fragment. However, comparative studies of both fixation methods would be necessary to draw more precise conclusions.
In our study, the bone graft was obtained from the iliac crest due to its ease of access and because it could be obtained simultaneously while the scaphoid was being prepared. Multiple studies in the literature use this location for graft extraction.22–24 However, other studies argue that bone harvested from the iliac crest is not superior to that harvested from the distal radius.25 Cognet et al.2 in a study treating 23 patients with scaphoid non-unions, did not resort to iliac bone grafting. Instead, they used bone grafts from the dorsal aspect of the radius and olecranon, with good results. Recently, Waitayawinyu et al.26 also published satisfactory results with arthroscopic treatment using olecranon bone grafts, achieving complete consolidation in all 22 patients that form part of study with an average union time of 15.3 weeks.
One of the limitations of the arthroscopic approach appears to be the restoration of carpal radiographic alignment. Slade and Dodds27 recommended open structural grafting for non-unions with poor scaphoid alignment. Oh et al.16 and Kim et al.28 also concluded that arthroscopic grafting had more limitations in restoring normal carpal alignment; however, they did not find statistically significant differences in clinical outcomes at a short-term follow-up. Both agree that arthroscopic reduction has positive effects on wrist clinical function recovery. In contrast to these articles, Wu et al.24 and Wong and Ho22 argue that correct arthroscopic technique with cancellous bone grafting can sufficiently correct scaphoid and carpal malalignment, making open reduction unnecessary. Hsiung et al.29 have also demonstrated that arthroscopic realignment achieves good clinical and radiographic results.
Comparatively, the systematic review by Santoshi et al. suggests that arthroscopic techniques achieve union rates at least equivalent to those of open (non-vascularized and vascularized) bone grafting, with a potentially lower morbidity profile and faster recovery.3 Nevertheless, possible selection biases remain (e.g., preferential use of open vascularized grafts for cases with avascular necrosis or ‘humpback’ deformity) previously noted in the arthroscopic literature, limiting direct comparisons.30 Overall, our findings are consistent with this body of evidence: the arthroscopic technique emerges as a highly effective, minimally invasive alternative for selected non-unions, but definitive confirmation of its superiority (or cost-effectiveness) over open approaches will require controlled trials and prospective studies stratified by avascular necrosis, deformity, and standardized radiological criteria.3,30
Although no complications occurred in the present series, wrist arthroscopy and iliac crest graft harvesting are not risk-free. Portal-related neuropraxia, transient dorsal branch of the ulnar and radial nerves irritation, superficial infection, and iatrogenic chondral scuffing have been described at low rates in the literature. Donor-site morbidity at the iliac crest may include local pain and hematoma and rare lateral femoral cutaneous nerve neurapraxia.3,22,30
This study has some limitations. Firstly, we lack a control group of patients treated by an open approach to compare clinical and radiological outcomes. Secondly, the number of patients studied is not very large, although it is comparable to the reviewed studies on arthroscopic treatment in scaphoid non-unions. Thirdly, radiological consolidation was primarily assessed with plain radiographs, and postoperative CT was only used in selected cases, which may overestimate the union rate. Moreover, our cohort predominantly comprised young adults with few adverse prognostic factors (mean age 28 years; only four light smokers), which likely contributed to the favorable biology and rapid union observed. Therefore, external validity to older patients, heavy smokers, or those with metabolic bone disease and proximal pole AVN is limited. Results should not be over-generalized to these high-risk groups.
ConclusionsArthroscopy-assisted osteosynthesis with percutaneous compression screw and cancellous bone grafting has proven to be a viable and minimally invasive method for treating scaphoid non-unions, including cases with early-stage SNAC wrist and those with humpback deformity. Additionally, this technique leads to high consolidation rate and good clinical results with a short recovery period.
The results of this study are truly promising, but the limitations previously discussed may limit the generalization of our results.
Level of evidenceLevel of evidence IV.
Ethics approval and consent to participateApproval was granted by the Ethics Committee of Institutional Review Board of the 12 de Octubre Hospital, Madrid, Spain. Informed consent was obtained from all individual participants written included in the study.
Consent for publicationThe authors affirm that all research participants provided informed consent for publication of the clinical data and images in Figs. 1–5 with removing any identifying personal information.
FundingNo funding was received for this study. The authors received no funding for this publication.
Conflict of interestEach author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.