Translation and validation of the risk assessment and prediction tool (RAPT) into Spanish to assess the discharge needs of patients after total hip arthroplasty.
MethodologyThe original RAPT instrument was translated into Spanish following the guidelines of Sousa and Rojjanasrirat, 2011. To carry out the cross-cultural adaptation of the instrument to Spanish, the translation method of Guillermin et al., 1993 was used.
ResultsOne hundred and thirty-four patients were included. The mean age was 71.6 years. Of the patients analyzed in the study, the tool detected that 57.8% required home rehabilitation, 28.9% would be discharged home and 13.3% would require an assessment from the social worker to go to a social health center. The content validity index (CVI) for the entire scale was 0.91. Cronbach's alpha was 0.84.
ConclusionsThe RAPT tool has been shown to be highly effective in assessing patients’ needs upon discharge. According to the results of the study, 94.2% of the needs identified by the tool coincided with the real needs of the patients. This suggests that the tool may be an efective tool for planning post-discharge care.
Traducción y validación de la herramienta de evaluación y predicción de riesgos (RAPT) al español para evaluar de las necesidades al alta de los pacientes después de una artroplastia total de cadera.
MetodologíaEl instrumento original RAPT fue traducido al español siguiendo las directrices de Sousa y Rojjanasrirat 2011. Para realizar la adaptación transcultural del instrumento al idioma español se utilizó el método de traducción de Guillermin et al., 1993.
ResultadosSe incluyeron 134 pacientes. La edad media era de 71,6 años. De los pacientes analizados en el estudio la herramienta detectó que un 57,8% requería rehabilitación a domicilio, un 28,9% se iría de alta a su domicilio y un 13,3% requeriría valoración de la trabajadora social para ir a un centro sociosanitario. El índice de validez de contenido para toda la escala fue 0,91. El alfa de Cronbach fue de 0,84.
ConclusionesLa herramienta RAPT ha demostrado ser altamente efectiva en la evaluación de las necesidades de los pacientes al alta. Según los resultados del estudio, el 94,2% de las necesidades identificadas por la herramienta coincidían con las necesidades reales de los pacientes. Esto sugiere que la herramienta puede ser eficaz para la planificación de la atención postalta.
Millions of people worldwide suffer from osteoarthritis,1 which impacts their quality of life.2 The factors that trigger the process are unknown, and it is believed to be the result of a combination of genetic and environmental factors. The main symptom of hip osteoarthritis is pain, which is primarily located in the groin area. Currently, there is no cure for osteoarthritis, nor are there proven treatments to delay the progression of the disease. The goal of treatments is therefore to alleviate the joint pain and physical disability it causes in patients.3 Osteoarthritis is a global health priority given its high prevalence. It affects more than 50% of patients over 60 years of age, and given the progressive ageing of the population and the increase in diseases related to its aetiopathogenesis (obesity and sedentary lifestyle), the World Health Organisation estimates that more than 579 million people worldwide will suffer from it in the near future.4
Total hip arthroplasty (THA) and knee arthroplasty represent an effective alternative for the treatment and pain control of patients with osteoarthritis. The development of modern arthroplasty began in the 1950s with the Charnley low-friction arthroplasty. After decades of improvement, arthroplasty is now one of the most reliable and requested surgical procedures by patients.5
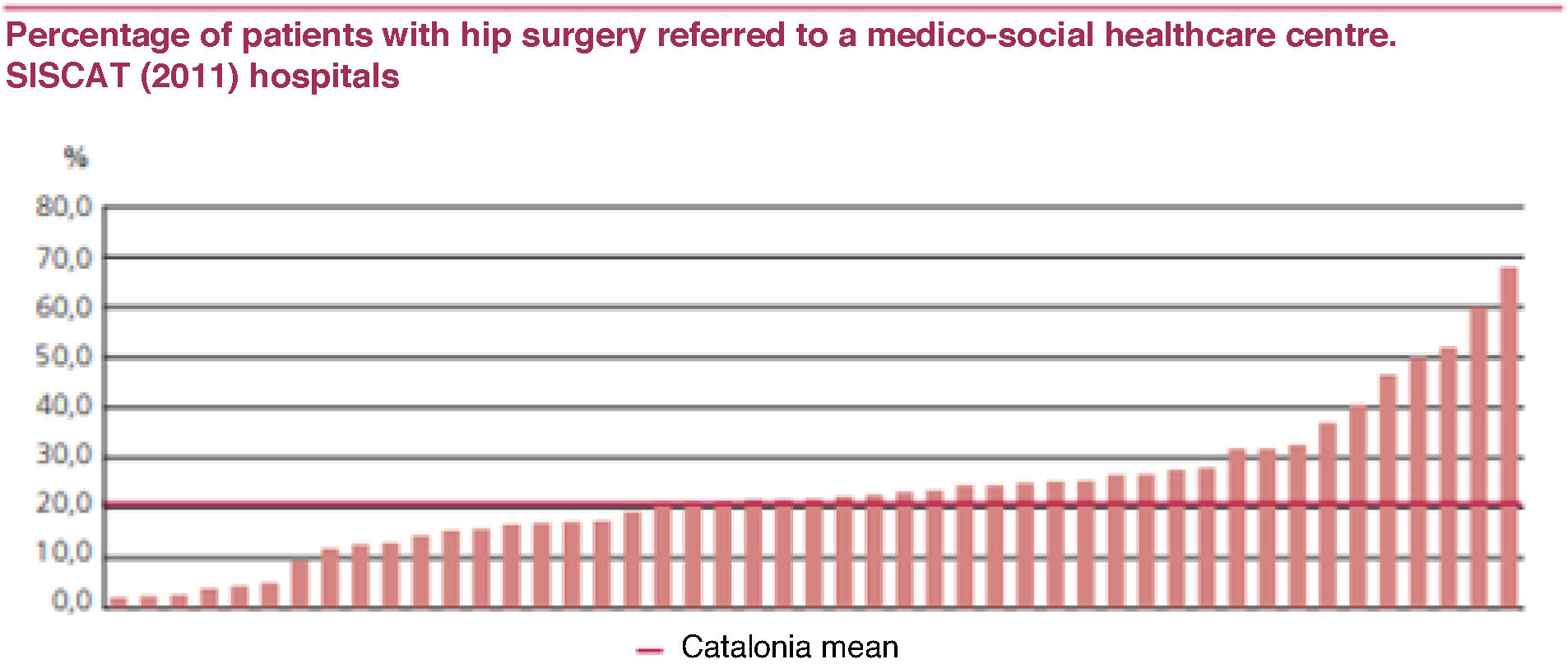
In Catalonia, 21.1% of patients who underwent total hip arthroplasty in 2011 were referred to a social-health resource, according to the data presented in Fig. 1. This percentage has increased considerably from the 9.6% recorded in 2004.6
Percentage of patients with hip surgery referred to a medico-social healthcare centre. SISCAT (2011) hospitals.
Source: Gencat.6
The care system for dependent elderly people in Catalonia is characterised by a predominance of family-provided care. This is due to the moderate development of residential care and the limited development of home care. People receiving some home care account for 1.3% of the population over 65 years of age, and those cared for in a residential care environment account for approximately 3.8%. This figure is half that of some of the most representative countries in the European Union, such as Germany and France, representing a significant shortage of residential care places. However, we cannot ignore the fact that the international trend is clearly giving preference to home care, and this is expected to moderate the demand for residential care places in the future.7
The risk assessment and prediction tool (RAPT) is a preoperative survey designed to predict discharge circumstances after THA.8
The RAPT was developed by Dr. Leoine Oldmeadow at the Alfred Hospital in Victoria, Australia, in 2001, to predict the fate of patients discharged after hip and knee replacement surgery. Predictions based on objective factors provide confidence in the decisions made regarding discharges by patients and the medical team.9
During its development, this tool has provided significant benefits and suffered some limitations. The most significant benefit is its potential to personalise postoperative rehabilitation, stratifying risks and optimising resources. This not only reduces hospital stays but also lowers healthcare costs by improving the organisation of healthcare resources. The RAPT helps identify patients who need more assistance after discharge.10
The six elements included in the RAPT are age, sex, preoperative walking distance, use of a walking aid, community supports, and the presence of a caregiver upon return home. The weighting of the questions varies according to their relevance in determining discharge readiness. The score assigned to each question is directly related to its correlation with this factor. A score between 1 and 12 is generated based on the patient's responses to the questions.
Patients who score less than 6 are at high risk of needing to attend a rehabilitation centre. Patients with a score between 6 and 9 are considered at intermediate risk. Finally, patients with a score above 9 are at low risk.11 Given the high prevalence and increasing number of interventions, it is important to have tools for better organisation of healthcare resources.12 The main objective of this study is to translate and validate the RAPT tool into Spanish to assess the discharge needs of patients after THA.
MethodologyThe original RAPT instrument was translated into Spanish to analyse its psychometric properties (content validity and internal consistency) following the guidelines of Sousa and Rojjanasrirat (2011).13 The original scale was translated from the original language (OL), English, to the target language (TL), Spanish, in six steps using the following process:
- 1.
Step 1: Translation. The RAPT tool was translated from the OL to the TL by two groups, each composed of two independent translators. One group consisted of a native Canadian translator-interpreter and a native English translator, both unfamiliar with the subject matter, and the other group consisted of two Spanish-born English translator-interpreters familiar with the subject matter. A joint discussion was then held to identify errors.
- 2.
Step 2: Fusion of the two versions. The first translation was completed by two groups of translators, each composed of two people. After discussing and resolving discrepancies with the first two groups, the manuscript was sent to a third reviewer, who was responsible for combining the two versions into a single one. At this stage, the research team, along with the principal investigator, collaborated in the discrepancy resolution process.
- 3.
Step 3: Back-translation. Two independent bilingual translators, both English philologists, each performed a completely blind translation from the original document from the IO to the ID. This produced two different documents.
- 4.
Step 4: Differences between the two back-translations. Once the previous processes were completed, a group of 20 subject matter experts was convened to compare the versions. The equivalence of content, structure, and semantics was analysed. There were some differences in cultural meaning, but these were resolved by consensus within the translation team. For example, the block length in Canada (the scale's original city) is 200m, but in Barcelona it is 300m, so this aspect was specified in the final document. We then compared the final document with the original document, and there were no significant differences.
- 5.
Step 5: First pilot test. Ten non-expert participants (two medical specialists, two nurses, two physical therapists, two occupational therapists, and two social workers) were randomly recruited to analyse content, semantic, and conceptual equivalence. Each participant was asked to rate whether each item was clear and easy to understand and to offer suggestions on how to rewrite them to make them clearer. The entire group of selected participants determined that the items were clear and concise.
- 6.
Step 6: Expert evaluation panel (evaluation of item clarity). The research team evaluated the document to determine its clarity and appropriateness for our context. To calculate the instrument's content validity, eight nurses, a nursing coordinator, and an orthopedic surgeon formed the expert panel to evaluate each item from 1=not relevant to 4=very relevant. The content validity index (CVI) for each item on the scale was the number of experts who rated each item as 3 or 4.14
- 7.
Step 7: Second pilot test. The instrument's comprehensibility and clarity were assessed. After the entire process, the version was ready for psychometric testing with the target population. In this phase, the scale's clarity and well-written design were assessed, ensuring it did not lead to misinterpretation. A random sample of 35 hospitalised patients was sufficient for this phase. The individuals were randomly selected and were not experts in the field. The entire group of people selected determined that the items were clear and concise, so it was not necessary to adjust any of them.
The study sample included 133 patients undergoing total hip replacement surgery at our centre. Participation was voluntary prior to completing the survey. Patients signed an informed consent form specifying that participation was voluntary and anonymous. The inclusion criteria for participants were: patients over 18 years of age who were literate and understood spoken and written Spanish, and patients undergoing THA. Exclusion criteria included patients undergoing hip replacement arthroplasty and patients who refused to participate in the study. To calculate the appropriate sample, we followed the recommendation of Sousa and Rojjanasrirat,14 who indicated that for the general psychometric analysis, a sample of 10 subjects per item of the instrument was required, and since the RAPT instrument has 6 items, a minimum sample of 60 patients was required. Initially, 180 patients were invited to participate, expecting a 50% response rate. Ultimately,128 patients participated, achieving a response rate of 71.11%.
Data analysisData were collected from October 2021 to July 2022. Data analysis was performed using The Jamovi Project (2022 version 2.3) (Computer software, retrieved from: https://www.jamovi.org) and Microsoft Excel. Descriptive statistical analysis was performed to analyse the demographic characteristics of the participants. Cronbach's alpha was used to analyse the instrument's properties, which measures the homogeneity and consistency of the survey statements. A Cronbach's alpha of >.7 indicated good internal consistency.15
Ethical considerationsThe study was approved by our centre's Ethics and Research Committee (registration number: HCB/2021/1153). Patients received oral and written information at the time of signing the informed consent (IC), which meets the criteria defined in the LOPD 3/2018. They were also informed of their right to access, rectify, erase, or object. Before completing the survey, all participants were informed of the study purpose and the confidentiality of their participation. This study was conducted in accordance with the Declaration of Helsinki, good clinical practice principles, and the Universal Declaration of Human Rights. It complies with current regulations at both European and Spanish levels (Regulation [EU] No. 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC [General Data Protection Regulation]. Organic Law 3/2018 of 5 December on the protection of personal data and the guarantee of digital rights).
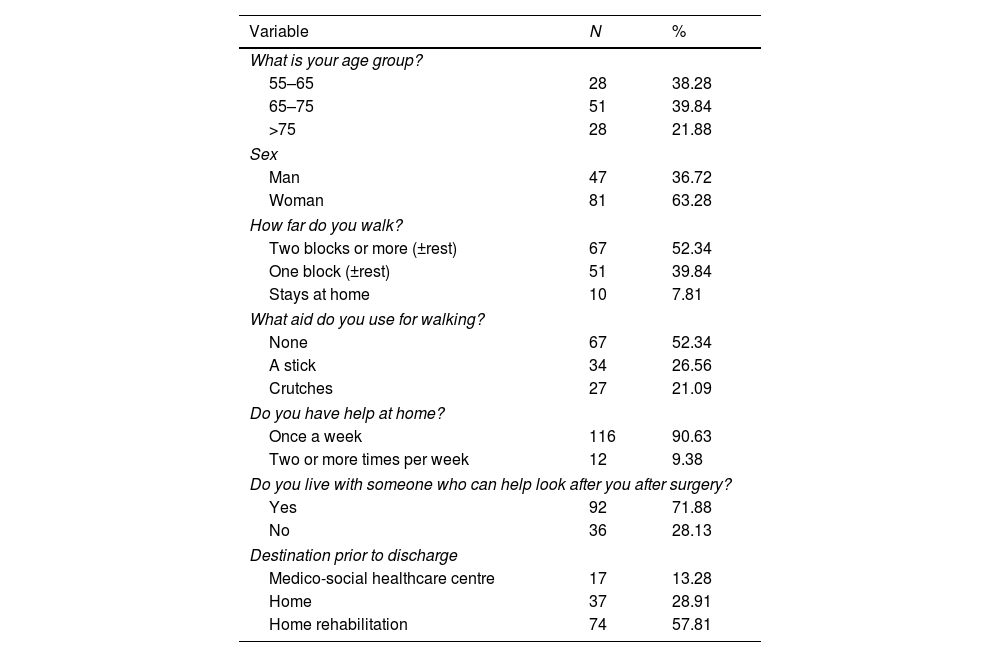
ResultsThe sample consisted of 128 participants, predominantly women (63.3%). The majority (52.3%) could walk two or more blocks before surgery, and 52.34% did not use walking aids. Regarding social support, 90.6% had help at home at least once a week, and 71.8% would be accompanied by a family member after surgery. Detailed demographic characteristics are presented in Table 1.
Sample characteristics.
| Variable | N | % |
|---|---|---|
| What is your age group? | ||
| 55–65 | 28 | 38.28 |
| 65–75 | 51 | 39.84 |
| >75 | 28 | 21.88 |
| Sex | ||
| Man | 47 | 36.72 |
| Woman | 81 | 63.28 |
| How far do you walk? | ||
| Two blocks or more (±rest) | 67 | 52.34 |
| One block (±rest) | 51 | 39.84 |
| Stays at home | 10 | 7.81 |
| What aid do you use for walking? | ||
| None | 67 | 52.34 |
| A stick | 34 | 26.56 |
| Crutches | 27 | 21.09 |
| Do you have help at home? | ||
| Once a week | 116 | 90.63 |
| Two or more times per week | 12 | 9.38 |
| Do you live with someone who can help look after you after surgery? | ||
| Yes | 92 | 71.88 |
| No | 36 | 28.13 |
| Destination prior to discharge | ||
| Medico-social healthcare centre | 17 | 13.28 |
| Home | 37 | 28.91 |
| Home rehabilitation | 74 | 57.81 |
The psychometric analysis of the scale revealed a CVI of .91, indicating excellent suitability of the items for the variable being measured. Internal consistency, assessed using Cronbach's alpha coefficient, was .84, suggesting high reliability of the scale. The result is similar to that of the original scale, thus warranting adaptation of the scale to Spanish. Regarding the predictive capacity of the RAPT tool, a 94.2% concordance was observed between predictions and actual outcomes, ensuring accurate predictions at patient discharge. Fifty-seven point eight per cent of patients required home rehabilitation, 28.9% were discharged immediately, and the remaining 13.3% required a social assessment. After this assessment, only 5.8% ultimately required a social healthcare centre.
DiscussionIn this study, we conducted an exhaustive process of translation, validation, and cultural adaptation of the RAPT prediction tool into Spanish, with the specific objective of applying it in the clinical context of our centre. The main purpose of this adaptation is to accurately and promptly anticipate the most appropriate discharge destination for patients undergoing hip replacement surgery.
Our results demonstrate that the RAPT tool, in its Spanish version, maintains the validity and reliability demonstrated in previous studies. It has been confirmed as an effective preoperative tool for identifying the specific needs of each patient at the time of discharge. This makes it possible to optimise postoperative care planning and ensure a smoother transition of the patient to the community setting or to an alternative level of care, if necessary, as well as optimise healthcare resources.
The tool has good psychometric properties: the CVI was .91 and the Cronbach's alpha for the entire instrument was .84,15,16 confirming the scale's good validation and stability in Spanish. The RAPT has also been adapted to Italian and French, presenting similar psychometric properties.17,18
The RAPT assesses a series of risk factors associated with the need for prolonged rehabilitation after arthroplasty, classifying patients into three risk categories. The tool has demonstrated high accuracy in identifying those patients who will require postoperative care. The high accuracy obtained in Spanish (94.2%) is very similar to that reported for the original version (89%), reinforcing the robustness of this tool. By identifying these patients early, healthcare professionals can implement the necessary measures to ensure optimal recovery and prevent complications. The tool allows the care plan to be tailored to each patient's individual needs, improving the efficiency of care. It is an early identifier of the need for assessment by the social worker, facilitating social services coordination and ensuring a smooth transition to discharge.
The increasing number of knee and hip replacements (661 in 2022 and 816 in 2023),19 along with high healthcare costs, has increased the need to optimise discharge planning. At our centre, where the average postoperative stay is 24–48h, the RAPT score is presented as a key tool to streamline this process. Its implementation enables consensual discharge planning with the patient, reducing hospital stay, costs, and the risk of infection. This advance is especially relevant considering the 32.46% increase in hip surgeries in a single year at our centre. By improving the prediction of postoperative disposition, the RAPT score contributes to more efficient resource management and more patient-centred care.
ConclusionsThe RAPT represents an effective clinical tool for preoperative decision-making in patients undergoing hip arthroplasty. Its ability to quickly and accurately predict discharge destination facilitates optimised care planning, improved resource efficiency, and more personalised and patient-centreed care. Furthermore, the reduction in hospital readmissions, sometimes associated with inadequate discharge planning, improves patients’ quality of life and reduces the burden on the healthcare system.
Level of evidenceLevel of evidence III.
Eithical considerationsThe project was conducted in accordance with the World Medical Association's Code of Ethics (Declaration of Helsinki), and informed consent was obtained from the patients. The project was approved by the hospital's ethics committee.
FundingThis research project did not receive any funding from any private or public body.
Conflict of interestsThe authors have no conflict of interests to declare.