Guillain Barré syndrome (GBS) is an immune-mediated disorder of the peripheral nervous system characterized by acute polyradiculoneuritis. Clinically it is characterized by a sensory alteration, ascending paresis and areflexia. Sometimes, the symptoms are preceded by gastrointestinal tract infection. The diagnosis is clinical, and complementary explorations (lumbar puncture and neurophysiological study) support the diagnosis and rule out other etiologies. The primary role of magnetic resonance imaging (MRI) is not well established. We present two cases in which the MRI resulted being the key to the diagnosis.
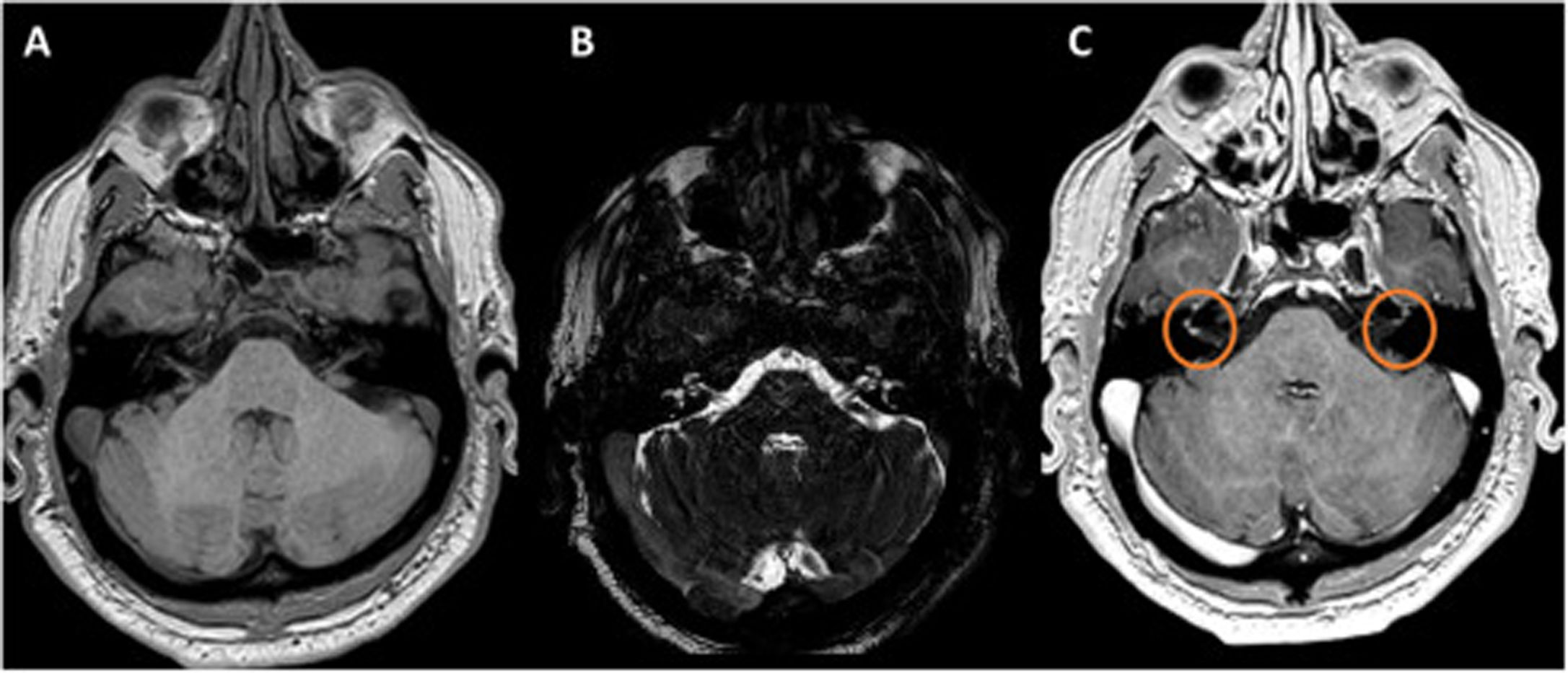
Case 1A 25-year-old man with no significant medical history, presented to the emergency room with weakness of both feet. The exploration showed distal paresis of both legs, grade 3/5, with exaggerated lower limbs osteotendinous reflexes and indifferent cutaneo-plantar reflex. The initial diagnostic suspicion was myelitis, so an MRI was performed, which showed an enhancement in conus medullaris and nerve roots (Fig. 1). A posterior lumbar puncture showed pleocytosis (8 cells/mm3) and elevated cerebrospinal fluid (CSF) protein sprain (93.00mg/dL), with negative serologies. The nerve conduction study reported prolonged F wave latency in right S1, with delayed ipsilateral sural conduction and mild S1 denervation in bilateral insertion study, all compatible with acute, sensitive polyneuropathy motor with mixed profile. The neurophysiological study realized one month later showed lower motor action potential values and signs of moderate denervation. A control study, six months after the onset of symptom, was normal. Anti-GM 1 and GM2 IgM anti-ganglioside antibodies were positive. On the basis of clinic manifestation, MRI, neurophysiological study and CSF, the final diagnosis was an acute idiopathic polyradiculoneuritis, acute motor axonal neuropathy (AMAN) variant. The patient improved with no specific treatment.
Lumbar MRI (A–C), and medullary MRI. (A) T1-weighted sequence without contrast. (B) STIR sequence. (C) T1-weighted sequence with gadolinium. (D) Medullary MRI. Left image T1 weighted sequence; right image T2-weighted sequence. The figure shows linear enhancement in conus medullaris and nerve roots (green arrow).
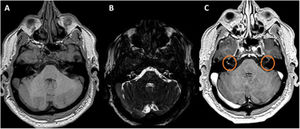
A 51-year-old male, with no relevant medical history, presented to the emergency room with bilateral facial paresis and 24-h progressive dysphagia. The neurological examination showed bilateral facial paresis with other cranial nerves and osteotendinous reflexes preserved. The lumbar puncture showed pleocytosis (13 cells/mm3, 100% mononuclear) with serologies, PCR for meningitis and CSF cultures, all negative. The study was completed with brain and cervical MRI with gadolinium, finding bilateral millimeter enhancement of both the VII and VIII cranial nerves in the internal auditory canals (Fig. 2). The anti-ganglioside antibodies (including GM1, GM2, GM3, GD1a, GD1b, GT1b and GQ1b) were negative. On the basis of the clinical manifestation, the lumbar puncture and the MRI the patient was diagnosed with acute idiopathic polyradiculoneuritis (facial diplegia variant). Finally, the patient was treated then with intravenous Immunoglobulin improving his symptoms.
DiscussionThe diagnosis of GBS is established based on clinical manifestation and physical examination. The neurophysiological studies and cerebral fluid exam are used to confirm the diagnosis and rule out other etiologies. In the first case, we suspected a transversal myelitis. The MRI showed the enhancement in conus medullari and the root nerves, but not an inflammation of the medular spine. This result was essential to guide the posterior examinations, which confirmed the diagnosis of acute idiopathic polyradiculoneuritis, AMAN variant, due to neurophysiological study and the positivity of Anti-GM1 and Anti-GM-2 antibodies. In the diagnosis of GBS the role of MRI is not well established. There are few papers that describe changes in MRI in patients with GBS.1,2 In a retrospective study of twenty-four children, Mulkey et al. discuss its importance in the differentiation of a myelitis or GBS, and how the enhancement of the lumbar nerves could be more sensitive than the neurophysiological study in early inflammation.3 In the second patient, the MRI ruled out neoplastic or infectious causes, showing an enhancement of VII and VIII cranial nerves, also compatible with an inflammation of the nerves and the final diagnosis of facial diplejia, an unusual variant of GBS.4 The MRI helped the diagnosis of GBS and this case report supports another previously described.5–7
We present images already described, but unusual in clinical practice. In our patients the MRI has been the key to the diagnosis of the pathology described. We think that it is an important exam to perform in doubtful cases or those in which the neurophysiological studies does not show abnormalities8; it should be taken into account in the diagnosis criteria.