Alcoholism and malnutrition are the main causes of Marchiafava-Bignami disease (MBD). We present a case of MBD in which poorly-controlled diabetes mellitus is suggested as the aetiopathogenic mechanism.
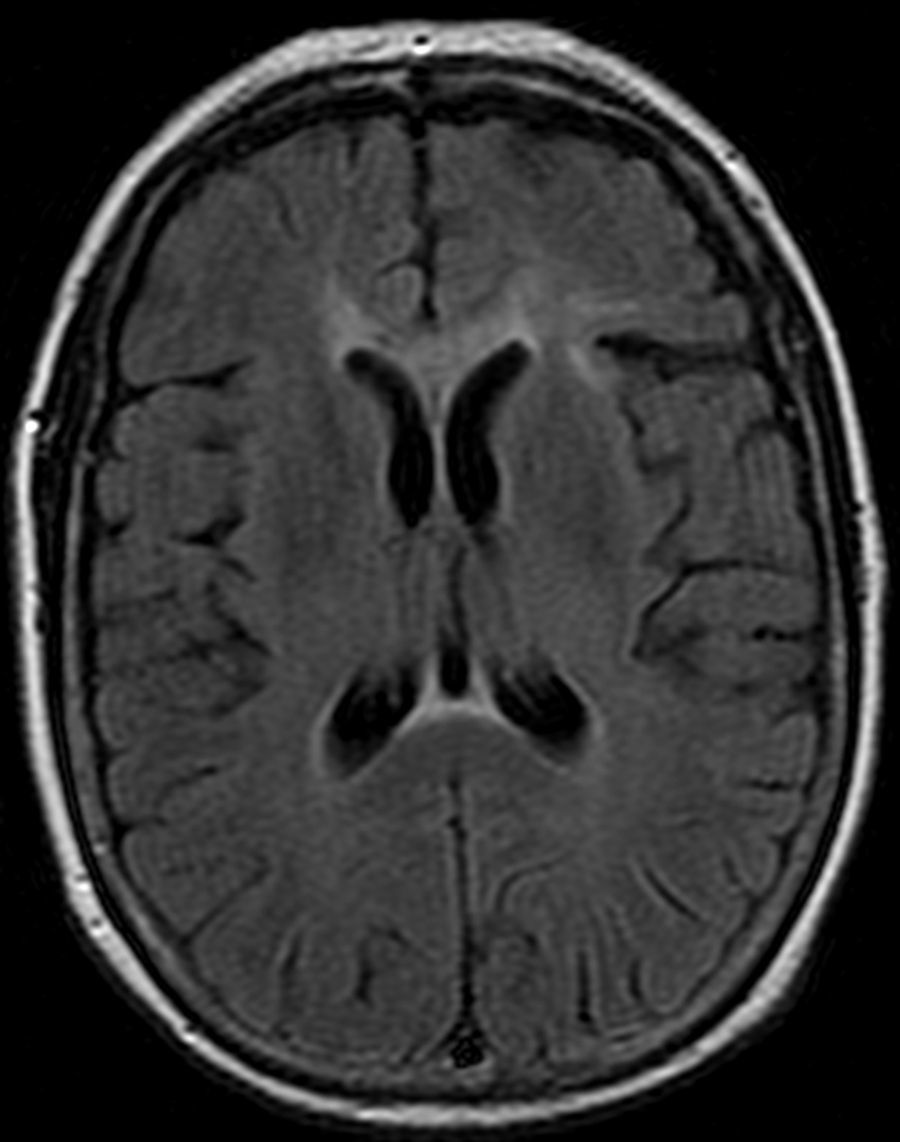
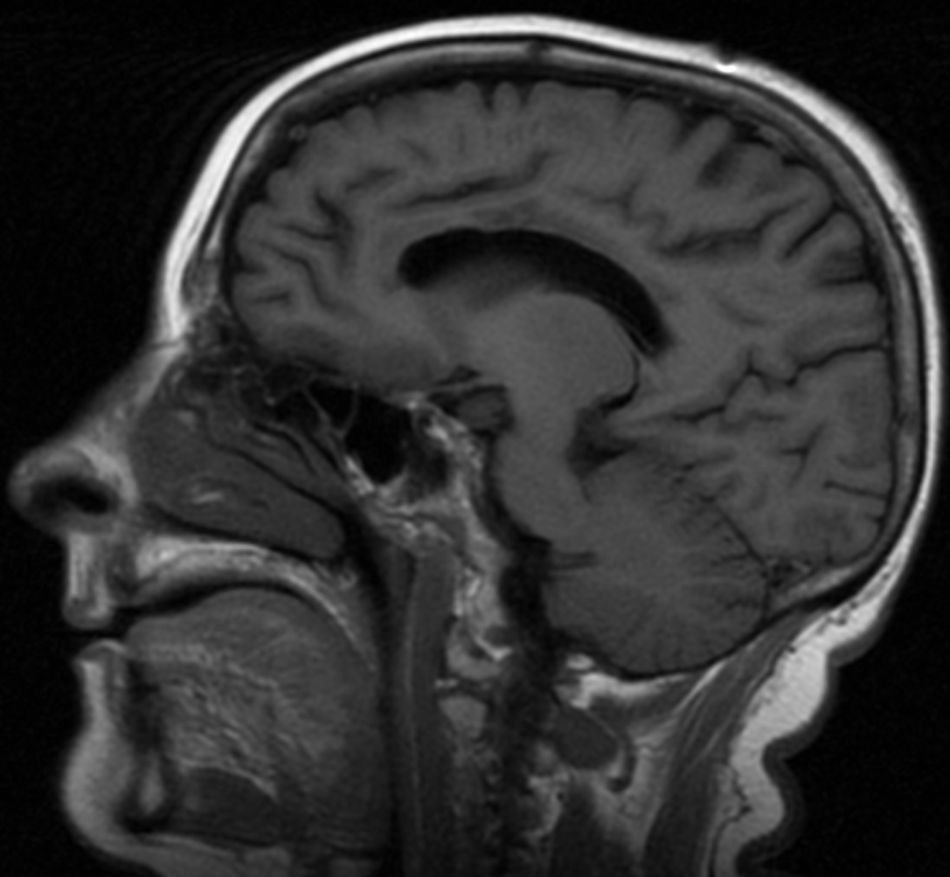
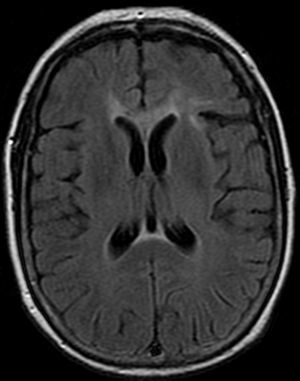
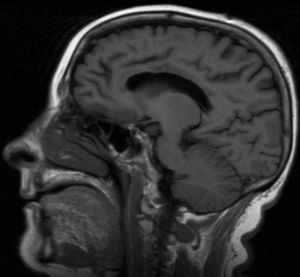
Our patient, a 57-year old diabetic woman, had been hospitalised on several occasions due to hyperglycaemic episodes, with no history of previous alcoholism or malnutrition. She was admitted due to a 1-month history of memory loss, confusion, delirium, and gait disorder. The examination revealed bradypsychia and disorientation in time, space, and person; as a sign of interhemispheric disconnection, she showed left-sided ideomotor apraxia when attempting to follow directions. Blood analysis revealed a glycaemic level of 474mg/dL and glycated haemoglobin of 11.9%. Brain magnetic resonance imaging (MRI) showed anomalies in the corpus callosum, more pronounced in its central region and appearing as hyperintensities in T2-weighted, FLAIR (Figs. 1 and 2), and diffusion sequences. The patient received treatment with intravenous thiamine (300mg/day for 3 days) followed by oral thiamine (300mg/day for 1 month), and intravenous methylprednisolone (1g/day for 5 days) followed by oral prednisone (60mg/day) in decreasing doses for 6 months. Antidiabetic treatment was readjusted. Three months after treatment, her gait and ideomotor apraxia had improved but the cognitive sequelae persisted.
MBD is an infrequent disorder first described in 1903 by 2 Italian pathologists who performed autopsies on 3 alcoholic patients with rapidly progressing symptoms of neurological impairment.1 A 2004 review article reported 250 cases of patients mostly ranging between 40 and 60 years of age, with no differences linked to ethnic group, sex, or geographical location.2 Anatomical pathology studies described necrosis and demyelination of the corpus callosum sometimes including impairment of the semioval centre and the cerebral cortex. On the microscopic level, loss of oligodendrocytes with abundant macrophages can be observed.3 The lesion mechanism may result from the direct toxic effect of alcohol or the indirect effect of electrolytic and osmotic changes, as in central pontine myelinolysis. It is thought to be linked to B12 and folate deficiencies in malnourished patients.4,5
Suzuki et al.6 and Yadala and Luo7 have recently described 2 cases of MBD in diabetic patients who were not alcoholic or malnourished. One of these studies presents a patient with no known diabetes, and therefore not being treated, whose glycated haemoglobin was 16%. The other case was a diabetic patient with glycaemia measurements ranging from 30 to 450mg/dL and with glycated haemoglobin of 8.4%. These authors suggest that osmotic changes secondary to glycaemic fluctuations constitute the pathophysiological mechanism. These descriptions match those of our patient, who had been admitted repeatedly due to hyperglycaemic episodes.
There are 2 clinical variants of MBD; the acute form manifests with rapidly progressing decline and even death, and a subacute and chronic form, seen in our case, which progresses with dementia, extrapyramidal symptoms, incontinence, difficulty walking, and signs of interhemispheric disconnection.8,9 Diagnosis is established using MRI, which shows hypointense lesions to the corpus callosum in T1-weighted sequences, and hyperintensities in T2-weighted and FLAIR sequences. Other findings include increased signal in DWI sequences and decreased signal in ADC maps, which is an early sign of MBD.10 The acute form affects the genu and the splenium, while chronic forms primarily impair the truncus. Treatment consists of ceasing alcohol consumption, taking vitamin supplements and corticosteroids, and correcting glycaemia in poorly-controlled diabetics. Steroid treatment is prescribed for potentially reversible cytotoxic oedema, which can be identified as an alteration in the DWI and ADC sequences of MRI.6 Prognosis ranges from death from acute forms to partial clinical recovery with treatment.11,12
We conclude that, in addition to classic risk factors, osmotic changes associated with glycaemic fluctuations, and possibly changes in other electrolytes or particles which alter normal blood osmotic concentration, can cause this disease. Diffusion sequence as a marker of a potentially reversible lesion can help in the selection of patients able to benefit from early steroid treatment in a context of hyperglycaemia.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez Álvarez AI, Ramón Carbajo C, Morís de la Tassa G, Pascual Gómez J. Diabetes mellitus mal controlada como desencadenante de un caso de enfermedad de Marchiafava-Bignami. Neurología. 2016;31:498–500.
Este trabajo no ha formado parte de la Reunión Anual de la SEN ni de otras reuniones o congresos.